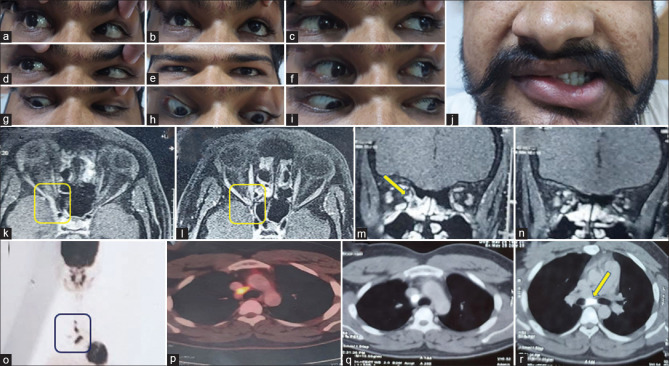
Figure 11.
A 22-year-old gentleman presented with acute onset painless horizontal binocular diplopia with no history of diurnal variation or fatiguability since 3 weeks. The next day he had also developed right-sided ptosis and had noticed that he was not able to move his right eyeball in any direction completely. History was suggestive of right-sided LMN facial palsy 2 years back with aberrant regeneration which had persisted till date. At the time of presentation, he had bilateral upper eyelid swelling more on the lateral aspect with restriction of eye movements in all directions in the right eye with pupillary sparing and right LMN facial palsy with the rest of the neurological and systemic examination being normal. Hence, evaluation was done for the syndrome of acute onset painless external ophthalmoparesis with an old history of LMN facial nerve paresis which did not reveal any evidence of neuromuscular junction disorder. Gadolinium-enhanced MRI of the brain and orbit showed an ill-defined lesion in the right cavernous sinus and orbital apex which showed mild contrast enhancement (k). The lesion was FDG avid in FDG-PET of the whole body, with FDG avid enlarged mediastinal and paratracheal lymph nodes (fig. 0-r). The possibility of sarcoidosis was kept which was further confirmed by raised serum ACE levels of 90.1 (normal values: 8–63). Endobronchial ultrasound-guided transbronchial needle aspiration showing epithelioid cell granulomas. Ziehl–Neelsen stain and Bactec culture was negative. The patient was started on oral steroids and azathioprine. He was asymptomatic at 6 months follow-up