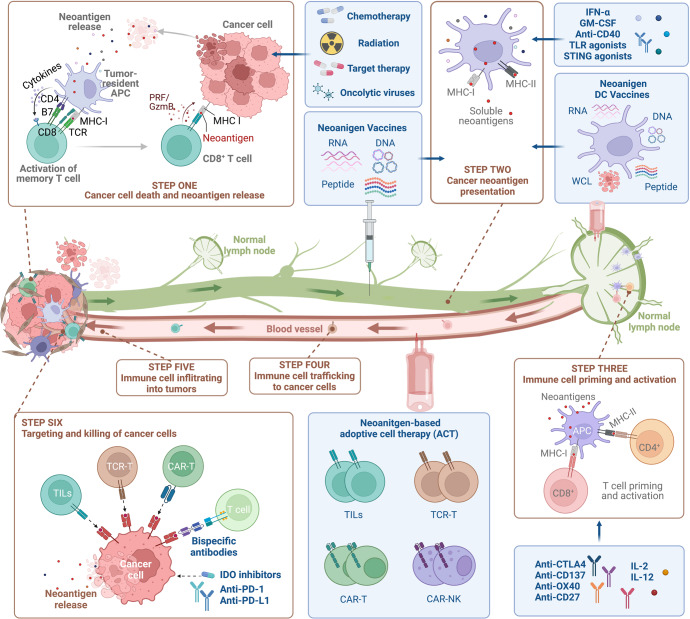
Fig. 6.
Combinational neoantigens-based anti-tumor strategies. The “Cancer-Immunity Cycle” refers to the sequential events that must be initiated, proceeded, and expanded to achieve an anti-cancer immune response, resulting in the efficient eradication of cancer cells. Briefly, neoantigens generated by oncogenesis are released and captured by DCs (step 1). DCs convey the collected neoantigens on MHC-I and MHC-II molecules to T cells (step 2), resulting in priming and activation of effector T cell responses against cancer-specific neoantigens (step 3). Subsequently, activated effector T cells migrate to (step 4) and infiltrate into (step 5) the tumor bed, where they recognize and finally destroy their target cancer cells (step 6). The death of cancer cells produces additional tumor-associated neoantigens (step 1 once more), which broadens and intensifies the immune response in subsequent cycles. Therefore, cancer immunotherapies have been designed to reinitiate or amplify a self-sustaining cycle of cancer immunity. Multiple immunotherapies have been developed to target the rate-limiting steps in “Cancer-Immunity Cycle”, including enhancing the neoantigen release by chemotherapy, radiation therapy and oncolytic virus, increasing the quantity and quality of tumor-reactive T cells through cancer vaccine and ACTs, and boosting the infiltration and cytotoxicity efficacy of immune cells via checkpoints inhibitors