Abstract
Introduction
Perceived benefits like decreased contamination rates and reduced postoperative incidence of complications after urolithiasis surgery have led to increased adoption of single-use flexible ureteroscopes (su-fURS). Using a validated, standardized simulator model with enhanced “fluoroscopic” capabilities, we performed an in vitro comparative assessment of four commercially available models of su-fURS. Both objective and subjective parameters were assessed in this study.
Methods
Two standardized tasks, (1) exploration of the model's kidney collecting system and (2) repositioning of a stone fragment from the upper renal to lower renal pole were assigned to participants, who performed these tasks on all four scopes. Four models of su-fURS (Boston LithoVue, PUSEN PU3033A, REDPINE, INNOVEX EU-Scope<sup>TM</sup>) were assessed, with task timings as end-points for objective analysis. Cumulative “fluoroscopic” time was also recorded as a novel feature of our enhanced model. Post-task questionnaires evaluating specific components of the scopes were distributed to document subjective ratings.
Results
Both subjective and objective performances (except stone repositioning time) across all four su-fURS demonstrated significant differences. However, objective performance (task timings) did not reflect subjective scope ratings by the participants (R<sub>s</sub> < 0.6). Upon Kruskal-Wallis H test with post hoc analyses, REDPINE and INNOVEX EU-Scope<sup>TM</sup> were the preferred su-fURS as rated by the participants, with overall scope scores of 9.00/10 and 9.57/10.
Conclusions
Using a standardized in vitro simulation model with enhanced fluoroscopic capabilities, we demonstrated both objective and subjective differences between models of su-fURS. However, variations in perception of scope features (visibility, image quality, deflection, maneuverability, ease of stone retrieval) did not translate into actual technical performance. Eventually, the optimal choice of su-fURS fundamentally lies in individual surgeon preference, as well as cost-related factors.
Keywords: Single-use flexible ureteroscope, Disposable ureteroscope, Reusable ureteroscope
Introduction
With the advent of flexible ureteroscopy (fURS) as a treatment modality, we have seen a drastic improvement in both diagnostic and therapeutic outcomes of stone management [1]. Pathologies of the upper urinary tract have been made more accessible, and urolithiasis in patients with challenging circumstances such as large renal calculi is now amenable to management with fURS [2]. However, with the widespread adoption of reusable flexible ureteroscopies (r-fURS), secondary issues have been raised pertaining to its use. Most notably, preprocedural contamination concerns, maintenance costs, and reprocessing fees are taken into account [3]. Initial capital expenditure of procuring such equipment is also hefty [4]. A study by Ofstead et al. [5] demonstrated the persistence of microbiological organisms within the r-fURS despite undergoing thorough decontamination processes postsurgery. Moreover, the manual cleaning also incurs sizeable labor costs, adding to the financial liability of usage. In a bid to address these shortcomings, single-use flexible ureteroscopes (su-fURS) were developed as a practical solution to the lack of sterility and cost-inefficiency.
There are many commercially available su-fURS in clinical practice, with more being introduced annually. In Singapore, brands most commonly deployed include LithoVue (Boston Scientific, MA, USA), Uscope (PUSEN Medical Technology Pte. Ltd., Zhuhai, China), REDPINE (REDPINE Medical Instruments, Guangzhou, China), and INNOVEX (ANQING Medical, Shanghai, China). Presently, a number of clinical retrospective studies have evaluated a few of these models to assess the utility of su-fURS [6, 7, 8, 9]. Despite so, there is no clear-cut consensus or recommendation on how and when to choose a su-fURS [10], coupled with a paucity of clinical evidence on how to assess a particular su-fURS model. A good option is to self-evaluate objective and subjective performance parameters of each device. This has hence formed the basis of our study. For an extensive evaluation, an in vitro testing environment has to be simulated. Our current study aims to adopt a head-to-head comparative assessment of su-fURS, evaluating both subjective and objective performances of each device. Standardization was achieved by performing the evaluation on a validated retrograde intrarenal simulator model with novel fluoroscopic capabilities utilizing a reusable ureteroscope (Karl Storz Flex-X2) as the control.
Methods
Participants
This study was approved by the National Healthcare Group Domain Specific Review Board, reference number 2021/00924. Seven practicing urologists from two sister institutions of the Singapore National University Health System were invited and consented to participate in this study. The cohort comprised two residents (year 2 and year 3, respectively) and five consultants with variable years of experience in endourology. They were briefed on the study tasks, as well as intratask and post-task evaluation methods. A baseline questionnaire (refer to online suppl. material; for all online suppl. material, see www.karger.com/doi/10.1159/000525246) was issued for collection of demographic information and to ascertain the level of participant expertise in retrograde intrarenal surgery (RIRS).
Completion of Tasks
Each participant performed two tasks during their evaluation: (1) endoscopic visualization and exploration of the model's kidney collecting system via a ureteric sheath, (2) basketing and repositioning a stone from the lower to upper calyx, with a standardized nitinol stone-extracting basket. During the stone transfer, participants were aided by a passive assistant, who only opened and closed the basket upon receiving instructions to do so. These tasks were adapted from a previous ureteroscopy task trainer study [11]. All tasks were performed initially with a control r-fURS (Karl-Storz Flex-X2) for participant familiarization with the simulator model. Subsequently, the other four su-fURS were utilized for assessment. Technical features of all ureteroscopes are specified in Table 1. A total of 35 exercises with 70 actions were recorded for statistical analysis. All participants had to complete both tasks on the same scope before moving on to the next su-fURS model. A numbers lottery method was used for randomization of the order of testing to prevent opportunistic recall of the previous device. Each surgeon performed both tasks on all five ureteroscope models in one sitting. The aforementioned efforts were incorporated to minimize any user bias.
Table 1.
Technical features of ureteroscopes
| Details | Boston LithoVue | PUSEN PU3033A | REDPINE RP-U-C12 | INNOVEX EU-ScopeTM US31B-12 |
|---|---|---|---|---|
| Manufacturer | Boston Scientific | PUSEN Medical | REDPINE Medical | SHANGHAI ANQING Medical |
| Type of use | Single-use | Single-use | Single-use | Single-use |
| Optical system | Digital CMOS | Digital CMOS | Digital CMOS | Digital CMOS |
| Length, mm | 680 | 650 | 670 | 650 |
| Working channel(s) | 1 | 1 | 1 | 1 |
| Working channel diameter, Fr | 3.6 | 3.6 | 3.2 | 3.6 |
| Tip diameter, Fr | 7.7 | 9.0 | 8.7 | 9.3 |
| Shaft diameter, Fr | 9.5 | 9.5 | 9.12 | 8.7 |
| Direction of deflection | Bidirectional | Bidirectional | Bidirectional | Bidirectional |
| Degree of deflection,° | 270/270 | 270/270 | 270/270 | 275/275 |
As all ureteroscopes possessed distinctive features and are easily identified, blinding the participants from the type of scope used was not possible. For the first task, the surgeon was provided with a diagrammatic template of the model's collecting system. They navigated and identified all calyces accordingly. Verification was reaffirmed by an independent study assessor (WZ So), who observed in detail the participant's progress throughout the task. The timing was started when the ureteroscope was inserted and stopped when the participant fully identified all calyces, as well as successfully repositioned the stone from the lower renal pole to the upper pole. The time taken to complete each task was recorded by a study team member.
Model Design
We used the Cook Endourology Model (Fig. 1) that includes three main components: a dual calyceal system (left), a complete left kidney-ureter-bladder system, and a tortuous ureter system (right). It is cased in a platform made up of acrylic and polycarbonate plastic. All components of the model are 3D printed with a translucent, acrylonitrile butadiene styrene-like plastic material and dyed red to simulate internal color and translucency. The model needs to be filled with water and includes an easy to fill and drain system. The model also houses a motorized suction system for the filtration of any remaining debris from the channeled areas, simulating high-pressure irrigation. This aids in providing quality visualization while any form of lithotripsy is performed in vitro. This model has been previously evaluated by a separate study and demonstrated good face, content, and construct validity [12].
Fig. 1.

Cook Endourology Model.
A novel enhancement that we have made to the model is the incorporation of “fluoroscopic” capabilities to simulate intraoperative fluoroscopic time. To achieve this, we placed an additional opaque film on the model acrylic cover (Fig. 2), powered by another internal motorized system. This film is transiently opaque, whereby the opacity can be toggled on or off with the flick of a switch (Fig. 3). To facilitate this, we have attached a wired foot pedal. By stepping on the foot pedal, an electric current is delivered to the opaque film, rendering it transparent. To fully simulate the element of fluoroscopy, we have added an electronic timer on the bottom-left corner of the cover, such that a cumulative fluoroscopy timing can be recorded. With the foot pedal depressed, the participant is able to see through the cover and appreciate the position of the ureteroscope within the model. This is akin to using the foot pedal during surgery to obtain a fluoroscopic image. The cumulative “fluoroscopy” time clocked by each participant was collected.
Fig. 2.
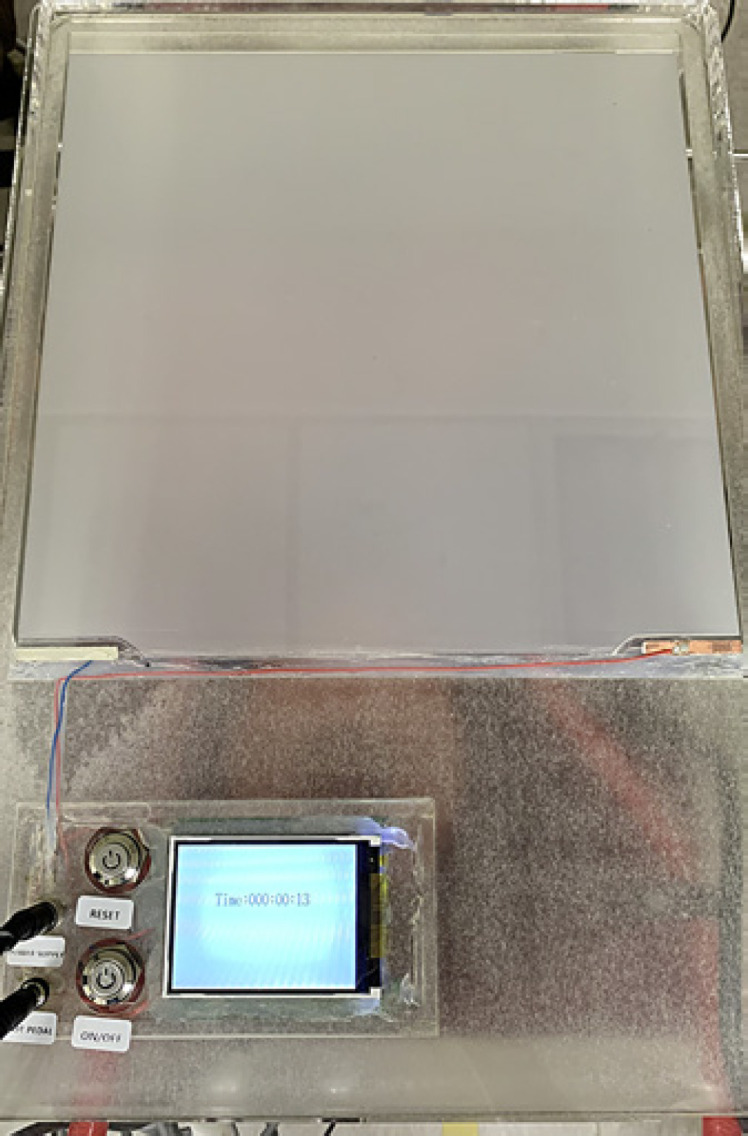
Model with opaque acrylic cover.
Fig. 3.
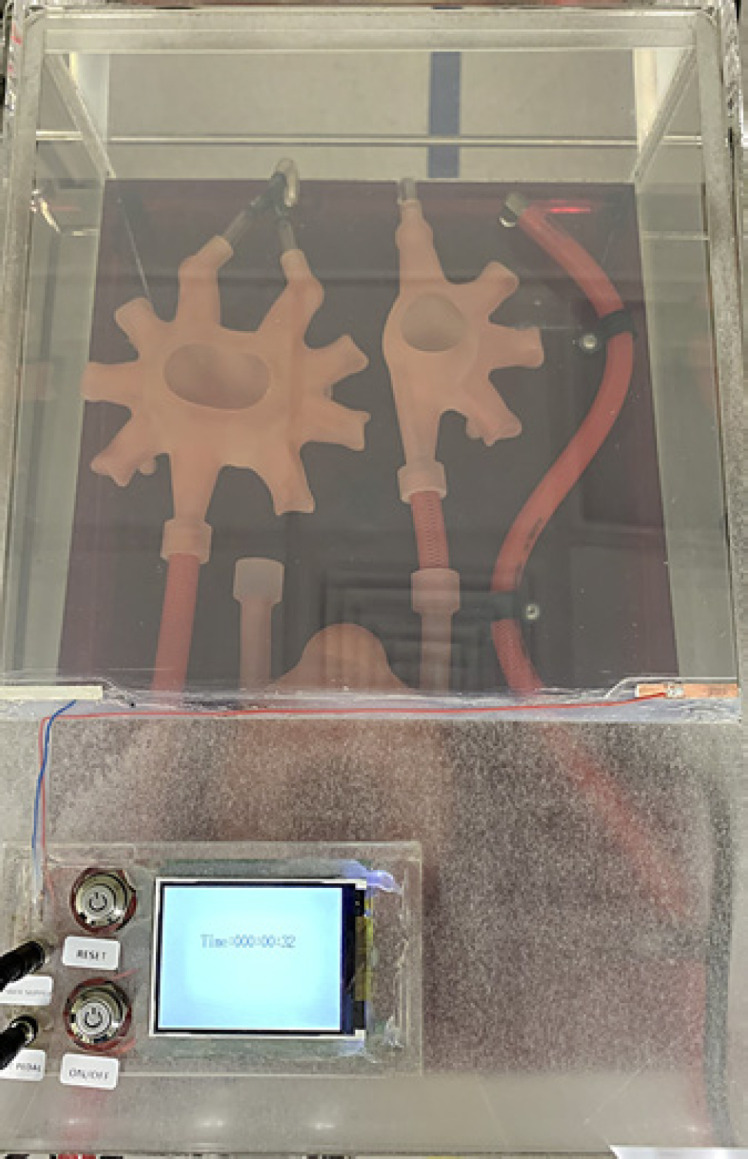
Model with opaque acrylic cover toggled off.
Post-Task Questionnaire
After completion of the assessment, participants were issued a post-task questionnaire (refer to online suppl. material) to evaluate the five ureteroscopes on five respective domains: visibility, deflection, maneuverability, ease of stone retrieval, and image quality during the procedure. These assessment categories have been utilized in other fURS studies as well [13, 14, 15]. Participants also gave each ureteroscope an overall performance score. Responses were graded on a 10-point Likert scale. In addition, participants also evaluated the face and content validity of our enhanced endourology model. The questionnaire can be found within the online supplementary material.
Statistical Analysis
χ2 tests (or Fisher's exact test, wherever applicable) and Independent T test were used to compare between categorical and continuous variables, respectively. All p values were two-tailed, and a p value of <0.05 was taken to be statistically significant. Categorical variables are reported as number (percent), while continuous variables are reported as mean (standard deviation; SD). Comparison of the scores attained by each scope within each domain was analyzed using Kruskal-Wallis H test with pair-wise comparison. Subsequently, post hoc analyses were carried out to identify the brands of su-fURS that demonstrated statistically significant differences. Comparison of task timings across different scopes was analyzed using Kruskal-Wallis H test as well. Spearman rank-order correlation was used to investigate the relationship between individual task timings achieved by participants and the overall scope scores, utilizing Spearman's rank correlation coefficient (Rs) as a measure of strength and direction of association. Absolute Rs values of >0.6 were considered as strong correlations between the two variables. All statistical analyses were performed using IBM SPSS Version 26.0.
Results
Baseline Characteristics
A total of 35 simulation exercises were done by seven practicing urologists of varying expertise (2 residents in year 2 and year 3, respectively, and five consultants with variable years of experience in endourology). All participants were male, with adequate prior experience in fURS and RIRS urological procedures.
Visibility and Image Quality
All domains of the post-task questionnaire demonstrated significant differences between the scores of four su-fURS (Table 2). For visibility (H(3) = 17.405, p = 0.001), REDPINE RP-U-C12 and INNOVEX EU-ScopeTM obtained significantly higher rates compared to PUSEN PU3033A and Boston LithoVue. INNOVEX EU-ScopeTM attained the highest mean score for visibility during the procedure (9.71/10).
Table 2.
Comparison of scope domains
| Mean scores | Boston LithoVue | PUSEN PU3033A | REDPINE RP-U-C12 | INNOVEX EU-ScopeTM US31B-12 |
|---|---|---|---|---|
| Visibility (1–10, mean) | 7.29 (REDPINE: 0.018) (INNOVEX: 0.003) |
6.86 (REDPINE: 0.005) (INNOVEX: 0.001) |
9.29 | 9.71 |
|
| ||||
| Deflection (1–10, mean) | 7.00 (REDPINE: 0.019) (INNOVEX: 0.014) |
7.43 | 8.86 | 9.00 |
|
| ||||
| Maneuverability (1–10, mean) | 7.29 (INNOVEX: 0.039) | 7.00 (REDPINE: 0.026) (INNOVEX: 0.014) |
8.71 | 9.00 |
|
| ||||
| Stone retrieval (1–10, mean) | 7.14 (REDPINE: 0.043) (INNOVEX: 0.005) |
7.29 (INNOVEX: 0.024) | 8.71 | 9.29 |
|
| ||||
| Image quality (1–10, mean) | 7.29 (REDPINE: 0.017) (INNOVEX: 0.001) |
6.86 (REDPINE: 0.014) (INNOVEX: 0.001) |
9.14 | 9.71 |
|
| ||||
| Overall score (1–10, mean) | 7.14 (REDPINE: 0.014) (INNOVEX: 0.001) |
6.71 (REDPINE: 0.016) (INNOVEX: 0.001) |
9.00 | 9.57 |
Significant p values (p < 0.05) for comparison with the respective su-fURS scope are provided in brackets and bolded.
Likewise, image quality scores also differed significantly between all four scopes (H(3) = 17.119, p = 0.001). Post hoc analysis concluded that REDPINE RP-U-C12 and INNOVEX EU-ScopeTM obtained significantly higher rates compared to PUSEN PU3033A and Boston LithoVue (Table 3). No significant differences were observed between PUSEN PU3033A and Boston LithoVue, as well as between REDPINE RP-U-C12 and INNOVEX EU-ScopeTM. INNOVEX EU-ScopeTM achieved the highest mean rating for image quality during the procedure (9.71/10).
Table 3.
Comparison of task timings
| Mean timings, mean±SD | Boston LithoVue | PUSEN PU3033A | REDPINE RP-U-C12 | INNOVEX EU-ScopeTM US31B-12 |
|---|---|---|---|---|
| Exploration of kidney collecting system, s | 34.14±6.64 (INNOVEX: 0.004) | 42.29±11.74 | 38.14±16.21 (INNOVEX: 0.024) | 54.29±9.57 |
| Stone repositioning from lower to upper calyx,* s | 33.86±9.84 | 35.29±18.36 | 41.71±17.48 | 53.71±13.97 |
| Cumulative fluoroscopy time, s | 10.43±9.69 (PUSEN: 0.013) | 39.71±19.93 | 7.14±6.69 (PUSEN: 0.001) | 22.14±21.40 |
The p values for comparison with the Karl Storz Flex-X2 r-fURS are provided in brackets. Significant differences (p < 0.05) are in bold. *No significant difference observed between all four single-use fURS (p = 0.098).
Deflection
Similarly, scope deflection rates also differed significantly when pegged against the r-fURS (H(3) = 9.126, p = 0.028). Post hoc analysis revealed that REDPINE RP-U-C12 (p = 0.019) and INNOVEX EU-ScopeTM (p = 0.014) scored significantly better than Boston LithoVue su-fURS. INNOVEX EU-ScopeTM achieved the highest mean rating for deflection during the procedure (9.00/10).
Maneuverability
Significant differences were observed with respect to scope maneuverability (H(3) = 9.603, p = 0.022). Post hoc analysis demonstrated that both REDPINE RP-U-C12 (p = 0.026) and INNOVEX EU-ScopeTM (p = 0.014) attained higher ratings compared to PUSEN PU3033A. On the other hand, only INNOVEX EU-ScopeTM (p = 0.039) performed significantly better than Boston LithoVue. Again, INNOVEX EU-ScopeTM achieved the highest mean rating for maneuverability during the procedure (9.00/10).
Ease of Stone Retrieval
When grading the ease of stone retrieval, significant differences were also observed (H(3) = 10.114, p = 0.018). INNOVEX EU-ScopeTM (p = 0.024) attained significantly higher scores than PUSEN PU3033A. Both REDPINE RP-U-C12 (p = 0.043) and INNOVEX EU-ScopeTM (p = 0.005) scored significantly better than Boston LithoVue. Again, INNOVEX EU-ScopeTM achieved the highest mean rating for maneuverability during the procedure (9.29/10).
Overall Scope Scores
Overall scope scores also varied significantly across all four su-fURS (H(3) = 17.679, p = 0.001). Post hoc analysis revealed that both REDPINE RP-U-C12 (p = 0.016, p = 0.014) and INNOVEX EU-ScopeTM (p = 0.001, p = 0.001) scored significantly better than PUSEN PU3033A and Boston LithoVue, respectively. Overall scores did not differ significantly between PUSEN PU3033A and Boston LithoVue, as well as between REDPINE RP-U-C12 and INNOVEX EU-ScopeTM. INNOVEX EU-ScopeTM was ranked as the best overall scope rated by the participants (9.57/10).
Exploration and Identification of Kidney Collecting System
Results of mean task timings are summarized in Table 3. Both visualization and correct verification of calices were achieved in all cases (100%). Average time to complete the first task across all scopes amounted to 54.3 s. Timings differed significantly across all four su-fURS (H(3) = 9.268, p = 0.026). Post hoc tests revealed that Boston LithoVue (p = 0.004) and REDPINE RP-U-C12 (p = 0.024) accrued significantly shorter timings than INNOVEX EU-ScopeTM. Boston LithoVue clocked the shortest mean timings for exploration and identification of the model's collecting system (34.14 s).
Stone Basketing and Repositioning
Unlike the timings for exploration and identification of the model's kidney collecting system, the differences seen across all four su-fURS did not achieve statistical significance (H(3) = 6.288, p = 0.098). Observably, the Boston LithoVue su-fURS clocked the shortest time among all (33.86 s).
Cumulative Fluoroscopy Time
The fluoroscopic time attained across all scopes differed significantly (H(3) = 11.300, p = 0.01). Individual post hoc analyses showed that Boston LithoVue (p = 0.013) and REDPINE (p = 0.001) clocked significantly shorter fluoroscopic timings than PUSEN PU3033A. Overall, REDPINE RP-U-C12 had the shortest cumulative fluoroscopic timing across all four scopes (7.14 s).
Correlation between Overall Scope Scores and Task Timings
For each individual scope, task timings (exploration and identification of kidney collecting system, stone repositioning, and cumulative fluoroscopy time) displayed weak correlations with overall scope scores (Rs < 0.6).
Model Validity
Our enhanced endourology model with fluoroscopic capabilities also demonstrated excellent face and content validity. The participants rated the model as realistic (mean score = 6.14/10) and considered it as a useful simulator training tool (mean score = 7.43/10).
Discussion
Our study contributes to the armamentarium of existing literature, elaborating on the ongoing debate between reusable versus single-use fURS. We tested a variety of commercially available single-use fURS to ensure adequate grounds for assessment. Using a standardized in vitro simulation model with enhanced fluoroscopic capabilities, we demonstrated both objective and subjective differences between models of su-fURS. INNOVEX EU-ScopeTM consistently attained the highest ratings across all aspects of the questionnaire, but completion of task timings did not reflect its subjective superiority. This is also substantiated by the weak correlation observed between overall scope scores and task timings.
In a recent scoping review of 48 articles by Hendriks et al. [16], they identified five key items in the assessment of flexible ureterorenoscopy: “maneuverability” (87.5%), “optics” (64.6%), “irrigation” (56.3%), “handling” (39.6%), and “durability” (35.4%). Single-use scope technology is evolving and new scopes are being progressively introduced in the market. It is thus imperative to constantly update the literature and aid urologists in making an educated choice when selecting the optimal device for use at their place of practice. Single-use digital fURS possess visibility and maneuverability profiles approaching that of a reusable digital flexible ureteroscope [17], and our study attempts the same. Using a standardized enhanced ureteroscopy model, it can be conclusively said that su-fURS demonstrated noninferiority in performance comparable to their reusable counterpart. This finding was also validated in a previous in vitro evaluative study that assessed a different series of su-fURS [11]. Both types of scopes either paralleled in performance or the r-fURS demonstrated superiority in technical features.
However, variations in surgeon preference of scope features (visibility, image quality, deflection, maneuverability, ease of stone retrieval) did not translate into actual technical advantages in the standardized tasks. An important application of in vitro studies like ours is their relevance to clinical studies. Particularly, it is beneficial to see how these experiences translate into improved safety and better stone-free rate.
A meta-analysis of 772 patients [9] undergoing either r-fURS or su-fURS reported higher stone-free rates achieved with su-fURS (OR 1.50, 95% CI: 1.06–2.12, p = 0.02), with no significant difference in perioperative complication rates. However, it is worth noting that su-fURS was also associated with longer operative times, which may not be accurately assessed in our study due to limitations of an in vitro environment.
Similarly, Meng et al. [18] and Huang et al. [19] concluded that in a modern era of RIRS, su-fURS are a comparable alternative to r-fURS in terms of surgical efficacy and safety for upper urinary calculi. This reiterates that commercially available su-fURS are likely to become the first-choice equipment, provided that they demonstrates cost-effectiveness specific to each institution of practice.
REDPINE RP-U-C12 (2021) and INNOVEX EU-ScopeTM su-fURS appeared to have performed the most optimally in our comparative study. Owing to the recency of their release, they are likely equipped with more advanced technological features (e.g., INNOVEX has a 160K resolution display with ×2.5 high imaging pixel) to amplify the endourological experience. However, as previously mentioned, subjective preferences of the surgeon did not necessarily correspond to better task timings, a surrogate marker for technical performance. LithoVue [20, 21], with its chip-on-tip technology, was the first disposable scope to be launched. Subsequently, evaluation by multiple authors had paved the way for adoption of su-fURS into mainstream practice. Since then, many flexible reusable scopes have been launched. Schlager et al. [11] were the first to comment that LithoVue offers performance and characteristics similar to a reusable device, while the FlexorVue's performance does not yet yield satisfactory results for clinical use. The first generation of Uscope exhibits potential but requires further technical improvements to match the performance of a reusable device. With the new-generation UE3022, PUSEN has made significant improvements and offers a quality comparable to the LithoVue's. The scopes evaluated in our study are reflective of how technology continues to improve, and in our study, we see that REDPINE RP-U-C12 (p = 0.016, p = 0.014) and INNOVEX EU-ScopeTM (p = 0.001, p = 0.001) scored significantly better than PUSEN PU3033A and Boston LithoVue, respectively.
With increased utility of disposable scopes comes responsibility, and the long-term environmental impact of su-fURS remains to be fully evaluated [22]. Even though su-fURS achieve similar clinical outcomes compared to the more expensive reusable counterparts, the ambiguity in a sustained adoption of su-fURS use also dwells upon other factors, including availability, insurance, case volume, and type of practice. Several papers reported equivocal cost-effectiveness [23] and possible incurrence of higher financing [24, 25, 26]. A study specifically demonstrated better cost-efficacy with r-fURS after 155–274 cases were performed [27], questioning the benefit of su-fURS usage in centers with heavy caseload.
Strengths and Limitations
To the best of our knowledge, this is the first head-to-head comparative in vitro study to evaluate the latest commercially available su-fURS devices. We have also incorporated an enhanced fluoroscopic element to maximize realism of the simulation. However, our study is not devoid of limitations. First and foremost, the in vitro environment can never fully replicate the actual surgical experience − stone fragmentation during lithotripsy, irrigation fluid contamination are aspects that we cannot simulate perfectly. We envision the assessment of stone fragmentation time via laser lithotripsy to be conducted in our future studies. The scale of our study is indubitably small as well, a larger sample size would have been ideal in reducing bias. Our practicing urologists are also relatively well-versed with the use of some su-fURS (e.g., Boston LithoVue) that were being tested, which may also contribute to an extent of familiarity with the scope. We also were not able to house all currently available su-fURS for our comparative assessment, such as the Wiscope® Single-Use Digital Flexible Ureteroscope or the Tianjin Guyufan Biological Technology Single-Use Video Ureteroscope.
Conclusion
Our in vitro study revealed noninferiority between the different single-use fURS models tested for subjective and objective performance. By testing on a validated and enhanced fluoroscopy-assisted standardized endourology model, this indirectly affirms that the in vivo choice of the most optimal su-fURS will depend on variables that define personal preference of the surgeon. We believe our paper is a timely addition to the ongoing discourse regarding su-fURS.
Statement of Ethics
The study protocol was approved by the National Healthcare Group Domain Specific Review Board, reference number: 2021/00924. All subjects were issued a participant information sheet and written informed consent was taken prior to commencement of the study.
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Funding Sources
This manuscript did not receive any funding.
Author Contributions
Wei Zheng So: conceptualization, methodology, formal analysis, and writing. Vineet Gauhar: review and editing. Kelven Chen: conceptualization, methodology, review, and editing. Jirong Lu: conceptualization and methodology. Wei Jin Chua: review and editing. Ho Yee Tiong: conceptualization, supervision, review, and editing.
Data Availability Statement
The data that supports the findings of this study are not publicly available due to information that may compromise the privacy of the research participants but are available upon request from the corresponding author Ho Yee Tiong.
Supplementary Material
Supplementary data
Acknowledgments
The authors would like to thank Boston Scientific, PUSEN Medical, REDPINE Medical, and SHANGHAI ANQING Medical for the provision of study equipment.
Funding Statement
This manuscript did not receive any funding.
References
- 1.Geavlete P, Multescu R, Geavlete B. Pushing the boundaries of ureteroscopy: current status and future perspectives. Nat Rev Urol. 2014 Jul;11((7)):373–382. doi: 10.1038/nrurol.2014.118. [DOI] [PubMed] [Google Scholar]
- 2.Buscarini M, Conlin M. Update on flexible ureteroscopy. Urol Int. 2008;80((1)):1–7. doi: 10.1159/000111721. [DOI] [PubMed] [Google Scholar]
- 3.Scotland KB, Chan JYH, Chew BH. Single-use flexible ureteroscopes: how do they compare with reusable ureteroscopes? J Endourol. 2019 Feb;33((2)):71–8. doi: 10.1089/end.2018.0785. [DOI] [PubMed] [Google Scholar]
- 4.Collins JW, Keeley FX, Jr, Timoney A. Cost analysis of flexible ureterorenoscopy. BJU Int. 2004 May;93((7)):1023–1026. doi: 10.1111/j.1464-410X.2003.04774.x. [DOI] [PubMed] [Google Scholar]
- 5.Ofstead CL, Heymann OL, Quick MR, Johnson EA, Eiland JE, Wetzler HP. The effectiveness of sterilization for flexible ureteroscopes: a real-world study. Am J Infect Control. 2017;45((8)):888–895. doi: 10.1016/j.ajic.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 6.Cho SY, Lee JY, Shin DG, Seo IY, Yoo S, Park HK. Evaluation of performance parameters of the disposable flexible ureterorenoscope (LITHOVUE) in patients with renal stones: a prospective, observational, single-arm, multicenter study. Sci Rep. 2018 Jun 28;8((1)):9795. doi: 10.1038/s41598-018-28247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eisel M, Strittmatter F, Ströbl S, Freymüller C, Pongratz T, Sroka R. Comparative investigation of reusable and single-use flexible endoscopes for urological interventions. Sci Rep. 2020 Mar 30;10((1)):5701. doi: 10.1038/s41598-020-62657-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bozzini G, Filippi B, Alriyalat S, Calori A, Besana U, Mueller A, et al. Disposable versus reusable ureteroscopes: a prospective multicenter randomized comparison. Res Rep Urol. 2021;13:63–71. doi: 10.2147/RRU.S277049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Y, Chen J, Zhu Z, Zeng H, Zeng F, Chen Z, et al. Comparison of single-use and reusable flexible ureteroscope for renal stone management: a pooled analysis of 772 patients. Transl Androl Urol. 2021 Jan;10((1)):483–493. doi: 10.21037/tau-20-1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quhal F, Seitz C. Guideline of the guidelines: urolithiasis. Curr Opin Urol. 2021;31((2)):125–129. doi: 10.1097/MOU.0000000000000855. [DOI] [PubMed] [Google Scholar]
- 11.Schlager D, Obaid MA, Hein S, Wilhelm K, Schönthaler M, Gratzke C, et al. Current disposable ureteroscopes: performance and limitations in a standardized kidney model. J Endourol. 2020 Oct;34((10)):1015–1020. doi: 10.1089/end.2020.0185. [DOI] [PubMed] [Google Scholar]
- 12.Blankstein U, Lantz AG, Honey RJDA, Pace KT, Ordon M, Lee JY. Simulation-based flexible ureteroscopy training using a novel ureteroscopy part-task trainer. Can Urol Assoc J. 2015;9((9–10)):331. doi: 10.5489/cuaj.2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doizi S, Kamphuis G, Giusti G, Andreassen KH, Knoll T, Osther PJ, et al. First clinical evaluation of a new single-use flexible ureteroscope (LithoVue™): a European prospective multicentric feasibility study. World J Urol. 2017 May;35((5)):809–818. doi: 10.1007/s00345-016-1936-x. [DOI] [PubMed] [Google Scholar]
- 14.Emiliani E, Mercadé A, Millan F, Sánchez-Martín F, Konstantinidis CA, Angerri O. First clinical evaluation of the new single-use flexible and semirigid Pusen ureteroscopes. Cent European J Urol. 2018;71((2)):208–213. doi: 10.5173/ceju.2018.1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston TJ, Baard J, de la Rosette J, Doizi S, Giusti G, Knoll T, et al. A clinical evaluation of the new digital single-use flexible ureteroscope (UscopePU3022): an international prospective multicentered study. Cent European J Urol. 2018;71((4)):453–461. doi: 10.5173/ceju.2018.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hendriks N, Henderickx MM, Schout BM, Baard J, van Etten-Jamaludin FS, Beerlage HP, et al. How to evaluate a flexible ureterorenoscope? Systematic mapping of existing evaluation methods. BJU Int. 2021;128((4)):408. doi: 10.1111/bju.15544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kam J, Yuminaga Y, Beattie K, Ling KY, Arianayagam M, Canagasingham B, et al. Single use versus reusable digital flexible ureteroscopes: a prospective comparative study. Int J Urol. 2019;26((10)):999–1005. doi: 10.1111/iju.14091. [DOI] [PubMed] [Google Scholar]
- 18.Meng C, Peng L, Li J, Li Y, Li J, Wu J. Comparison between single-use flexible ureteroscope and reusable flexible ureteroscope for upper urinary calculi: a systematic review and meta-analysis. Front Surg. 2021;8:691170. doi: 10.3389/fsurg.2021.691170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang F, Zhang X, Cui Y, Zhu Z, Li Y, Chen J, et al. Single-use vs. reusable digital flexible ureteroscope to treat upper urinary calculi: a propensity-score matching analysis. Front Surg. 2022 Jan 10;8:778157. doi: 10.3389/fsurg.2021.778157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Butticè S, Sener TE, Netsch C, Emiliani E, Pappalardo R, Magno C. LithoVue™: a new single-use digital flexible ureteroscope. Cent European J Urol. 2016;69((3)):302. doi: 10.5173/ceju.2016.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Proietti S, Dragos L, Molina W, Doizi S, Giusti G, Traxer O. Comparison of new single-use digital flexible ureteroscope versus nondisposable fiber optic and digital ureteroscope in a cadaveric model. J Endourol. 2016;30((6)):655–659. doi: 10.1089/end.2016.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis NF, McGrath S, Quinlan M, Jack G, Lawrentschuk N, Bolton DM. Carbon footprint in flexible ureteroscopy: a comparative study on the environmental impact of reusable and single-use ureteroscopes. J Endourol. 2018 Mar;32((3)):214–217. doi: 10.1089/end.2018.0001. [DOI] [PubMed] [Google Scholar]
- 23.So WZ, Wang Z, Tiong HY. Disposable or reusable flexible ureterorenoscopy for renal calculi: cost remains as the deciding factor. World J Urol. 2022 May;40((5)):1267–1268. doi: 10.1007/s00345-021-03867-3. [DOI] [PubMed] [Google Scholar]
- 24.Mager R, Kurosch M, Höfner T, Frees S, Haferkamp A, Neisius A. Clinical outcomes and costs of reusable and single-use flexible ureterorenoscopes: a prospective cohort study. Urolithiasis. 2018 Nov;46((6)):587–593. doi: 10.1007/s00240-018-1042-1. [DOI] [PubMed] [Google Scholar]
- 25.Taguchi K, Usawachintachit M, Tzou DT, Sherer BA, Metzler I, Isaacson D, et al. Micro-costing analysis demonstrates comparable costs for LithoVue compared to reusable flexible fiberoptic ureteroscopes. J Endourol. 2018 Apr;32((4)):267–273. doi: 10.1089/end.2017.0523. [DOI] [PubMed] [Google Scholar]
- 26.Ventimiglia E, Godínez AJ, Traxer O, Somani BK. Cost comparison of single-use versus reusable flexible ureteroscope: a systematic review. Turk J Urol. 2020 Nov;46((Suppl 1)):S40–5. doi: 10.5152/tud.2020.20223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Compernolle D, Veys R, Elshout PJ, Beysens M, Van Haute C, De Groote L, et al. Reusable, single-use, or both: a cost efficiency analysis of flexible ureterorenoscopes after 983 cases. J Endourol. 2021 Oct;35((10)):1454–1459. doi: 10.1089/end.2021.0006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Data Availability Statement
The data that supports the findings of this study are not publicly available due to information that may compromise the privacy of the research participants but are available upon request from the corresponding author Ho Yee Tiong.


