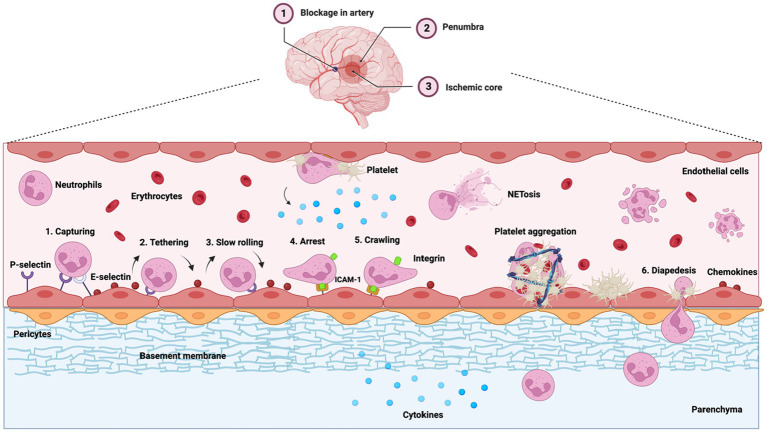
Figure 1.
Leukocyte (neutrophil) extravasation and infiltration during inflammation are major contributors to poor ischemia outcomes. Middle cerebral artery occlusion is illustrated. During inflammation, cytokines (IL-1β, IL-6, and TNF-α) and the chemokines (MIP-1, MIP-2, and MCP-1) are upregulated, which stimulate the expression of selectins and ICAM-1 on the endothelial surface near the ischemic area. Chemokines (blue dots) are transcytosed through or deposited on the endothelium. E-selectin and P-selectin capture neutrophils from the blood flow, pulling the tethers at the rear of neutrophils and initiating their rolling motion. This activates integrins on neutrophils that firmly attach to ICAM-1, causing neutrophil adhesion. Neutrophils also recruit platelets, causing platelet aggregation and blocking the flow of red blood cells (erythrocytes). Neutrophils then infiltrate into the perivascular space through diapedesis while continuing to release pro-inflammatory factors into the ischemic area, causing neuronal damage.