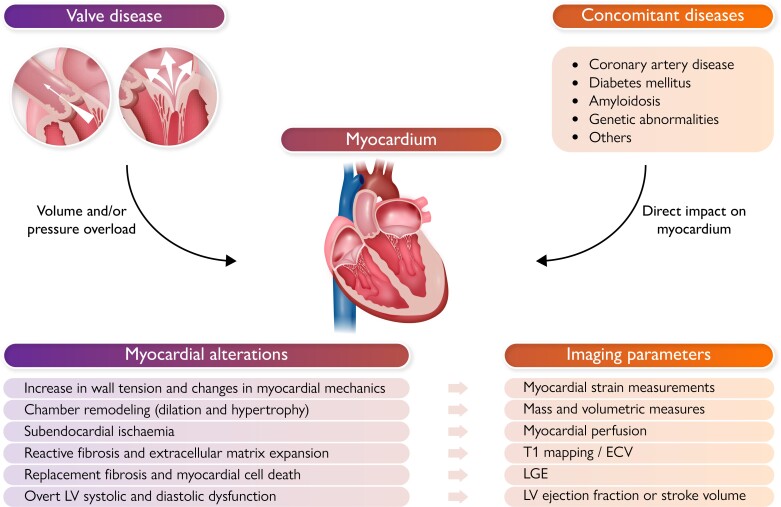
Graphical Abstract.
In the presence of severe valvular heart disease (and associated comorbidities), cardiac chambers are exposed to either pressure (as in aortic stenosis) or volume overload (as in mitral regurgitation), which triggers at first a series of adaptive mechanisms to release wall tension and maintain cardiac output (namely chamber hypertrophy and/or dilatation). However, these compensatory phenomena are soon followed by maladaptive myocardial changes such as reactive fibrosis, microvascular ischemia and cell death with replacement fibrosis, which substantially impair their function. New imaging biomarkers (namely obtained from echocardiography and cardiac magnetic resonance imaging) are capable of depicting the occurrence of such maladaptive changes with important potential impact on patient risk stratification and decision making. Particularly, global longitudinal strain has shown to be a sensitive marker of systolic dysfunction and cardiac magnetic resonance imaging has the key strength of myocardial tissue characterization, including fibrosis an inflammation, but also myocardial perfusion and energetics, and therefore offers an in-vivo “virtual histology”.