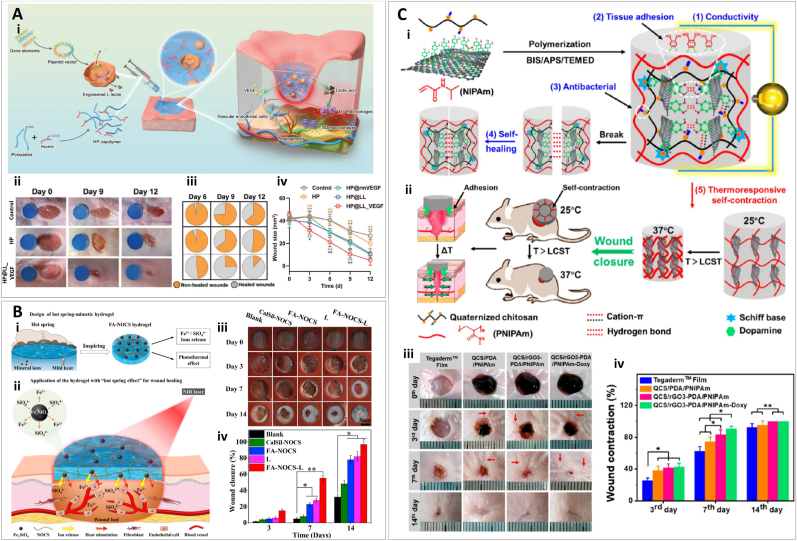
Fig. 8.
Wound dressing using other bioactive agents. (A) (i) This graphic represents the accelerating angiogenesis in diabetic wounds by promoting the angiogenic capacity of endothelial cells and inducing macrophages toward M2 polarization. (ii) Representative pictures of the wound area in response to different treatments (HP: heparin poloxamer; HP@rm VEGF: heparin poloxamer with VEGF; HP@LL: heparin poloxamer with Lactococcus lactis; HP@LL_VEGF: heparin poloxamer with VEGF-producing L. lactis) on days 0, 6, 9, and 12. The blue circle with a 6 mm diameter indicates the initial wound size. (iii) Fractions of the wounds healed with the different treatments. (iv) Quantitative analysis of the wound area for each group (n = 6). Reprinted and adapted with permission from Lu et al., 2021 [232]. (B) (i) Design of a hot spring-mimetic hydrogel, where there is Fe2+/SiO44− ion release and photothermal effect provided by fayalite (FA). (ii) Application of the hot spring-mimetic hydrogel for promoting angiogenesis in wound healing due to bioactive ions and heat stimulation. (FA: Fe2SiO4; NOCS: N, O-carboxymethyl chitosan. Yellow and red arrow heads denote the release of Fe2+/SiO44− ions and the photothermal heating effect of fayalite particles, respectively). (iii) Pictures of wounds treated with FA-NOCS hydrogel, calcium silicate (Calsil)-NOCS hydrogel and/or infrared irradiation (L: laser irradiation only). (iv) Wound closure percentage of different treatments. Reprinted and adapted with permission from Sheng et al., 2021 [235]. (C) (i) Schematic representation of quaternized chitosan (QCS), polydopamine-coated reduction graphene oxide (rGO-PDA), and poly(N-isopropylacrylamide) (PNIPAm) (QCS/rGO-PDA/PNIPAm) hydrogel preparation and its properties. (ii) Schematic diagram of the hydrogels assisting wound closure by thermoresponsive self-contraction. (iii) Pictures of wounds treated with Tegaderm film dressing (control), QCS/PDA/PNIPAm, QCS/rGO3 (containing 3 mg/mL rGO) PDA/PNIPAm, and QCS/rGO3-PDA/PNIPAm-Doxycycline hydrochloride (Doxy) in a murine model on days 0, 3, 7, and 14. (iv) Wound contraction percentage for each treatment. Reprinted and adapted with permission from Sheng et al., 2021 [236].