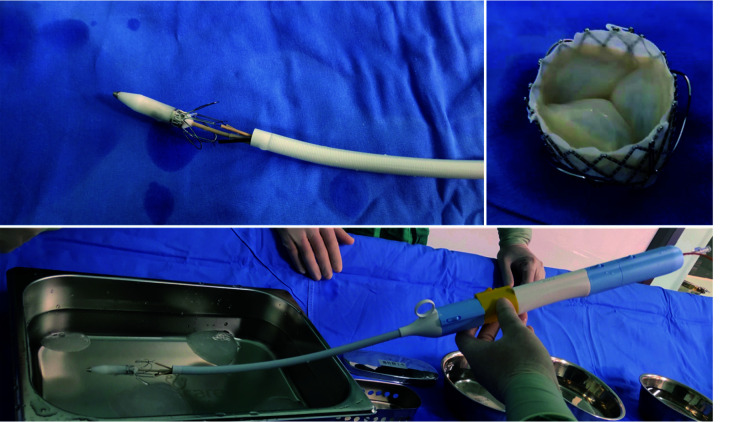
Aortic annulus calcification (AC) and mitral AC are common in patients with cardiac valvular disease.[1] Procedures to resect or debride aortic AC and mitral AC may lead to cerebral emboli, heart failure, arrhythmia, coronary artery lesions, and even ventricular rupture.[2] Therefore, it is often a challenge for surgeons to choose an appropriate surgical strategy for patients with severe valvular AC.[3,4] A sutureless valve is a good choice, doing away with the need to take time to remove the AC, but many countries do not have this valve. Transcatheter aortic valve implantation (TAVI) and transcatheter mitral valve replacement (TMVR) have developed rapidly during recent years.[5–7] Artificial stent valves for TAVI use offer another choice for patients requiring surgical aortic valve replacement or surgical mitral valve replacement in severe AC.[6,8–10] The J-valve is a short frame, interventional valve developed in China. It is a second-generation, self-expandable stent device with three U-shaped graspers, and has been approved for treating both aortic stenosis and aortic regurgitation (Figure 1). Trans-apical transcatheter valve replacement in patients using the J-valve system has been previously reported.[11] The unique structure with graspers, a low profile, and bare metal area at the coronary orifice region is efficacious for positioning, stabilizing, and avoiding obstruction of the coronary arteries in open cardiac surgery. Therefore, we implemented the use of the J-valve during traditional cardiac surgery in two cases presenting with unexpected complications of AC.
Figure 1.
The J-valve system for trans-apical transcatheter valve replacement.
The J-valve is a second-generation self-expandable device with three U-shaped graspers and has been approved for treating both aortic stenosis and regurgitation in China. Patients underwent trans-apical transcatheter valve replacement using the J-valve system.
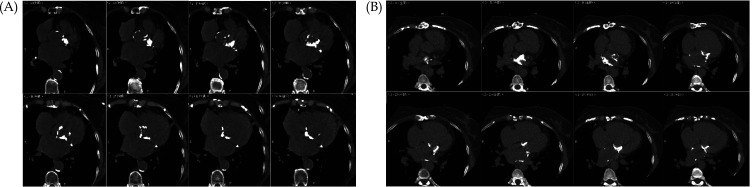
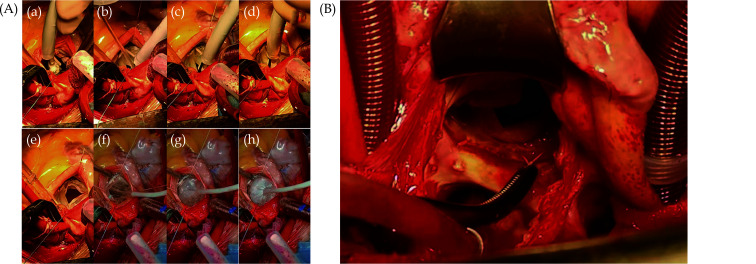
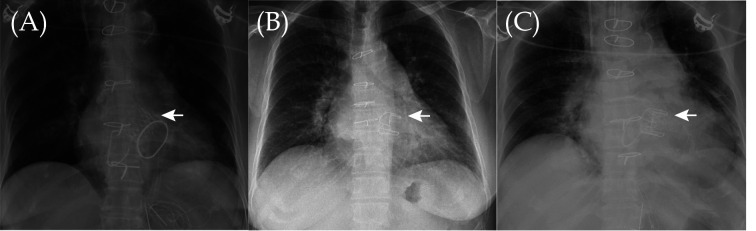
Case 1 A 75-year-old woman was the first case. She showed marked limitation of physical activity. At admission, echocardiography showed severe aortic valve stenosis with moderate regurgitation, severe mitral regurgitation, and atrial fibrillation. Chest computed tomography showed severe aortic AC and severe mitral posterior AC (Figure 2A). The preoperative EuroSCORE II for this patient was 2.4%. From previous experience, we planned intraoperative debridement of the severe AC and replacement of the valve with a bioprosthetic valve. The median sternotomy approach was used and cardiopulmonary bypass was established routinely. Unexpected severe and extensive calcification in the aortic valve and annulus was found. The calcification extended deep into the left ventricular myocardium. Considering the potential risks and time required for removing the calcification, and annulus reconstruction, and that the sutureless valves were not yet approved for clinical use in China, we decided to use a TAVI valve under direct view to simplify the procedure. The J-valve was designed for aortic valves TAVI and the short frame design was an ideal temporary choice under direct view. The intraoperative diameter of aortic annulus was 22–23 mm. With consent from the patient’s family, the J-valve (size: 25 mm) was implanted under direct vision through the aortic incision. Post dilatation with balloon valvuloplasty was used to confirm that the valve was connected tightly to the AC annulus (Figure 3A). The mitral valve was repaired using the edge-to-edge approach with a 36 Carpentier-Edwards physio II ring. The aortic cross-clamp time was 135 min. After the heart beat again, the intraoperative transthoracic echocardiogram revealed only a trace of a paravalvular leak in the aortic valve and mild mitral regurgitation. Tracheal extubation was performed 12 h postoperatively and the patient was discharged at seven days postoperatively. Echocardiographic examinations and chest radiographs at one-year follow-up revealed a satisfactory position and function of the J-valve (Figure 4A). Additionally, the patient demonstrated significant improvement in her clinical condition.
Figure 2.
Chest computed tomography findings.
(A): Chest computed tomography of the first patient shows severe aortic annulus calcification and severe mitral posterior annulus calcification; and (B): chest computed tomography of the second patient shows severe calcification in the posterior wall of the left atrium and mitral posterior annulus calcification.
Figure 3.
Photographs from the surgeries.
(A): The J-valve was implanted into the aortic annulus of the first patient. We installed the J-valve into the valvular conveying system in the reverse direction, released the three U-shaped graspers, and then pulled them down to the bottom of the aortic sinuses (a–e). Post-implantation balloon valvuloplasty was necessary (f–h); and (B): the degenerated bioprosthetic mitral valve of the second patient.
Figure 4.
The post-operative chest radiographs.
(A): The post-operative chest radiograph of the first patient. The chest radiograph showed a satisfactory position of the J-valve at one year postoperatively; (B): the preoperative chest radiograph of the second patient. The image of the mitral valve bioprosthesis can be seen on the radiograph; and (C): the post-operative chest radiograph of the second patient. The chest radiograph showed a satisfactory position of the J-valve at six months postoperatively.
Case 2 A 58-year-old woman was the second case whom referred to our hospital because of a degenerated mitral valve bioprosthesis (Figure 4B). At admission, echocardiography showed a degenerated bioprosthetic mitral valve, severe bioprosthetic mitral valve regurgitation, moderate tricuspid regurgitation, and severe pulmonary hypertension. Chest computed tomography showed severe calcification of the posterior mitral annulus of the left atrium and posterior mitral AC. However, because of the metal stent of the bioprosthetic mitral valve, the degree of posterior mitral AC could not be confirmed clearly (Figure 2B). Therefore, TMVR or valve-in-valve (ViV) procedure was not the first choice for this patient.[12] We decided to perform a repeat open heart surgery for this patient. The degenerated bioprosthetic mitral valve was exposed through an interatrial groove incision (Figure 3B). However, unexpected severe calcification existed extensively in the posterior mitral annulus, which was connected and fused with the bioprosthetic stent and left ventricle. Considering that removal of the calcification might take too long, and may cause left ventricular damage, even rupture, we decided to implant a TAVR valve as ViV procedure to simplify the surgery. With consent from the patient’s family, we implanted the J-valve into the degenerated bioprosthetic mitral valve as mitral ViV procedure under direct vision. The degenerated bioprosthetic mitral valve was 25 mm Carpentier-Edwards Perimount Magna Ease valve with the true inner diameter as 23 mm. The 25 mm J-valve was implanted. Subsequently, a post-implantation balloon (size: 25 mm) dilatation was performed and the tricuspid valve was repaired as usual. The aortic cross-clamp time was 70 min. Intraoperative transthoracic echocardiogram showed no paravalvular leak from the mitral valve. Tracheal extubation was performed 16 h postoperatively. The patient recovered and was discharged six days postoperatively. Several echocardiographic examinations and chest radiographs showed a satisfactory position and function of the J-valve after six months follow-up (Figure 4C). Echocardiography showed a significant reduction in pulmonary hypertension from 91 mmHg (preoperative) to 40 mmHg (postoperative). The activity tolerance of the patient was significantly improved.
The first case may be the first report of J-valve implantation with severe aortic calcification during traditional surgery. Most of the current TAVI valves have a long frame design, making it difficult to implant under direct vision and potentially affecting aortic root incision closure. The J-valve, a self-expandable device with a short frame and three U-shaped graspers for the coronary sinus, is an ideal option for such cases. This surgical procedure significantly reduces the risk and duration of surgery and has satisfactory follow-up results. In 2009, Cheung, et al.[13] from St. Paul’s Hospital in Canada, reported on the first case of trans-apical TMVR for ViV. Thereafter, this procedure has been increasingly reported.[14] A multicenter registration study on TMVR involving 322 patients, reported an average STS (The Society of Thoracic Surgeons mortality risk score) score of 9.2% ± 7.2%.[6] Patients with NYHA IV accounted for 32.3%. The average left ventricular ejection fraction was 53.3% ± 11.5%. Patients with previous myocardial infarction accounted for 12.1%. 59.9% of patients underwent trans-apical mitral ViV and 38.8% of patients underwent trans-atrial septal approach ViV. The surgical success rate was 94.4%. The thirty-day and one-year mortality rates were 6.2% and 14%, respectively. The results in our cases highlighted the effectiveness of mitral ViV for degenerated bioprostheses as a temporary solution for unexpectedly difficult situations caused by during traditional cardiac surgery. The severity of ACs can be missed or misidentified during preoperative examinations. Degenerated bioprostheses may require the intraoperative removal of calcification using the traditional approach. However, this procedure may take a longer bypass time with higher risks of complications. Our case may be the first report of J-valve implantation into a failed bioprosthetic mitral valve (ViV) during traditional cardiac surgery, with good results seen during the follow-up. J-valve implantation under direct vision provides a simplified choice for emergencies during traditional cardiac surgery.
Despite its benefits, there are limited conditions suitable for implanting the J-valve under direct view. More case data with longer follow-up are required for a more accurate evaluation of this therapeutic approach. If the severity of cardiac AC exceeds preoperative assessment in traditional cardiac surgery, J-valve or ViV implantation presents a useful intraoperative risk management strategy.
ACKNOWLEDGMENTS
This study was supported by the Development and Research Fund of Topical Medicine (2020-2-2065), and the International Key Research and Development Program of Ministry of Science and Technology (2020YFC2008105). All authors had no conflicts of interest to disclose.
References
- 1.Boulif J, Slimani A, Lazam S, et al Diagnostic and prognostic accuracy of aortic valve calcium scoring in patients with moderate-to-severe aortic stenosis. Front Cardiovasc Med. 2021;8:673519. doi: 10.3389/fcvm.2021.673519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexis SL, Malik AH, El-Eshmawi A, et al Surgical and transcatheter mitral valve replacement in mitral annular calcification: a systematic review. J Am Heart Assoc. 2021;10:e018514. doi: 10.1161/JAHA.120.018514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sorajja P, Gössl M, Bae R, et al Severe mitral annular calcification: first experience with transcatheter therapy using a dedicated mitral prosthesis. JACC Cardiovasc Interv. 2017;10:1178–1179. doi: 10.1016/j.jcin.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 4.Ge Y, Gupta S, Fentanes E, et al Role of cardiac CT in pre-procedure planning for transcatheter mitral valve replacement. JACC Cardiovasc Imaging. 2021;14:1571–1580. doi: 10.1016/j.jcmg.2020.12.018. [DOI] [PubMed] [Google Scholar]
- 5.Tiwana J, Aldea G, Levin DB, et al Contemporary transcatheter mitral valve replacement for mitral annular calcification or ring. JACC Cardiovasc Interv. 2020;13:2388–2398. doi: 10.1016/j.jcin.2020.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Yoon SH, Whisenant BK, Bleiziffer S, et al Outcomes of transcatheter mitral valve replacement for degenerated bioprostheses, failed annuloplasty rings, and mitral annular calcification. Eur Heart J. 2019;40:441–451. doi: 10.1093/eurheartj/ehy590. [DOI] [PubMed] [Google Scholar]
- 7.Gheorghe L, Brouwer J, Wang DD, et al Current devices in mitral valve replacement and their potential complications. Front Cardiovasc Med. 2020;7:531843. doi: 10.3389/fcvm.2020.531843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Russell HM, Guerrero ME, Salinger MH, et al Open atrial transcatheter mitral valve replacement in patients with mitral annular calcification. J Am Coll Cardiol. 2018;72:1437–1448. doi: 10.1016/j.jacc.2018.07.033. [DOI] [PubMed] [Google Scholar]
- 9.Simonato M, Whisenant B, Ribeiro HB, et al Transcatheter mitral valve replacement after surgical repair or replacement: comprehensive midterm evaluation of valve-in-valve and valve-in-ring implantation from the VIVID registry. Circulation. 2021;143:104–116. doi: 10.1161/CIRCULATIONAHA.120.049088. [DOI] [PubMed] [Google Scholar]
- 10.Spitzer E, Mylotte D, Lauten A, et al Editorial: TAVI and the challenges ahead. Front Cardiovasc Med. 2020;7:149. doi: 10.3389/fcvm.2020.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li F, Wang X, Wang Y, et al Structural valve deterioration after transcatheter aortic valve implantation using J-valve: a long-term follow-up. Ann Thorac Cardiovasc Surg. 2020;26:158–165. doi: 10.5761/atcs.oa.19-00325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Condado JF, Kaebnick B, Babaliaros V Transcatheter mitral valve-in-valve therapy. Interv Cardiol Clin. 2016;5:117–123. doi: 10.1016/j.iccl.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Cheung A, Webb JG, Wong DR, et al Transapical transcatheter mitral valve-in-valve implantation in a human. Ann Thorac Surg. 2009;87:e18–e20. doi: 10.1016/j.athoracsur.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 14.Ristalli F, Maiani S, Hamiti B, et al Percutaneous trans-septal mitral valve-in-ring implantation using a transcatheter balloon-expandable transcatheter heart valve with elective intra-procedural artero-venous ECMO in a patient with severely reduced left ventricular ejection fraction. Front Cardiovasc Med. 2019;6:174. doi: 10.3389/fcvm.2019.00174. [DOI] [PMC free article] [PubMed] [Google Scholar]