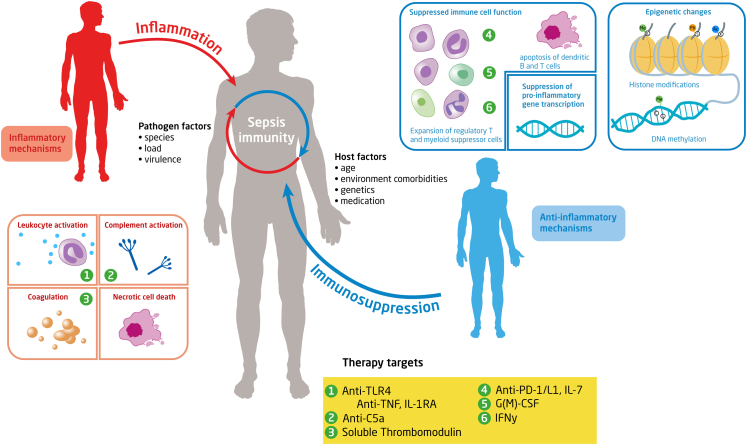
Fig. 1.
Sepsis immunity and therapeutic targets. Sepsis is characterized by the simultaneous interplay of pro- and anti-inflammatory mechanisms. The magnitude of the immune response in sepsis depends on pathogen and host related factors. The proinflammatory response is characterized by among others the release of pro-inflammatory mediators, activation of the complement and the coagulation systems and the release of alarmins by necrotic cell death. Excessive inflammation can cause collateral damage to healthy tissue. The anti-inflammatory response is characterized by impaired immune cell function due to effector cell apoptosis, T cell exhaustion, reduced monocyte HLA-DR expression, increased expression of suppressor cells and inhibition of pro-inflammatory gene transcription. Anti-inflammatory changes may relate to epigenetic changes, in particular histone modifications and alterations in DNA methylation. Histones determine the accessibility of DNA to transcription factors; histone function can be modified by acetylation (Ac), methylation (Me), and phosphorylation (Ph) of their tails. DNA methylation happens at cytosine-guanine dinucleotides (denoted by C and G). The yellow boxes indicate a selection of therapeutic targets that have been clinically evaluated as interventions in the septic immune response. Abbreviations: TLR4: Toll-like receptor-4; TNF: tumour necrosis factor; PD-1: programmed cell death protein; IL-1RA: interleukin-1 receptor antagonist; IFN: interferon; G(M)-CSF: Granulocyte macrophage-colony stimulating factor.