Abstract
Background
Colonoscopies provide a crucial diagnostic and surveillance tool for inflammatory bowel disease (IBD). Accordingly, IBD patients undergo repeated and frequent colonoscopies. The oral purgative bowel prep (BP) is often burdensome on patients, resulting in delayed or missed colonoscopies due to patient noncompliance. Additionally, oral BP has been noted to possibly induce colon mucosal inflammatory changes in some patients, which may be misleading when assessing actual disease activity.
Methods
In this retrospective clinical study, we evaluated the use of an FDA cleared, defecation-inducing high-volume colon irrigation (>40 L) BP to prepare IBD patients for colonoscopy. Data were collected at 4 US Hygieacare centers from September 2016 to March 2021. The IBD patient population consisted of 314 patients that underwent 343 BPs. The BPs were prescribed by 65 physicians and performed by 16 nurses and technicians.
Results
Patient ages were 20–85 years old, 76% females, 24% males, and 97% of the patients were adequately prepared for their colonoscopy (n = 309). Patient satisfaction with the BP was very high, as reflected in postprocedure surveys and open-ended responses text analyses, and there were no serious adverse events.
Conclusions
We present data supporting that the defecation-inducing high-volume colon irrigation BP for colonoscopy is safe, effective, and preferred for IBD patients. Using this BP for IBD patients can allow earlier interventions, significantly impacting disease management and future outcomes.
Keywords: IBD, colonoscopy, bowel prep
Introduction
Colonoscopies provide a crucial diagnostic tool for inflammatory bowel disorder (IBD) since they deliver clear, detailed views of the gastrointestinal tract. The term IBD usually includes ulcerative colitis (UC) and Crohn’s disease (CD). Patients with IBD are at increased risk of developing colorectal cancer (CRC), the third most common malignancy globally and the second most common cause of cancer deaths in the United States.1 Recognizably, IBD increases CRC risk by 2- to 5-fold, accounting for 10%–15% of IBD deaths.2–8 The American Gastroenterologist Association (AGA), the American College of Gastroenterology (ACG), and other international gastroenterology associations have recommended that IBD patients, starting from 10 years after diagnosis, undergo surveillance colonoscopies every 1–3 years.9–11 Patient adherence to the recommended surveillance frequency is directly linked to their probability of developing CRC,5,12 yet compliance is estimated to be only 50%–75%.13,14
High-quality bowel preparation (BP) is crucial for both clear colonic mucosa visualization and the diagnosis and surveillance of IBD progression and flares. However, 20%–60% of colonoscopies are associated with inadequate BPs, accounting for 20%–70% of incomplete procedures.15,16 Inadequate BP for colonoscopy is associated with increased adverse outcomes,17,18 thereby significantly affecting IBD patients.19 Colonoscopies are also used as surveillance for mucosal healing to assess long- and short-term therapeutic efficacy, postoperative follow-up, and neoplasia identification.20 When evaluating the root causes for colonoscopy noncompliance among IBD patients, the most common was difficulties with BP.14
An FDA-cleared open-system technology to purge the colon by controlled gravity-fed water infusion provides an alternative to overcome the well-established issues with the oral purgative colonoscopy BP. This BP is prescription based and performed by highly trained personnel operating under stringent standard operating procedures (SOPs). The method has proved safe, effective, and well tolerated in patients, with a 97% adequacy in over 12 000 colonoscopy preparations.21–25 Clinical adequacy remains high even in patients with poor BP predictors such as age, male sex, and various comorbidities.21 Furthermore, the procedure has high patient satisfaction rates and fewer side effects than the standard oral purgative prep for colonoscopy.21 Here, we present a retrospective analysis of 343 BPs performed in 319 patients with IBD.
Methods
High-Volume Colon Irrigation BP
The high-volume water irrigation BP is used to purge the colon by gravity-fed water infusion before colonoscopy.22,26 This BP is FDA cleared and intended for use when medically indicated, such as before radiological or endoscopic examination. It is performed by trained personnel and under stringent SOPs. During the BP, the patients are seated on a disinfected basin, and a sterile, disposable nozzle is inserted about 1 inch into their rectum. Gravity-directed water (37–39 °C) flows into the bowel, loosening stool and allowing the patient to evacuate their colon. Water continues to flow and clean the colon until the patient is notified that the BP is completed. The BP takes approximately 1 hour and is automatically stopped if the water temperature exceeds the safe range of 37–39 °C. As a pre-BP regiment, patients were asked to follow a clear liquid diet the day before and the day of their colonoscopy (similar to instructions given for oral purgative-based BP). They were also instructed to take a stimulant laxative (bisacodyl, 2 × 5 mg) twice on the day before the BP (noon and evening) and once on the morning of their high-volume colon irrigation BP and colonoscopy. Some physicians also instructed the patients to take magnesium hydroxide (gentle laxative and antacid) 1–5 days before their BP.
Collection of Clinical Data and Demographic Information
Clinical and demographic data were collected from IBD patients at 4 centers: GI Associates (GIA)—Hygieacare Center in Jackson, MS, Ohio Gastroenterology and Liver Institute (OGI)—Hygieacare Center in Cincinnati, OH, Austin Gastro (AG)—Hygieacare Center in Austin, TX, and Hygieacare Center in Norfolk, VA, between September 2016 and March 2021. Procedures were prescribed by 65 physicians. The demographic and self-reported clinical data were collected via the patients’ responses to questionnaires. Since this is a retrospective descriptive study, in a standard FDA and unchanged cleared procedure, deidentified and with patient consent, no IRB was required. The examining physicians provided the BP’s adequacy for the colonoscopies, and the data were directly fed into the database by an endoscopy center employee.
Recording and Analysis of Adverse Events
All adverse events (AEs) that occurred during and immediately after the high-volume gravity-fed colonic lavage with induced defecation BP procedures were documented by the center’s staff. The AEs recorded included nausea, vomiting, dizziness, and abdominal cramping.
Patients’ Satisfaction Report and Free-Text Analysis
To estimate patients’ satisfaction, all patients were provided with a post-BP satisfaction survey that included 4 questions referring to the gravity-fed colonic lavage with induced defecation quality: (1) “Was the check-in welcoming and efficient?”; (2) “Were the explanations received from the staff about what to expect clear and to the point?”; (3) “Were the techs available as needed and adequate privacy kept?”; (4) “Were the prep room and system clean to their satisfaction?” The survey included an additional question regarding the patients’ preference when choosing between the colonic lavage BP and an oral purgative BP in the future. The answers to the survey questions were ranked on a scale of 0–3: definitely agree, agree, disagree, or definitely disagree. The survey responses were analyzed by counting responses in each category for each of the centers, and the results are presented per rating and satisfaction percentages.
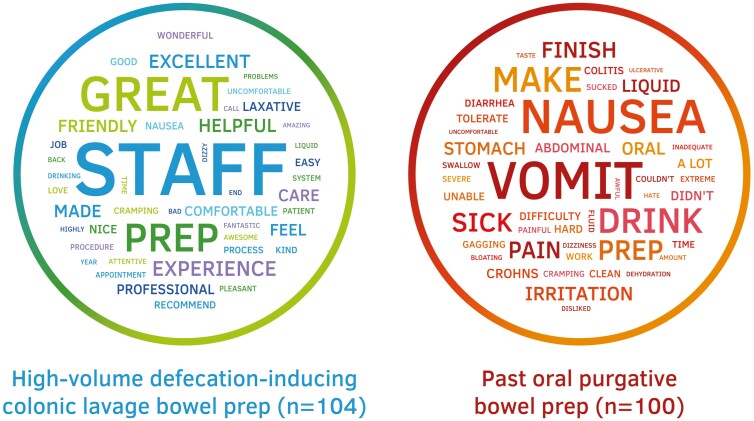
In addition, the patients were given two open-ended questions to express their opinion on the colonic lavage BP and past oral purgative BP, if applicable. Patient open-text feedback was available for 104 HygiPrep procedures and 100 past oral prep responses, gathered from all 4 sites. The patient responses were analyzed for word abundance and presented as a word cloud analysis, where the size of the words represents their relative abundance in the patients’ responses.
Results
Between September 2016 and March 2021, the gravity-fed colonic lavage with induced defecation BP for colonoscopy was performed 342 times in 318 patients suffering from IBD, as prescribed by 65 gastroenterologists. Patients’ age ranged from 20 to 85 (average = 57 ± 14), 76% of the procedures with assigned gender were performed on females and 24% on males (Table 1). Of these patients, 58% were diagnosed with UC, 33% with CD, 3% with both UC and CD, and 6% with unspecified IBD (Table 2). Out of the 342 procedures performed during this time, 309 had reported outcomes, of which 301 were deemed adequate (97%). Demographics and key results are presented in Table 1.
Table 1.
Demographics and summary of key results.
| Parameter | Summary of demographic data and key results |
|---|---|
| Procedures performed | 342 |
| Number of patients | Overall—318; patients with 1 procedure—297; patients that have had 2-to-3 procedures—21 patients (45 procedures) |
| Number of referring physicians | 65 |
| Adequacy | 97% (301/309) |
| Age of patients | min—20; max—85; average—57.5 ± 14 (n = 328) |
| Gender of patients | Male—61 (24%) Female—192 (76%) (n = 253) |
| Serious adverse events | 0 |
All patients underwent gravity-fed colonic lavage with induced defecation BP between January 2017 and March 2021. Abbreviation: BP, bowel preparation.
Table 2.
Breakdown of IBD diagnosis of 314 patients that underwent the gravity-fed colonic lavage with induced defecation BP.
| IBD indication | |
|---|---|
| Ulcerative colitis (UC) | 182 (58%) |
| Crohn’s disease (CD) | 104 (33%) |
| UC and CD | 10 (3%) |
| Unspecified IBD | 18 (6%) |
Abbreviations: BP, bowel preparation; IBD, inflammatory bowel disease.
The BP adequacy remained high (>90%) even when patients reported comorbidities considered as predictors of poor BP, such as constipation and diabetes (Table 3). The only exception was severe hemorrhoids that reduced adequacy to 89% (17/19). Prior clinical procedures, including abdominal hernia, bariatric, and GI tract surgeries, did not affect adequacy, which remained >94% (Table 4, n = 229). No severe AEs were recorded. Other AEs, defined as a patient rating of “quite a bit” or “a lot” (Table 5) included: nausea (n = 23, 7%), vomiting (n = 13, 4%), diarrhea (n = 5, 1%), and abdominal pain/cramping (n = 15, 4%).
Table 3.
Comorbidities diagnosed in 343 gravity-fed colonic lavage procedures with induced defecation BP procedures and their effect on BP adequacy.
| Comorbidity | Total number of performed procedures | Adequate BPs (% of performed BPs) |
|---|---|---|
| Constipation | 56 | 52 (93%) |
| Diabetes | 37 | 34 (92%) |
| Bladder or pelvic mesh | 18 | 17 (94%) |
| Severe hemorrhoids | 19 | 17 (89%) |
| Fissures or rectal fistula | 15 | 15 (100%) |
| Diarrhea | 10 | 9 (90%) |
| Intestinal obstruction/stricture | 12 | 12 (100%) |
| Clostridium difficile (C. Diff) | 17 | 16 (94%) |
Abbreviation: BP, bowel preparation.
Table 4.
The occurrence of prior surgeries in 343 gravity-fed colonic lavage procedures with induced defecation BP procedures and the effect on BP adequacy.
| Prior procedures | Total number of performed procedures | Adequate BPs (% of performed BP) |
|---|---|---|
| Abdominal hernia | 18 | 17 (94%) |
| Bariatric surgery | 115 | 110 (96%) |
| Colon, rectal or abdominal surgery, etc. | 97 | 93 (96%) |
Abbreviation: BP, bowel preparation.
Table 5.
Analysis of adverse events as experienced and reported by patients before and after the gravity-fed colonic lavage with induced defecation BP.
| Very little | Some | Quite a bit | A lot | None | |
|---|---|---|---|---|---|
| Nausea | 22 (6%) | 32 (9%) | 6 (2%) | 17 (5%) | 266 (78%) |
| Vomiting | 8 (2%) | 15 (4%) | 10 (3%) | 3 (1%) | 307 (89%) |
| Dizziness | 7 (2%) | 5 (1%) | 3 (1%) | 2 (1%) | 326 (95%) |
| Abdominal pain/cramping | 6 (2%) | 19 (5%) | 5 (1%) | 10 (3%) | 303 (88%) |
Abbreviation: BP, bowel preparation.
Patients were given questionnaires to assess how satisfied they were with the treatment center and the procedure itself. Patient satisfaction (on a scale of 0–3) was 2.94 for “efficient check-in” and “clear explanation regarding the procedure,” 2.96 for technician availability and room cleanliness, and 2.73 for preferring the gravity-fed colonic lavage with induced defecation technique over the traditional BP (Table 6). Analysis of the free-text analysis from the postprocedure survey provided the patients’ opinions and sentiments on the defecation-inducing colonic lavage BP (n = 104) and 100 responses on the patients’ experience with past oral purgative preps. For the colonic lavage BP, the most abundant words were “staff,” “great,” “prep,” and “experience,” all with 12–70 occurrences in 104 responses. These were followed up with the words “excellent,” “helpful,” “friendly,” “care,” “feel,” “made,” and “professional,” with 8 and 9 occurrences (Figure 1). The responses regarding past oral preps were characterized with words of different sentiment, where “vomit,” “nausea,” “drink,” and “make” were the most common words with 15–30 occurrences in 100 responses, followed by “prep,” “sick,” and “pain” with 8 and 9 occurrences (Figure 1).
Table 6.
Analysis of patient’s quality of service survey following gravity-fed colonic lavage with induced defecation BP.
| Satisfaction parameter | Score (0–3) |
|---|---|
| Efficient check-in | 2.94 ± 0.3 (n = 248) |
| Clear explanation | 2.94 ± 0.3 (n = 248) |
| Technician availability | 2.96 ± 0.3 (n = 249) |
| Room cleanliness | 2.96 ± 0.3 (n = 249) |
| Gravity-fed colonic lavage with induced defecation over traditional oral prep | 2.73 ± 0.6 (n = 240) |
Patients were asked to rate parameters on a 0–3 scale where 0 = definitely disagree, 1 = disagree, 2 = agree, 3 = definitely agree. Abbreviation: BP, bowel preparation.
Figure 1.
Word cloud analysis of free-text open-ended responses of the reported IBD population. On the left—responses from patients asked about their past experience with oral preps. On the right—responses from patients asked about their experience with the high-volume colon irrigation bowel prep. Abbreviation: IBD, inflammatory bowel disease.
Discussion
In this multicenter retrospective clinical study, high-volume gravity-fed colonic lavage with induced defecation (HygiPrep) was shown to be a well-tolerated, safe, and effective therapeutic treatment for 318 patients suffering from inflammatory bowel disease (IBD) (Table 1). In this study, 318 patients underwent 342 procedures with no severe AEs and minimal other AEs (Table 5). In addition, patients reported high levels of satisfaction (Table 4) that could translate into increased patient compliance. Physician acceptance was demonstrated by the number of physicians (n = 65) located in 4 independent endoscopy centers that referred patients (1–3 times over 4.5 years) to this prescription-only BP.
Routine colonoscopies are especially crucial for monitoring IBD patients since they are at increased risk of developing CRC.2–8 Although international guidelines recommend that IBD patients undergo colonoscopies every 1–3 years,9–11 patient adherence is estimated at only 50%–75%.13,14 Increasing compliance is crucial for improving patient quality of life and decreasing CRC occurrence and burden on the healthcare system. One factor known to reduce compliance is the burden of the pre-prep regime on patients.14 The high-volume gravity-directed colonic lavage with induced defecation presented here has shown to be safe, well tolerated, and with high patient satisfaction in 12 000 patients.25,27 Furthermore, the technology is comorbidities agnostic BP with high adequacy (97%),27 which is crucial for both IBD surveillance20 and CRC detection.17,18
It is well known that IBD is characterized by chronic inflammation of the bowel manifested by episodic or continuous intestinal symptoms such as diarrhea, abdominal pain and endoscopically by mucosal damage. Altering the natural history of the disease requires mucosal healing, and the achievement of endoscopic remission (ER) has been consistently associated with improvements in short- and long-term disease outcomes.28 ER has progressively become integrated as a primary treatment target in IBD patients, and colonoscopies are used for IBD diagnosis, assessing disease severity, disease surveillance, and adjusting treatment. Since the accurate diagnosis of IBD depends upon mucosa visualization, any procedure that can potentially disrupt the gut mucosa layer can skew diagnosis and surveillance results. Previously, it has been shown that several oral purgative-based preps, especially those containing sodium phosphate, can injure the mucosa, even to the point that it mimics CD.29,30 The HygiPrep is a gravity-fed and defecation-inducing colonic lavage that does not use any chemicals that might affect the mucosa. The prep induced peristalsis as the water gently flows in the gut lumen and naturally loosens the colon content, including that of the ascending (right) colon.26,27 Therefore, this prep is likely to be less disruptive for the bowels of IBD patients and circumvents the disruptive nature of the oral purgative prep while providing a more accurate assessment of disease activity.
The high-volume gravity-fed colonic lavage with induced defecation (HygiPrep) BP holds both clinical and patients facing advantages and increases patients' compliance with clinical guidelines for managing the disease. In addition, from a research perspective, studying the colon effluent, mucosa layer, and gut epithelial from a gut that was not prepped using a chemical agent can hold a myriad of benefits, from accurate biomarkers detection to microbiome research for personalized medicine. We suggest that the presented consistent BP adequacy and high patient satisfaction make this defecation-inducing colonic lavage a favorable strategy for colonoscopy preparation in IBD patients and can be a powerful tool in improving disease management and treatment for this population.
Contributor Information
Amit Gajera, Ohio GI & Gastro Health, Norwood Endoscopy Center, Cincinnati, Ohio, USA.
Christopher South, Ohio GI & Gastro Health, Norwood Endoscopy Center, Cincinnati, Ohio, USA.
Kevin M Cronley, Ohio GI & Gastro Health, Norwood Endoscopy Center, Cincinnati, Ohio, USA.
John J Ziebert, Austin Gastro & GI Alliance, Endoscopy Center I (North) Austin, Texas, USA.
Cynthia H Wrigh, GI Alliance, GI Associates and Endoscopy Center, Flowood, Mississippi, USA.
Orly Levitan, Hygieacare Inc., Clinical & Regulatory, Norfolk, Virginia, USA.
Dawn B Burleson, Hygieacare Inc., Clinical & Regulatory, Norfolk, Virginia, USA.
David A Johnson, Eastern VA Medical School, Chief of Gastroenterology, Norfolk, Virginia, USA.
Funding
The data for this retrospective study were mined using the Hygieacare Inc. database. There was no external funding for this study.
Conflicts of Interest
Amit Gajera, Christopher South, Kevin M. Cronley, John J. Ziebert, and Cynthia H. Wright declare that they have no conflict of interest. Orly Levitan and Dawn B. Burleson: Employees of Hygieacare Inc. David A. Johnson: consultant for Johnson and Johnson, Hygieacare Inc., and ISOThrive Inc.
Data Availability
Not publicly available.
References
- 1. Bray C, Bell LN, Liang H, Collins D, Yale SH.. Colorectal cancer screening. WMJ. 2017;116(1):27–33. [PubMed] [Google Scholar]
- 2. Keller DS, Windsor A, Cohen R, Chand M.. Colorectal cancer in inflammatory bowel disease: review of the evidence. Tech Coloproctol. 2019;23(1):3–13. [DOI] [PubMed] [Google Scholar]
- 3. Stidham RW, Higgins PDR.. Colorectal cancer in inflammatory bowel disease. Clin Colon Rectal Surg. 2018;31(3):168–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jess T, Rungoe C, Peyrin-Biroulet L.. Risk of colorectal cancer in patients with ulcerative colitis: a meta-analysis of population-based cohort studies. Clin Gastroenterol Hepatol. 2012;10(6):639–645. [DOI] [PubMed] [Google Scholar]
- 5. Herrinton LJ, Liu L, Levin TR, Allison JE, Lewis JD, Velayos F.. Incidence and mortality of colorectal adenocarcinoma in persons with inflammatory bowel disease from 1998 to 2010. Gastroenterology. 2012;143(2):382–389. [DOI] [PubMed] [Google Scholar]
- 6. von Roon AC, Reese G, Teare J, Constantinides V, Darzi AW, Tekkis PP.. The risk of cancer in patients with Crohn’s disease. Dis Colon Rectum. 2007;50(6):839–855. [DOI] [PubMed] [Google Scholar]
- 7. Winther KV, Jess T, Langholz E, Munkholm P, Binder V.. Long-term risk of cancer in ulcerative colitis: a population-based cohort study from Copenhagen County. Clin Gastroenterol Hepatol. 2004;2(12):1088–1095. [DOI] [PubMed] [Google Scholar]
- 8. Bernstein CN, Blanchard JF, Kliewer E, Wajda A.. Cancer risk in patients with inflammatory bowel disease: a population-based study. Cancer. 2001;91(4):854–862. [DOI] [PubMed] [Google Scholar]
- 9. Kornbluth A, Sachar DB; Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105(3):501–523. [DOI] [PubMed] [Google Scholar]
- 10. Farraye FA, Odze RD, Eaden J, et al. . AGA medical position statement on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138(2):738–745. [DOI] [PubMed] [Google Scholar]
- 11. Clarke WT, Feuerstein JD.. Colorectal cancer surveillance in inflammatory bowel disease: practice guidelines and recent developments. World J Gastroenterol. 2019;25(30):4148–4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Singh K, Al Khoury A, Kurti Z, et al. . High adherence to surveillance guidelines in inflammatory bowel disease patients results in low colorectal cancer and dysplasia rates, while rates of dysplasia are low before the suggested onset of surveillance. J Crohns Colitis. 2019;13(10):1343–1350. [DOI] [PubMed] [Google Scholar]
- 13. Velayos FS, Liu L, Lewis JD, et al. . Prevalence of colorectal cancer surveillance for ulcerative colitis in an integrated health care delivery system. Gastroenterology. 2010;139(5):1511–1518. [DOI] [PubMed] [Google Scholar]
- 14. Friedman S, Cheifetz AS, Farraye FA, et al. . Factors that affect adherence to surveillance colonoscopy in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19(3):534–539. [DOI] [PubMed] [Google Scholar]
- 15. Audibert C, Perlaky A, Glass D.. Global perspective on colonoscopy use for colorectal cancer screening: a multi-country survey of practicing colonoscopists. Contemp Clin Trials Commun. 2017;7:116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mahmood S, Farooqui SM, Madhoun MF.. Predictors of inadequate bowel preparation for colonoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2018;30(8):819–826. [DOI] [PubMed] [Google Scholar]
- 17. Hendry PO, Jenkins JT, Diament RH.. The impact of poor bowel preparation on colonoscopy: a prospective single centre study of 10 571 colonoscopies. Colorectal Dis. 2007;9(8):745–748. [DOI] [PubMed] [Google Scholar]
- 18. Sulz MC, Kröger A, Prakash M, Manser CN, Heinrich H, Misselwitz B.. Meta-analysis of the effect of bowel preparation on adenoma detection: early adenomas affected stronger than advanced adenomas. PLoS One. 2016;11(6):e0154149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nett A, Velayos F, McQuaid K.. Quality bowel preparation for surveillance colonoscopy in patients with inflammatory bowel disease is a must. Gastrointest Endosc Clin. 2014;24(3):379–392. [DOI] [PubMed] [Google Scholar]
- 20. Goetz M. Endoscopic surveillance in inflammatory bowel disease. Visc Med. 2018;34(1):66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Underwood JA, Bekal P, Levitan O, Burleson DB, Johnson DA.. Hygieacare prep for colonoscopy consistently provides 97% adequacy, and is agnostic to predictors of poor oral bowel prep. Gastrointest Endosc. 2020;91(6):AB573–AB574. [Google Scholar]
- 22. Sportes A, Delvaux M, Huppertz J, Hernandez C, Gay G.. Randomized trial comparing high volume rectal water irrigation with standard 4 L split-dose PEG preparation before colonoscopy. J Gastroenterol Dig Dis. 2016;1(1):1–6. [Google Scholar]
- 23. Gagneja HK, Parekh P, Burleson DB, Johnson D.. Patient satisfaction and willingness to pay out of pocket for future HyGIeaCare preps: 2403. Am J Gastroenterol. 2016;111(ACG Annual Meeting Abstracts Supplement 2016):S1236. [Google Scholar]
- 24. Parekh P, Burleson D, Lubin C, Johnson DA.. Colon irrigation: effective, safe, and well-tolerated alternative to traditional therapy in the management of refractory chronic constipation. J Clin Gastroenterol Hepatol. 2018;2(1):1–5. [Google Scholar]
- 25. Hogan RB II, Underwood JA, Wright C, Lestina S, Mangels DG, O’Toole T.. Open-system colon irrigation bowel prep for colonoscopy is a safe and effective alternative to oral prep. JSM Gastroenterol Hepatol. 2021;8(1):1098–2006. [Google Scholar]
- 26. Gagneja HK, Parekh P, Burleson D, Johnson D.. HyGIeaCare® preparation for colonoscopy—a technical update for success. J Gastrointest Dig Syst. 2016;6(458):1–4. [Google Scholar]
- 27. Godell C, Frachtman R, Peake C, Sperling RM, Havemann BD, Ziebert JJ.. Colon irrigation bowel preparation supports multiple clinical benefits in over 8,000 patients. Open J Gastroenterol Hepatol. 2021;4(2):48:1–15. [Google Scholar]
- 28. Colombel JF, Rutgeerts P, Reinisch W, et al. . Early mucosal healing with infliximab is associated with improved long-term clinical outcomes in ulcerative colitis. Gastroenterology. 2011;141(4):1194–1201. [DOI] [PubMed] [Google Scholar]
- 29. Pockros PJ, Foroozan P.. Golytely lavage versus a standard colonoscopy preparation. Effect on normal colonic mucosal histology. Gastroenterology. 1985;88(2):545–548. [DOI] [PubMed] [Google Scholar]
- 30. Zwas FR, Cirillo NW, el-Serag HB, Eisen RN.. Colonic mucosal abnormalities associated with oral sodium phosphate solution. Gastrointest Endosc. 1996;43(5):463–466. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not publicly available.