Abstract
Recent evidence has shown an increase in recurrence and a decrease in overall survival in patients treated with laparoscopic radical hysterectomy (LRH) and robotic assisted radical hysterectomy (RRH) open techniques (ORH). In addition, several high quality trials were recently published regarding the laparoscopic treatment of early stage cervical cancer. We sought out to reassess the recurrence rates, overall survival, complications and outcomes associated with laparoscopic radical hysterectomy (LRH) techniques against open techniques (ORH) when robotic assisted techniques were excluded. We searched PubMed, Medline, Cochrane CENTRAL, SCOPUS, ClinicalTrials.Gov and Web of Science for relevant clinical trials and observational studies. We included all studies that compared with early stage cervical cancer receiving LRH compared with ORH. We included randomized clinical trials, prospective cohort, and retrospective cohort trials. We included studies that included LRH and RRH as long as data was available to separate the two arms. We excluded studies that combined LRH and RRH without supplying data to differentiate. Of 1244 total studies, we used a manual three step screening process. Sixty studies ultimately met our criteria. We performed this review in accordance with PRISMA guidelines. We analyzed continuous data using mean difference (MD) and a 95% confidence interval (CI), while dichotomous data were analyzed using odds ratio (OR) and a 95% CI. Review Manager and Endnote software were utilized in the synthesis. We found that when excluding RRH, the was no significant difference regarding 5-year overall Survival (OR = 1.24 [0.94, 1.64], (P = 0.12), disease free survival (OR = 1.00 [0.80, 1.26], (P = 0.98), recurrence (OR = 1.01 [0.81, 1.25], (P = 0.95), or intraoperative complications (OR = 1.38 [0.94, 2.04], (P = 0.10). LRH was statistically better than ORH in terms of estimated blood loss (MD = − 325.55 [− 386.16, − 264.94] (P < 0.001), blood transfusion rate (OR = 0.28 [0.14, 0.55], (P = 0.002), postoperative complication rate (OR = 0.70 [0.55, 0.90], (P = 0.005), and length of hospital stay (MD = − 3.64[− 4.27, − 3.01], (P < 0.001). ORH was superior in terms of operating time (MD = 20.48 [8.62, 32.35], (P = 0.007) and number of resected lymph nodes (MD = − 2.80 [− 4.35, − 1.24], (P = 0.004). The previously seen increase recurrence and decrease in survival is not seen in LRH when robotic assisted techniques are included and all new high quality is considered. LRH is also associated with a significantly shorter hospital stay, less blood loss and lower complication rate.
Prospero Prospective Registration Number: CRD42022267138.
Subject terms: Cervical cancer, Outcomes research
Introduction
Cervical cancer is the third most common malignancy and the second most common cause of death from cancer among women in the USA1. The incidence and mortality of cervical cancer have a large geographic variation as it is more common and more fatal in developing countries2. Cervical cancer is classified into early-stage and advanced-stage cancer3. Although staged clinically, the surgical treatment of early-stage cervical treatment is critical for optimizing patient survival4,5. Radical hysterectomy with pelvic lymphadenectomy is a commonly performed procedure for the treatment of cervical cancer6. Patients who are found to be candidates for surgical intervention may see 5-year survival rate increased to as high as 87%7. Abdominal, laparoscopic, robotic-assisted laparoscopic and vaginal approaches to radical hysterectomy have all been described and performed by many authors8. Secondary to the risk of spreading cancers, several authors have stated that gynecologic oncology has been slower to adopt minimally invasive techniques than other specialties, sometimes reserving these techniques for only risk reducing procedures9. The first laparoscopic radical hysterectomy was performed in 199310 and since that time the minimally invasive surgery (both laparoscopic and robotic-assisted laparoscopic) have been increasingly used.11,12. Over the last two decades, many studies have compared the survival outcomes and operative morbidity of the minimally invasive and open surgery for the management of cervical cancer13. Open radical hysterectomy shows significant morbidity including bladder dysfunction, blood loss, and complications of blood transfusion14. Many retrospective studies15–19 have shown that laparoscopic surgery causes perioperative complications less than open surgery. Complicating this, a recent randomized clinical multicenter trial proved that minimally invasive surgery was accompanied by a high rate of recurrence and a worse disease-free survival rate than open surgery20. In addition, a recent retrospective study that included 2461 patients with cervical cancer showed that minimally invasive surgery is associated with a higher risk of death than open surgery21. The culmination of these results was a change in the National Comprehensive Cancer Network (NCCN) guidelines with regards to minimally invasive radical hysterectomy22. The current NCCN guidelines and European Society of Gynaecological Oncology (ESGO) guidelines recommended that the standard surgical approach for management of early-stage cervical cancer is abdominal radical hysterectomy23.
In addition to this recent evidence against minimally invasive radical hysterectomy techniques, several new high quality trials regarding LRH and RRH have been published. For this reason, we were motivated to investigate LRH versus ORH while excluding robotic assisted techniques. We conducted this meta-analysis with late breaking, high quality data to again compare the efficacy and safety of laparoscopic radical hysterectomy with that of open radical hysterectomy for the management of cervical cancer. We have meticulously excluded all robotic assisted cases, and attempted to obtain data to use as many high quality trials as possible, while excluding robotic assisted cases.
Method
This meta-analysis was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)24 and the guidelines reported in the Cochrane Handbook for Systematic Reviews of Interventions25.
Eligibility criteria
The inclusion criteria included studies that met all of the following:
Population: women with early stage cervical cancer
Intervention: Laparoscopic radical hysterectomy (LRH)
Comparator: Open radical hysterectomy (ORH)
Included Study Designs: randomized clinical trials, prospective cohort, and retrospective cohort studies.
And included at least one of our primary or secondary outcomes.
Primary outcomes included:
(1.) Operative time, (2.) Estimated blood loss, (3.) Rate of intraoperative complications, (4.) Rate of postoperative complications, (5.) Rate of blood transfusions.
Secondary outcomes included:
(1.) Rate of recurrence, (2.) Postoperative or intraoperative mortality (defined as within 90 days of surgery), (3.) Five-year survival rate, (4.) Disease-free survival rate, (5.) Number of resected lymph nodes.
We made all efforts to obtain all data possible from all included studies in order to include as many high quality trials as possible, but ultimately excluded those trials that failed our inclusion critieria because they did not publish, or despite our best efforts we could not obtain the necessary data to differentiate which cases included robotic assistance and which did not. We excluded all secondary works, such as meta-analyses and reviews, all animal studies, conference abstracts, and studies with incomplete reported data.
Search and study selection
We searched PubMed, Medline, Scopus, Web of Science, ClinicalTrials.Gov and Cochrane CENTRAL databases from database inception until January 2nd 2022 for articles that matched our inclusion criteria.
We used the following search strategy in our search: (laparoscopic OR laparoscopy) AND (open OR abdominal) AND ((cervical cancer) OR (cancer cervix)) AND (hysterectomy). We screened the included articles in three steps. The first step implied importing the results from electronic databases to a Microsoft Excel26 sheet using EndNote Software27. The second step included a manual title and abstract screening of the articles imported to the Excel sheet. The third step was the full-text screening of the included citations from step 2. Additionally, we manually searched the references of the included papers for possible missed studies. Two researchers separately performed the literature search and eligibility match. Disagreements in the included studies was reached by consensus. A third member of the research team was assigned to settle disputes if consensus could not be reached on any study's eligibility, but was ultimately never needed.
Data collection
We collected three categories of data from each included study: the first category is the baseline and demographic characteristics of the included participants, such as the author, year, country, sample size, age, BMI, included stages, follow up period, time period, adenocarcinoma, squamous cell carcinoma, and positive lymph nodes. The second category included the outcomes of analysis, mainly: Operative time, estimated blood loss, Intraoperative complication, Postoperative complication, Blood transfusion rate, Recurrence, mortality, Five-year survival rate, Disease-free survival, and Resected lymph nodes. The third category included data for risk of bias assessment. The process of data collection was done using Microsoft Excel26.
Risk of bias assessment
We used the quality assessment tools from the National Heart, Lung, and Blood Institute (NHLB) to assess the risk of bias of observational studies28. We followed The Grading of Recommendations Assessment, Development and Evaluation (GRADE) Guidelines in assessing the quality of this study. We assessed the risk of bias of included trials using Cochrane’s risk of bias tool29. The tool assesses proper randomization of patients, allocation concealment, and adequate blinding through seven domains. Each domain was judged to be either “low”, “unclear”, or “high” risk of bias. The details of the GRADE assessment of each outcome can be found in Supplementary Table S1.
Analysis
We performed the meta-analysis of this study using Review Manager Software27. Our study included continuous and dichotomous outcomes. We analyzed continuous data using mean difference (MD) and 95% confidence interval (CI), while dichotomous data were analyzed using odds ratio (OR) and 95% CI. The fixed-effects model was used when data were homogeneous, while heterogeneous data were analyzed under a random-effects model. To measure the presence of inconsistency among the studies, we used the I2 and the p-value of the Chi-square tests30. Values of P < 0.1 or I2 > 50% were significant indicators of the presence of heterogeneity. We tried to solve the inconsistency of heterogeneous outcomes using Cochrane’s leave-one-out method30.
Ethics approval and consent to participate
This Manuscript has been reviewed by the institutional IRB board at Marchand Institute and was found to be exempt from IRB review. (January 2022). Data used was exempt from consent to participate or publish secondary to the nature of the study being a systematic review, retrospectively looking at previously published data.
Commitment to diversity
The Marchand Institute remains committed to diversity and tolerance in its research, and actively maintains a workplace free of racism and sexism. Greater than half of the authors for this study are female and many represent diverse backgrounds and under-represented ethnic groups.
Results
Summary of included studies
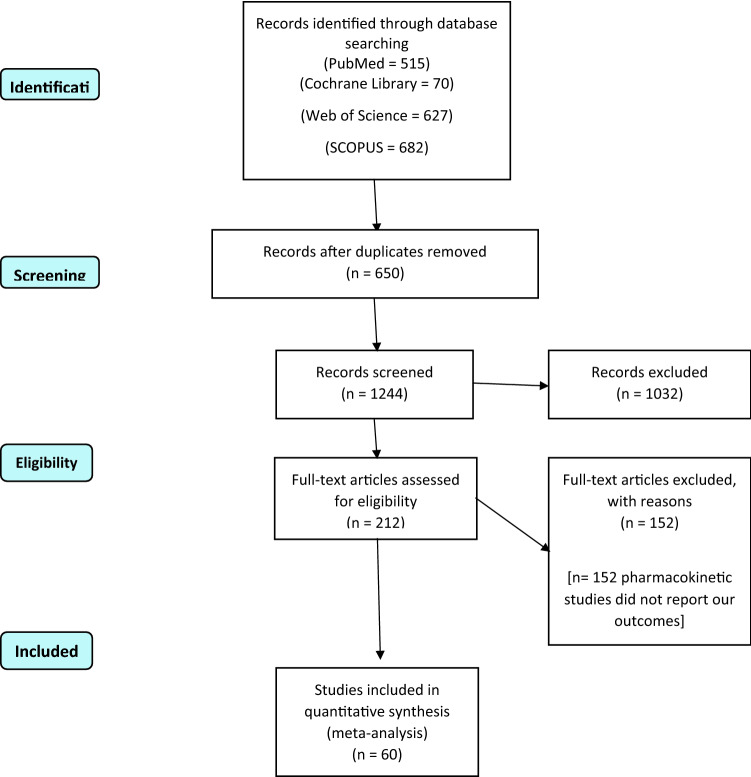
The literature search results are illustrated in the PRISMA flow diagram in Fig. 1. We included sixty studies that met our eligibility criteria from the different databases11,15,16,31–87. We analyzed 42,994 patients with cervical cancer in different stages according to FIGO staging (2009 edition)3. A total of 15,995 patients were allocated to the laparoscopic group, while 26,999 patients were allocated to the laparotomy group. The mean age of patients in the laparoscopic group and laparotomy group was 46.5 and 46.7 years, respectively. A summary of the included studies, the demographic data of patients, the included stages, and follow-up duration are described in detail in Tables 1 and 2.
Figure 1.
PRISMA flow diagram of our literature search.
Table 1.
Summary of the included studies.
| Study ID | Country | Study design | Included stages | Follow up (mo), (median) | Time period | Sample size, n | |
|---|---|---|---|---|---|---|---|
| LH | OH | ||||||
| Abu-Rustum 2003 | USA | Retrospective cohort | IA1, 2–IB1 | NR | 2000–2002 | 19 | 195 |
| Anagnostopoulos 2017 | UK | Retrospective cohort | IA2–IIA1–IB1 | 36 | 2011–2013 | 36 | 36 |
| Anchora 2019 | Italy | Retrospective cohort | IA1 | 49 | 2016 | 206 | 217 |
| Bogani 2014 | Italy | Prospective cohort | IA2, IIA, IB2, IIB | 36 | 2004–2011 | 65 | 65 |
| Bogani 2020 | Italy | Retrospective matched | IB1–IIA | 59 | 2013–2014 | 70 | 35 |
| Campos 2013 | Brazil | Clinical trial | IA2–IB | NR | 1999–2004 | 16 | 14 |
| Campos 2021 | Brazil | Clinical trial | IA2–IB–IIA | 60 | 1990–2004 | 16 | 14 |
| Chen 2014 | Taiwan | Retrospective cohort | IA–IIB | NR | 2005–2013 | 32 | 44 |
| Chen 2019 | China | Retrospective cohort | IB1 | 50 | 2010–2018 | 129 | 196 |
| Chen 2020 | China | Retrospective cohort | IB1 | 36 | 2004–2016 | 963 | 1634 |
| Chen 2021 | Italy | Retrospective matched | IB1 | 42 | 2008–2018 | 87 | 174 |
| Corrado 2018 | Italy | Retrospective cohort | IB1 | 82 | 2001–2016 | 152 | 101 |
| Estape 2009 | USA | Retrospective cohort | IA2, IB1, IB2 | 45 | 2006–2008 | 17 | 14 |
| Ditto 2015 | Italy | Retrospective cohort | IA2–IB1 | 40 | 2002–2013 | 60 | 60 |
| Frumovitz 2007 | USA | Retrospective cohort | IA1, 2–IB1, 2 | 13 | 2004–2006 | 35 | 54 |
| Ghezzi 2007 | Italy | Retrospective cohort | IA2, IIA, IB1, IB2 | 58 | 2004–2007 | 50 | 48 |
| Gil-Moreno 2018 | Spain | Prospective cohort | IA2, IIA2–IB1, IIB | 112 | 1999–2016 | 90 | 76 |
| Gortchev 2012 | Bulgaria | Retrospective cohort | IB1 | 26 | 2006–2010 | 46 | 175 |
| Guangyi 2007 | China | Retrospective cohort | IB–IIA | 26 | 1998–2005 | 90 | 35 |
| Guo 2018 | China | Retrospective cohort | IA–IIA | 39 | 2000–2003 | 412 | 139 |
| He 2020 | China | Retrospective matched | IA1–IA2–IB1 | 42 | 2004–2016 | 739 | 739 |
| Kanao 2019 | Japan | Retrospective cohort | IB1–IIB | 30 | 2014–2017 | 80 | 83 |
| Kim 2018 | Korea | Retrospective | NR | NR | 2011–2014 | 3100 | 3235 |
| Kim 2019 | Korea | Retrospective cohort | IB1–IB2 | 59.1 | 2000–2018 | 122 | 122 |
| Kim 2020 | Korea | Retrospective cohort | Ia1—IIa1–Ib1–Ib2–IIa2 | NR | 2006–2016 | 26 | 22 |
| Kong 2014 | Korea | Retrospective cohort | IB–IIA | 28/58 | 2006–2013 | 40 | 48 |
| Lambaudie 2010 | France | Prospective Cohort | IA1, IA2, IB1 | NR | 2007–2009 | 16 | 22 |
| Laterza 2016 | Italy | Retrospective cohort | IA1, IA2, IB1, IIA2 | 121.2/43.6 | 1997–2015 | 82 | 68 |
| Lee 2002 | Taiwan | Prospective cohort | IA2–IB | 60 | 2002 | 30 | 30 |
| Lee 2011 | Korea | Retrospective cohort | IA2, IIA, IB1, IB2 | 78 | 1994–2001 | 24 | 48 |
| Li 2021 | China | Retrospective cohort | IA2–IB1–IIA1 | 33 | 2009–2016 | 546 | 661 |
| Liang 2019 | China | Retrospective cohort | IA1–IA2–IB1–IB2–IIA1–IIA2–IIB | NR | 2004–2015 | 5491 | 12,956 |
| Lim 2019 | Singapore | Prospective cohort | IA1–IIA | 29 (0–79) | 2009–2014 | 51 | 85 |
| Liu 2019 | China | Retrospective cohort | IB1–IB2 | NR | 2001–2015 | 271 | 135 |
| Malzoni 2009 | Italy | Retrospective cohort | IA1 with LVSI–IB | 53 (4–89) | 1995–2007 | 65 | 62 |
| Margina 2008 | USA | Prospective cohort | IB, IC, IIA, IIB, IIIC | 40 | 1993–2006 | 31 | 35 |
| Mendivil 2016 | USA | Retrospective cohort | IA2–IIB | 39 | 2009–2013 | 39 | 49 |
| Naik 2010 | UK | Clinical trial | IB1 | NR | 2005–2007 | 7 | 6 |
| Nam 2012 | Korea | Retrospective cohort | IA2–IIA | 92 | 1997–2008 | 263 | 263 |
| Paik 2019 | Korea | Retrospective cohort | IB–IIA | 63.6 | 2000–2008 | 133 | 605 |
| Park 2013 | Korea | Retrospective cohort | IB2–IIA2 | 33 | 1997–2011 | 31 | 30 |
| Park 2016 | Korea | Retrospective cohort | IA2–IIA | 58.8 | 1997–2013 | 186 | 107 |
| Qin 2020 | NR | Retrospective cohort | IA1, IA2, IB1 | 59 | 59 | 172 | 84 |
| Rodriguez 2021 | Colombia | Retrospective cohort | IA1–IIA2–IIB1 | 52.35 | 2006–2017 | 681 | 698 |
| Sert 2011 | Norway | Retrospective cohort | IA1–IB1 /IA1–IB1 | 63.2 | 2005–2009 | 7 | 26 |
| Shanmugam 2020 | India | Retrospective cohort | IA1, IA2, IB1, IB | 33.5 | 2012–2018 | 82 | 89 |
| Sharma 2006 | England | Retrospective cohort | IA2–IIB | 38.25 | 1999–2005 | 35 | 32 |
| Soliman 2011 | Brazil | Retrospective cohort | NR | NR | 2007–2010 | 31 | 30 |
| Steed 2004 | Canada | Retrospective cohort | IA–IB | 20 | 1996–2003 | 71 | 205 |
| Suh 2015 | Korea | Retrospective cohort | IA2–IIA | 44 | 2003–2011 | 55 | 106 |
| Taylor 2011 | USA | Retrospective cohort | IA2–IB1 /IA2–IB1 | NR | 2003–2009 | 9 | 18 |
| Topatas 2014 | Turkey | Retrospective cohort | IA2–IB2 | 43 | 2007–2010 | 22 | 46 |
| Wang 2019 | China | Retrospective cohort | IA1, IA2, IB1, IB | 41.3 (6–193.5) | 2001–2015 | 217 | 179 |
| Wright 2012 | USA | Retrospective cohort | NR | NR | 2006–2010 | 217 | 1610 |
| Xiao 2015 | China | Retrospective cohort | IA–IIB | 106 | 48 | ||
| Xiao 2016 | China | Retrospective cohort | IA–IIA | 48.6 | 2001–2014 | 42 | 16 |
| Xu 2020 | China | Clinical trial | IA1, IA2, IB1, IB | NR | NR | 84 | 84 |
| Yuan 2019 | China | Retrospective cohort | IA2–IB2 | 64 | 2012–2014 | 99 | 99 |
| Zhang 2017 | China | Retrospective cohort | IA2–IIB | 54 | 2008–2012 | 35 | 42 |
| Zhao 2021 | China | Retrospective cohort | IA2–IIA2 | 60 | 2013–2016 | 148 | 939 |
NR not reported, mo month.
Table 2.
Baseline characteristics of participants.
| Study ID | Age (years), (mean, SD) (median, range) | BMI, (mean, SD) (median, range) | Squamous n (%) | Adenocarcinoma n (%) | Positive lymph nodes n (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| LH | OH | LH | OH | LH | OH | LH | OH | LH | OH | |
| Abu-Rustum 2003 | 42.6 (30–69) | 43.6 (20–85) | 23.1 (18–30) | 24.6 (18–40) | 10 (53%) | 132 (67%) | 7 | 55 | NR | NR |
| Anagnostopoulos 2017 | 44.6 (12.2) | 41.2 (12.7) | 25.8 (3.8) | 26.4 (4.7) | 25 (69%) | 20 (55%) | 11 (31%) | 16 (45%) | NR | NR |
| Anchora 2019 | 46 (19–85) | 46 (26–83) | 29 (17–40) | 26 (18–39) | 139 (67.5) | 141 (65.0 | 67 (32.5) | 76 (35.0) | 17 (8.3) | 43 (19.8) |
| Bogani 2014 | 48.9 (± 13.5) | 50.9 (± 14) | 25.1 (± 5.2) | 25.9 (± 6.1) | 20 (31%) | 22 (34%) | 45 (69%) | 43 (66%) | 18 (28%) | 17 (26%) |
| Bogani 2020 | 45 (25–82) | 45 (25–68) | 22.4 (15.8–39.8) | 23.1 (15.7–33.3) | 24 (68%) | 59 (84%) | 7 (20%) | 8 (11%) | 10 (28%) | 28 (40%) |
| Campos 2013 | 36.19 ± 9.78 | 39.64 ± 6.23 | NR | NR | 12 (75%) | 12 (86%) | 4 (25%) | 2 (14%) | NR | NR |
| Campos 2021 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Chen 2014 | 51.2 (11.9) | 51.9 (11.3) | 23.2 (3.4) | 24.9 (4.6) | 26 (81.3) | 33 (75) | 1 (3.1) | 1 (2.3) | 3 (9.4) | 9 (20.5) |
| Chen 2019 | 49.29 ± 9.31 | 51.69 ± 10.25 | 22.99 ± 3.29 | 22.98 ± 3.14 | 103 (79.84) | 165 (84.18) | 19 (14.73) | 23 (11.73) | 1 (0.78) | 11 (5.61) |
| Chen 2020 | 47.0 ± 9.3 | 46.7 ± 9.6 | NR | NR | 784 (100%) | 1393 (100%) | 0 | 0 | 78 (9.9%) | 106 (7.6%) |
| Chen 2021 | 49.00 ± 12.00 | 48.00 ± 14.00 | NR | NR | 66 (75.86) | 140 (80.46) | 18 (20.69) | 27 (15.52) | 4 (4.60) | 8 (4.60) |
| Corrado 2018 | 45 (23–78) | 50 (28–76) | 23.5 (17–35) | 24.8 (18–51) | 110 (72.3%) | 68 (67.3%) | 37 (24.3%) | 23 (22.8%) | 148 (97.3%) | 97 (96%) |
| Estape 2009 | 52.8 (4.8) | 42 (12) | 28.1 (4.8) | 29.5 (6.4) | 11 (64.7%) | 10 (71.4%) | 6 (35.3%) | 2 (14.3%) | NR | NR |
| Ditto 2015 | 46 (29.79) | 45.5 (15.78) | 24.3 (2.9) | 24.0 (4.3) | 36 (60%) | 35 (58%) | 24 (40%) | 25 (42%) | 3 (5%) | 6 (10%) |
| Frumovitz 2007 | 40.8 (28–63) | 42.5 (27–68) | 28.1 (18–40) | 28.2 (17–46) | 15 | 33 | 17 | 16 | NR | NR |
| Ghezzi 2007 | 47 (24–78) | 53 (28–75) | 23 (17.4–35) | 25 (19–43) | 38 (76%) | 33 (68.7%) | 7 (14%) | 13 (27.1%) | 7 (14%) | 9 (18.7%) |
| Gil-Moreno 2018 | 46.31 (11.04) | 50.5 (13.6) | 26 (18–38) | 26.5 (18–40) | 57 (63.3) | 47 (61.8) | 27 (30) | 23 (30.2) | 10 (11.11) | 12 (15.79) |
| Gortchev 2012 | 42.5 ± 9.9 | 49.0 ± 11.0 | NR | NR | 41 (89.1%) | 167 (95.4%) | 5 (10.9%) | 8 (4.6%) | 5 (10.9%) | 42 (24.0%) |
| Guangyi 2007 | 42 ± 9 | 44 ± 11 | NR | NR | 81 | 25 | 5 | 4 | 18 | 4 |
| Guo 2018 | 44.19 (25–76) | 40.52 (23–62) | 22.81 (14.33–35.61) | 23.19 (13.88–36.63) | 340 (82.52) | 110 (79.14) | 72 (17.48) | 29 (20.86) | 53 (12.86) | 20 (14.39) |
| He 2020 | 46.80 ± 9.460 | 46.69 ± 9.367 | NR | NR | 641 | 641 | 89 | 89 | 71 | 71 |
| Kanao 2019 | 44.0 ± 10.2 | 49.0 ± 11.5 | 20.5 (19.1–23.3) | 21.4 (19.7–23.7) | 37 (46.3) | 44 (53.0) | 43 (53.7) | 39 (47.0) | 9 (11.2) | 12 (14.5) |
| Kim 2018 | 40 sd is NR | 45 | NR | NR | NR | NR | NR | NR | NR | NR |
| Kim 2019 | 49.5 ± 11.2 | 49.0 ± 11.0 | 148 (66.7) | 167 (75.2) | 62 (27.9) | 42 (18.9) | 19 (8.6) | 23 (10.4) | ||
| Kim 2020 | 48.77 (11.82) | 53.82 (11.13) | 23.80 (3.47) | 24.43 (2.77) | 21 (80.8) | 15 (68.2) | 5 (19.2) | 6 (27.3) | NR | NR |
| Kong 2014 | 45.0 ± 10.6 | 48.0 ± 11.0 | 22.3 ± 2.9 | 23.4 ± 3.3 | 30 (75.0) | 39 (81.3) | 7 (17.5) | 7 (14.6) | 7 (17.5) | 8 (16.7) |
| Lambaudie 2010 | 45 (32–57) | 53 (31–72) | 21.9 (14.3–39.4) | 21.9 (17.2–34) | 11 (68.7%) | 17 (85.0%) | 4 (25.0%) | 3 (15.0%) | NR | NR |
| Laterza 2016 | 43 (24–77) | 48 (26–85) | 23.44 (16.9–39.76) | 24.52 (19.3–43.3) | NR | NR | NR | NR | 2 (2.4) | 1 (1.6) |
| Lee 2002 | 46.2 ± 7.2 | 48.0 ± 6.8 | NR | NR | 27 | 25 | 3 | 5 | 14 | 5 |
| Lee 2011 | 48.4 (39–68) | 50.2 (34–67) | 23.4 (18.2–32.4) | 23.9 (15.8–34.6) | 19 (79.2%) | 38 (79.2%) | 4 (16.7%) | 8 (16.7%) | 4 (16.7%) | 10 (20.8%) |
| Li 2021 | 46.94 ± 9.367 | 47.03 ± 9.354 | NR | NR | 451 (85.6) | 565 (58.48) | 82 (15.02) | 78 (11.8) | 51 (9.34) | 46 (6.96) |
| Liang 2019 | NR | NR | NR | NR | 4691 (85.4) | 11,404 (88) | 559 (10.2) | 1006 (7.8) | NR | NR |
| Lim 2019 | 47 (28–70) | 49 (30–70) | 22.9 (12.9–33.7) | 23.4 (14.7–33.9) | 21 (41.2) | 50 (58.8) | 25 (49.0) | 27 (31.8) | 7 (13.7) | 12 (14.1) |
| Liu 2019 | 42.9 ± 9.1 | 42.6 ± 7.9 | 23.1 ± 2.8 | 23.7 ± 3.0 | 217 (80.1) | 119 (88) | 42 (15.5) | 12 (8.9) | 42 (15.5) | 15 (11.1) |
| Malzoni 2009 | 40.5 ± 7.7 | 42.7 ± 8.6 | 26 (19–35) | 29 (19–35) | 56 (86) | 53 (85) | 7 (10.5) | 6 (10) | 23.5 ± 5.1 | 25.2 ± 6.2 |
| Margina 2008 | 54.9 (14.3) | 50.9 (8.6) | 26.8 (4.6) | 27.3 (5.8) | 12 | 14 | 6 | 7 | NR | NR |
| Mendivil 2016 | 47.8 ± 12.02 | 51.3 ± 12.48 | 27.9 ± 5.71 | 29.2 ± 6.00 | 38 (69) | 27 (77) | 9 (18) | 5 (12.8) | NR | NR |
| Naik 2010 | 38.5 (33.5–53.5) | 37 (29.5–46) | 24.8 ± 1.3 | 25.0 ± 1.8 | 6 (85) | 5 (83) | 1 (14) | 1 (16) | NR | NR |
| Nam 2012 | 46.4 | 46.5 | 23.9 | 23.2 | 214 (81.4) | 207 (78.7) | 41 (15.6) | 46 (17.5) | 252 (95.8) | 252 (95.8) |
| Paik 2019 | 45.2 ± 10.8 | 48.9 ± 11.2 | NR | NR | 91 (68.4) | 453 (74.9) | 42 (31.6) | 152 (25.1) | 0 | 0 |
| Park 2013 | 48.5 (25–77) | 48.1 (25–84) | 23.1 (15.6–34.8) | 23.7 (17.6–34.7 | 90 (78.3) | 154 (81.9) | 25 (21.7) | 34 (18.1) | 46 (40) | 71 (37.8) |
| Park 2016 | 45.3 (27–71) | 47.3 (28–73) | 23.69 (17.1–34.9) | 23.58 (17.1–35.9) | 0 (0) | 0 (0) | 186 (100) | 107 (100%) | 29 (15.6) | 16 (15.0) |
| Qin 2020 | 44.3 ± 8.2 | 42.8 ± 8.3 | 23.1 ± 2.8 | 23.2 ± 3.0 | 72 (85.7) | 72 (85.7) | 35 (20.3) | 35 (20.3) | 15 (8.7) | 9 (10.7) |
| Rodriguez 2021 | NR | NR | NR | NR | 451 (66.2%) | 462 (66.3%) | 206 (30.3%) | 208 (29.8%) | 77 (11.3) | 56 (8) |
| Sert 2011 | 45.0 ± 12.9 | 44.8 ± 11.8 | 22.5 ± 1.84 | 25 ± 3.0 | 5 (71.4) | 19 (73) | 2 (28.6) | 6 (23) | NR | NR |
| Shanmugam 2020 | 52.5 | 50.3 | NR | NR | 74 (43.3%) | 79 (46.2%) | 7 (4.1%) | 7 (4.1%) | 7 (12.1%) | 4 (6.8%) |
| Sharma 2006 | 43.4 (28–60) | 42.8 (28–66) | NR | NR | 18 (51.4) | 16 (50) | 9 (25.7) | 11 (34.3) | NR | NR |
| Soliman 2011 | 44.2 (23.55–64.9) | 48.1 (25.5–82.2) | 29.5 (18.7–47.8) | 26.2 (20.9–44.5) | 16 (51.6) | 13 (43.33) | 12 (38.7) | 16 (53.3) | 3 (10) | 9 (31) |
| Steed 2004 | 43 (30–69) | 44 (24–86) | NR | NR | 31 (44) | 111 (54) | 40 (56) | 94 (46) | 5 (7) | 18 (9) |
| Suh 2015 | 49.1 ± 11.3 | 48.7 ± 11 | 23.1 ± 3.25 | 23.55 ± 3.7 | NR | NR | NR | NR | 5 (9) | 39 (36.8) |
| Taylor 2011 | 41.4 (31–60) | 41.1 (25–61) | 26.3 (20.6–36.1) | 26.9 (17–38.3) | 5 (55.5) | 11 (61.1) | 4 (44.44) | 7 (38.88) | NR | NR |
| Topatas 2014 | 46.5 (40–57) | 50 (46–58) | 18 (81.8) | 29 (63.0) | 1 (4.6) | 5 (10.9) | 2 (9.1) | 3 (6.7) | ||
| Wang 2019 | 45.95 ± 7.331 | 44.76 ± 7.743 | 23.25 ± 2.629 | 23.56 ± 3.286 | 188 (86.6) | 160 (89.4) | 25 (11.5) | 9 (5.0) | 87 (40.1) | 71 (39.7) |
| Wright 2012 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Xiao 2015 | 43.7 ± 9.3 | 45.7 ± 11.3 | 23.8 ± 3.9 | 24.7 ± 3.8 | 96 (90.6%) | 42 (87.5%) | 6 (5.7%) | 5 (10.4%) | 9 (8.5%) | 9 (18.8%) |
| Xiao 2016 | 47.1 ± 9.9 | 55.1 ± 7.6 | 23.0 ± 3.0 | 23.8 ± 2.6 | 42 (100) | 16 (100) | 0 (0) | 0 (0) | NR | NR |
| Xu 2020 | 46.67 ± 9.49 | 44.9 ± 8.08 | NR | NR | 65 | 64 | 14 | 16 | NR | NR |
| Yuan 2019 | 43.58 ± 8.86 | 44.56 ± 7.60 | 44.56 ± 7.60 | 24.56 ± 1.50 | 82 (82.8%) | 82 (82.8%) | 14 (14.1%) | 13 (13.1%) | 11 (11.1% | 10 (10.1%) |
| Zhang 2017 | 45 (29–64) | 46.6 (27–75) | 22.68 ± 3.15 | 24.07 ± 3.3 | 32 (91.4) | 40 (95.2) | 3 (5.6) | 2 (4.8) | NR | NR |
| Zhao 2021 | 47.02 ± 8.70 | 49.53 ± 9.32 | NR | NR | NR | NR | NR | NR | NR | NR |
NR not reported, n number, SD standard deviation.
Results of risk of bias assessment
The result of the quality assessment yielded an overall moderate risk of bias according to Cochrane`s tool and the mean score for observational studies was 10.57 out of 14 according to NHLB. All clinical trials44,55,56,83 reported proper randomization therefore they were categorized as low risk of bias. All clinical trials were at low risk of bias regarding attrition bias and selective reporting. A detailed illustration of the quality assessment of the included studies is illustrated in Supplementary Table S2.
Analysis of outcomes
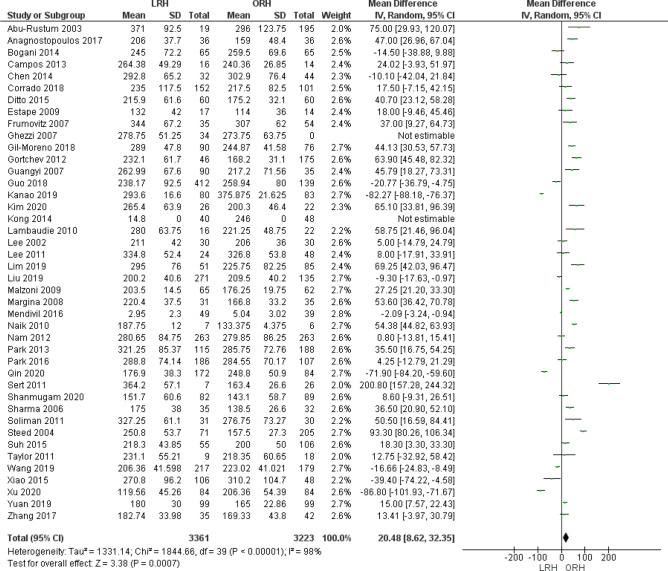
Operative time (minutes)
Operating time was reported by 42 studies. We found that ORH operating time was significantly lower than LRH operative time (MD = 20.48 [8.62, 32.35], (P = 0.007). Pooled data were heterogeneous (P < 0.001); I2 = 98% which could not be solved by the leave-one-out method or subgroup analysis (Fig. 2).
Figure 2.
Forest plot of operative time.
Estimated blood loss (ml)
We analyzed 6410 patients from 39 studies that reported the estimated blood loss. The overall mean difference showed that blood loss was significantly lower in LRH group than ORH group (MD = − 325.55 [− 386.16, − 264.94] (P < 0.001)), Pooled analysis was heterogeneous (P < 0.001); I2 = 97% (Fig. 3).
Figure 3.
Forest plot of estimated blood loss (EBL).
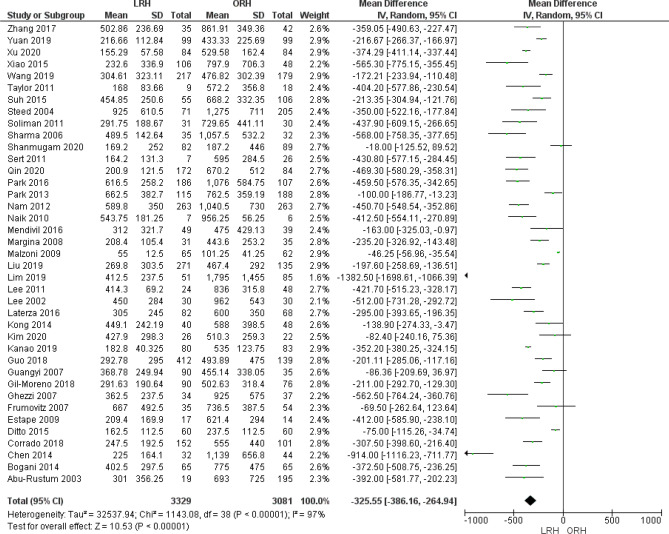
Intraoperative complication
Thirty two studies reported the rate of intraoperative complications. We found no significant difference between both groups (OR = 1.38 [0.94, 2.04], (P = 0.10)). Data was heterogeneous (P < 0.001); I2 = 69% as shown in Fig. 4A. We solved the heterogeneity by excluding Liang et al.87 (P = 0.15); I2 = 21%, the overall odds ratio after solving heterogeneity did not show any significant difference between both groups (OR = 1.14 [0.86, 1.51], (P = 0.37)) (Fig. 4B).
Figure 4.
Forest plot of the rate of intraoperative complications before (A) and after (B) solving for heterogeneity by excluding the Liang et al. study.
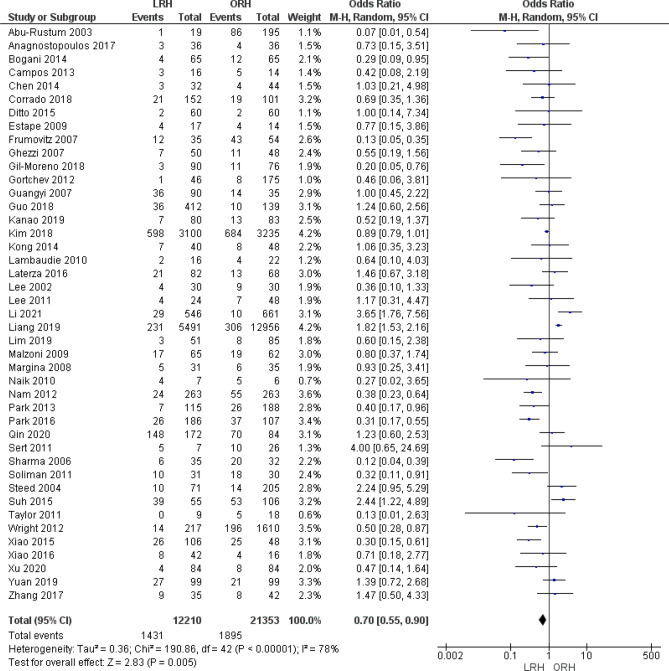
Postoperative complication
A total of 33,563 patients were analyzed from 43 studies that reported postoperative complications. The overall odds ratio showed that the LRH group had a postoperative complications rate significantly lower than that of ORH (OR = 0.70 [0.55, 0.90], (P = 0.005)). Pooled data was heterogeneous (P < 0.001); I2 = 78%. We could not solve heterogeneity by the leave-one-out method or subgroup analysis (Fig. 5).
Figure 5.
Forest plot of the rate of postoperative complications.
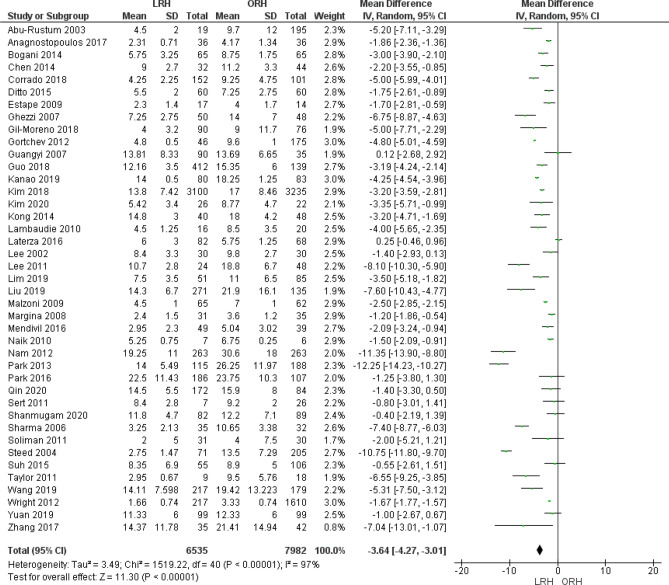
Length of hospital stay (days)
Forty-one studies reported length of hospital stay. We found that patients in the LRH group stayed at hospital fewer days than patients in the ORH group (MD = − 3.64 [− 4.27, − 3.01], (P < 0.001)). We found heterogeneity which could not be solved by the leave-one-out method or subgroup analysis (Fig. 6).
Figure 6.
Forest plot of the average length of hospital stay.
Resected lymph nodes
Thirty six studies reported the number of resected lymph nodes as an outcome. Pooled analysis showed that the LRH group was associated with fewer resected lymph nodes than the ORH group (MD = − 2.80 [− 4.35, − 1.24], (P = 0.004)). We found heterogeneity among studies (P < 0.001); I2 = 93% (Fig. 7).
Figure 7.
Forest plot of the number of resected lymph nodes.
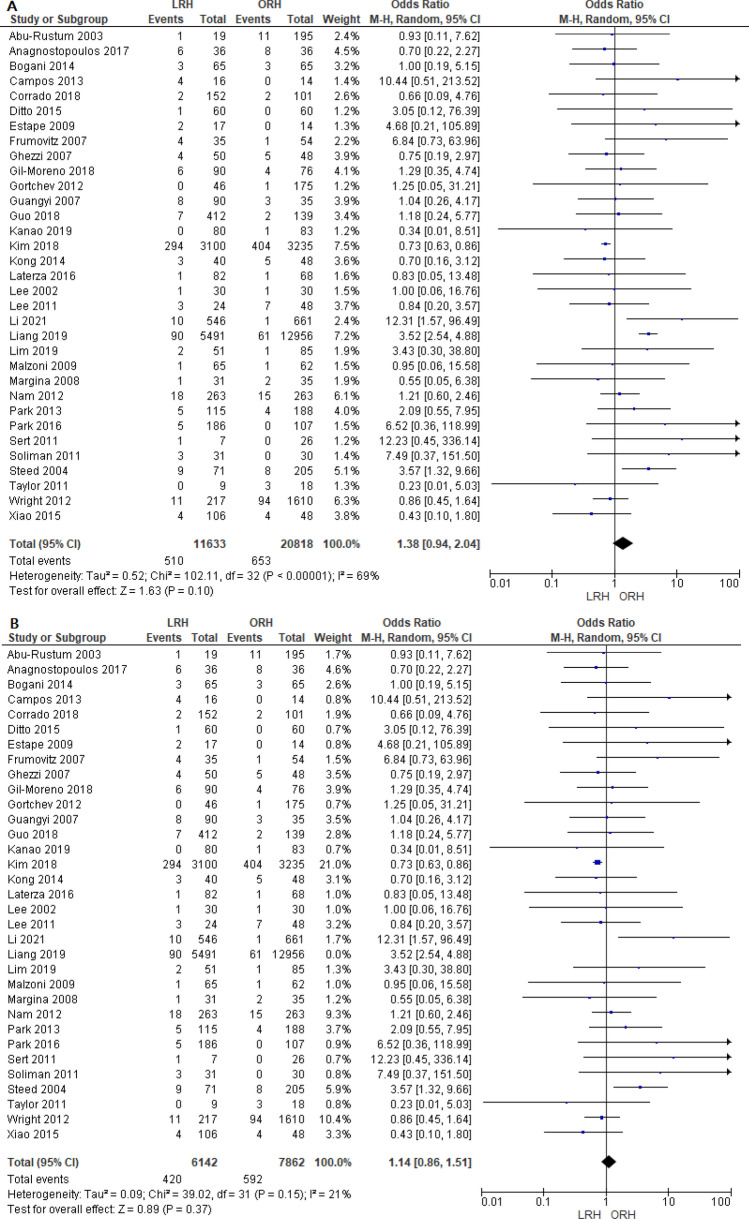
Five-year Overall Survival
A total of 8610 patients were analyzed from 22 studies. The combined analysis did not show any significant difference between both groups (OR = 1.24 [0.94, 1.64], (P = 0.12)). A little heterogeneity was found among studies (P = 0.03); I2 = 40% (Fig. 8A). We solved the heterogeneity by excluding Corrado et al.59 (P = 0.21); I2 = 19%. The overall analysis after solving heterogeneity also showed no significant difference between both groups (OR = 1.10 [0.87, 1.40], (P = 0.43)) (Fig. 8B).
Figure 8.
Forest plot of five-year overall survival before (A) and after (B) solving for heterogeneity by excluding the Corrado et al. study.
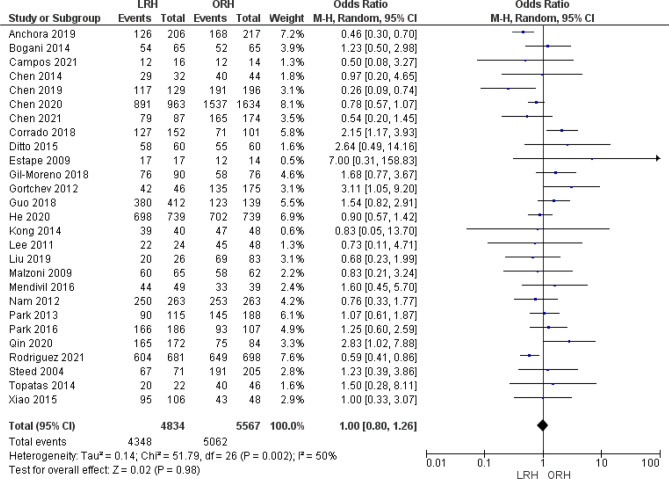
Disease free survival
Twenty seven studies reported DFS. Pooled analysis did not show any difference between both groups (OR = 1.00 [0.80, 1.26], (P = 0.98)). Data was heterogeneous (P = 0.002); I2 = 50% (Fig. 9).
Figure 9.
Forest plot of the rate of disease free survival.
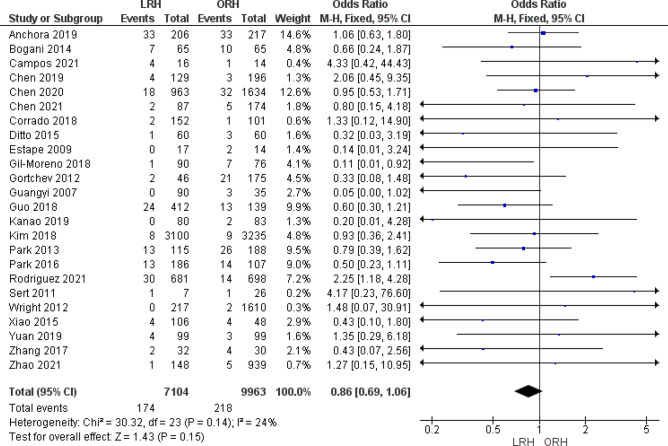
Postoperative or Intraoperative Mortality (Defined as within 90 days postop)
Twenty four studies reported mortality as an outcome. The overall odds ratio showed no significant difference between either group (OR = 0.86 [0.69, 1.06], (P = 0.15). Pooled analysis was homogeneous (P = 0.14); I2 = 24% (Fig. 10).
Figure 10.
Forest plot of the postoperative or intraoperative mortality rate.
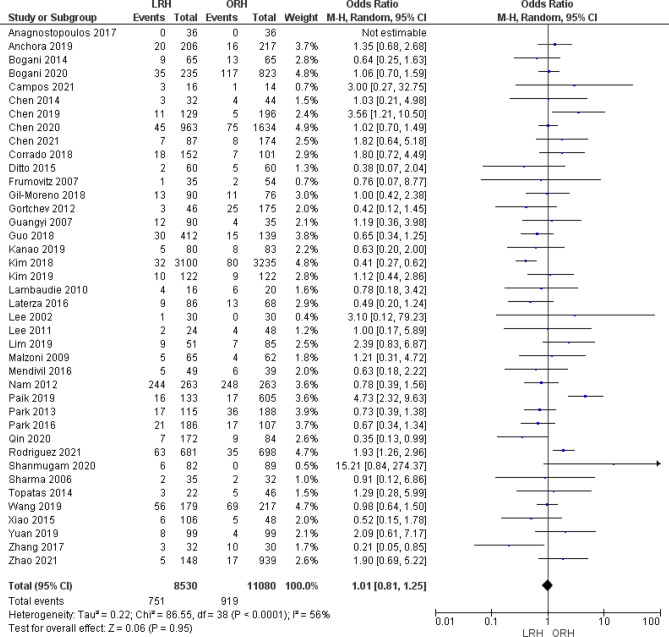
Recurrence
A total of 19,610 patients were analyzed from 40 studies. We found no significant difference between the two groups (OR = 1.01 [0.81, 1.25], (P = 0.95). Data was heterogeneous (P < 0.001); I2 = 56% (Fig. 11).
Figure 11.
Forest plot of recurrence of disease.
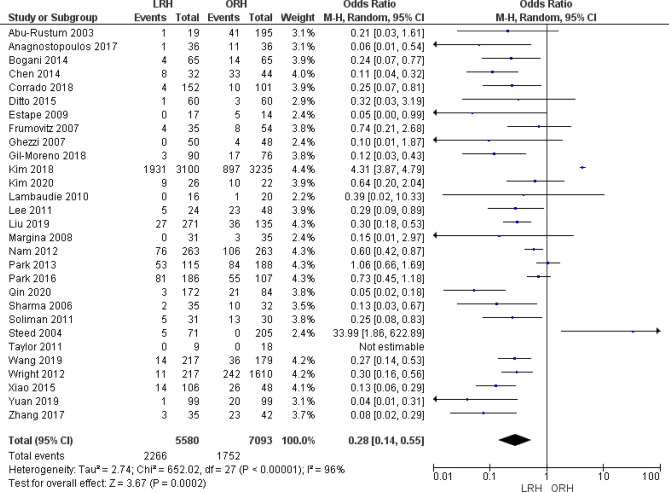
Blood transfusion rate
The combined analysis of 12,673 patients from 29 studies favored the LRH group significantly (OR = 0.28 [0.14, 0.55], (P = 0.002). Pooled analysis was heterogeneous (P < 0.001); I2 = 96% (Fig. 12).
Figure 12.
Forest plot of the rate of blood transfusion.
A funnel plot and Egger test of all outcomes can be found in Supplementary File S1. A separate sensitivity analysis involving only the studies with a low risk of bias can also be found in Supplementary File S2. The sensitivity analysis showed different findings only in the outcome of postoperative complications, where the result changed from statistically significant to insignificant. There were no changes in any other outcomes within the sensitivity analysis.
Discussion
This is the largest scale meta-analysis to date that has compared LRH to ORH through an evaluation of the available evidence, and the first, to our knowledge, to attempt to do so while specifically excluding robotic assisted techniques. In our study, we found that LRH was associated with a significantly lower incidence of estimated blood loss, postoperative complications. In addition, predictably, the LRH group had a short period of postoperative hospital stay. The number of the resected in the LRH group lymph node was significantly fewer than that of the ORH group. The combined analysis did not show any significant difference between both groups regarding 5-year overall survival, disease-free survival, and postoperative or intraoperative mortality. The duration of the surgical procedure was significantly longer in the LRH compared to ORH. This stands in contrast to previous studies that showed decreased survival as a result of minimally invasive radical hysterectomy techniques20.
Although isolated studies have disagreed with these results, the majority of previous systematic reviews and meta-analyses have not. In 2015, Wang et al.88 performed a meta-analysis of 12 cohort studies. They demonstrated similar results to our study. They conclude that LRH was better than ORH regarding the short-term outcomes such as faster functional recovery, estimated blood loss, and postoperative complications. The survival outcomes were also similar in both groups.
Smith et al.89 performed another meta-analysis to compare the minimally invasive hysterectomy with abdominal radical hysterectomy. They found that in more than 22,000 women with early-stage cervical cancer the progression-free survival was significantly worse for women who underwent the minimally invasive radical hysterectomy. This finding is strengthened with longer follow-up. The pooled relative risk for postoperative or intraoperative mortality was lower in the minimally invasive group.
In 2020, Kampers et al.90 performed the first meta-analysis stratifying the patients subjected to different operation techniques according to their risk factors. They compared the survival rates of open hysterectomy and laparoscopic hysterectomy in different risk groups. The study demonstrated that protective techniques in laparoscopy result in improved survival.
Kong et al.84 conducted a retrospective analysis of 88 patients with a cervical cancer diameter of 3 cm or greater. They found that LRH can be a feasible alternative surgical procedure for the management of FIGO stage IB and IIA cervical cancer. However, the institution at which the study was performed was introduced with the laparoscopic approach much later than the laparotomy approach. This in turn made the follow-up period in the LRH group relatively short to make any conclusive remarks on survival benefits.
Liang et al.87 reviewed the records of 18,447 patients undergoing radical hysterectomy for cervical cancer. They demonstrated that laparoscopic hysterectomy was associated with a higher risk of major complications than conventional laparotomy. Prior to our review, this study probably represented the largest scale evidence that assessed surgical complications after radical hysterectomy. Other studies to attempt this were single-center studies with small sample sizes15,60,74. In reconciling why the findings of Liang et al. did not also appear as statistically significant in our analysis, we hypothesize that this had to do with limitations on Liang’s study design. This study relied on inpatient medical records or readmission records to obtain information on complications without regular follow-up of the patients. Therefore, without any first-hand knowledge of the circumstances of this study we would hypothesize that perhaps this their conclusion may not have been as statistically significant if direct outreach to patients had been attempted, consistent with other cohort analyses.
In 2021, Campos et al.55 performed a single-center randomized controlled trial on 30 patients with cervical cancer and lymphovascular invasion. They demonstrated a non-significant trend of worse outcomes for LRH. The overall survival time and disease-free survival time were longer in the LRH group. However, the main limitation facing the study was the small sample size.
In 2018, the LACC study by Ramirez et al.20 found that the minimally invasive radical hysterectomy had lower rates of overall survival and disease-free survival than abdominal radical hysterectomy. It was largely based on this study that the National Comprehensive Cancer Network (NCCN) recommended careful counseling of the patient about short-term versus long-term outcomes and oncologic risks of the different surgical approaches.
Limitations
Although the main limitation facing us in this study is the heterogeneity in some outcomes, we managed to understand most of the attributing factors. We believe the use of studies with different designs and disparity in follow-up periods was responsible for the heterogeneity, which is understandable. Another possible limitation of our study includes selection bias, which is difficult to account for. With observational studies, there is always the possibility that surgeons have intentionally selected out cases for laparoscopic radical approaches that appear easier or have different characteristics than those chosen to be performed open. This could affect data. Our analysis represents the most recent and wide-scale evidence that compares LRH to ORH among women with cervical cancer. In light of this controversy it would be desirable to have more well designed prospective randomized trials in order to strengthen the evidence and dissolve any remaining controversy.
Conclusion
We conclude that LRH is associated with a significantly lower incidence of estimated blood loss, postoperative complications. In addition, the LRH had a short period of postoperative hospital stay. In contrast to previous studies that mixed robotic assisted cases we found no difference regarding 5-year overall survival and recurrence excluding robotic assisted cases.
Supplementary Information
Acknowledgements
The Marchand Institute for Minimally Invasive Surgery would like to acknowledge the efforts of all of the students, researchers, residents and fellows at the institute who put their time and effort into these projects without compensation, only for the betterment of women’s health. We firmly assure them that the future of medicine belongs to them.
Author contributions
All authors attest to significant contributions to this work. In particular the following duties were performed by the listed authors. This list does not preclude these authors from making other significant contributions to other portions of this work, and this Institute values all of the effort from our valuable team. (Middle initial corresponds to the second letter of the first name to avoid ambiguity.) Conceptualization was performed mostly by G.M., A.H.M., and A.H.A. Initial draft was composed mostly by A.K., H.U., A.M.A., C.C., S.G., C.M. and A.T.M. Data collection was performed mostly by C.C., S.G., and C.M. Data analysis was performed mostly by J.P., A.M.A., C.C., C.M., and A.T.M. Final draft and discussion was written mostly by G.M., A.H.M., and S.G. Data used was exempt from consent to participate or publish secondary to the nature of the study being a systematic review, retrospectively looking at previously published data.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-27430-9.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J. Clin. 2019;63:11–30. [Google Scholar]
- 2.Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J. Long-term outcome of laparoscopic surgery for colorectal cancer: A cochrane systematic review of randomised controlled trials. Cancer Treat. Rev. 2008 doi: 10.1002/14651858.CD003432.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int. J. Gynaecol. Obstet. 2009;105(2):103–104. doi: 10.1016/j.ijgo.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Ginaldi S, Wallace S, Jing BS, Bernardino ME. Carcinoma of the cervix: Lymphangiography and computer tomography. Am. J. Roentgenol. 1981 doi: 10.2214/ajr.136.6.1087. [DOI] [PubMed] [Google Scholar]
- 5.Togashi K, Nishimura K, Sagoh T, Minami S, Noma S, Fujisawa I, et al. Carcinoma of the cervix: Staging with MR imaging. Radiology. 1989 doi: 10.1148/radiology.171.1.2928532. [DOI] [PubMed] [Google Scholar]
- 6.Jones WB, Mercer GO, Lewis JL, Rubin SC, Hoskins WJ. Early invasive carcinoma of the cervix. Gynecol. Oncol. 1993 doi: 10.1006/gyno.1993.1241. [DOI] [PubMed] [Google Scholar]
- 7.Cibula D, Pötter R, Planchamp F, Avall-Lundqvist E, Fischerova D, Haie Meder C, et al. The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology Guidelines for the management of patients with cervical cancer. Int. J. Gynecol. Cancer. 2018 doi: 10.1016/j.radonc.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the cervix uteri. Int. J. Gynecol. Obstet. 2018 doi: 10.1002/ijgo.12611. [DOI] [PubMed] [Google Scholar]
- 9.Husain A, Chi DS, Prasad M, Abu-Rustum N, Barakat RR, Brown CL, et al. The role of laparoscopy in second-look evaluations for ovarian cancer. Gynecol. Oncol. 2001 doi: 10.1006/gyno.2000.6036. [DOI] [PubMed] [Google Scholar]
- 10.Nezhat CR, Burrell MO, Nezhat FR, Benigno BB, Welander CE. Laparoscopic radical hysterectomy with paraaortic and pelvic node dissection. Am. J. Obstet. Gynecol. 1992 doi: 10.1016/0002-9378(92)91351-A. [DOI] [PubMed] [Google Scholar]
- 11.Abu-Rustum NR, Gemignani ML, Moore K, Sonoda Y, Venkatraman E, Brown C, et al. Total laparoscopic radical hysterectomy with pelvic lymphadenectomy using the argon-beam coagulator: Pilot data and comparison to laparotomy. Gynecol. Oncol. 2003;91(2):402–409. doi: 10.1016/s0090-8258(03)00518-3. [DOI] [PubMed] [Google Scholar]
- 12.Diver E, Hinchcliff E, Gockley A, Melamed A, Contrino L, Feldman S, et al. Minimally invasive radical hysterectomy for cervical cancer is associated with reduced morbidity and similar survival outcomes compared with laparotomy. J. Minim. Invasive Gynecol. 2017 doi: 10.1016/j.ygyno.2016.04.485. [DOI] [PubMed] [Google Scholar]
- 13.Colombo N, Preti E, Landoni F, Carinelli S, Colombo A, Marini C, et al. Endometrial cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2013 doi: 10.1093/annonc/mdt353. [DOI] [PubMed] [Google Scholar]
- 14.Ayhan A, Tuncer ZS, Yarali H. Complications of radical hysterectomy in women with early stage cervical cancer: Clinical analysis of 270 cases. Eur. J. Surg/ Oncol. 1991;17:492–494. [PubMed] [Google Scholar]
- 15.Nam JH, Park JY, Kim DY, Kim JH, Kim YM, Kim YT. Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: Long-term survival outcomes in a matched cohort study. Ann. Oncol. 2012 doi: 10.1093/annonc/mdr360. [DOI] [PubMed] [Google Scholar]
- 16.Toptas T, Simsek T. Total laparoscopic versus open radical hysterectomy in stage IA2-IB1 cervical cancer: Disease recurrence and survival comparison. J. Laparoendosc. Adv. Surg. Tech. 2014;24(6):373–378. doi: 10.1089/lap.2013.0514. [DOI] [PubMed] [Google Scholar]
- 17.Wang W, Shang C, Huang J, Chen S, Shen H, Yao S. Long-term oncological outcomes after laparoscopic versus abdominal radical hysterectomy in stage I a2- II a2 cervical cancer: A matched cohort study. Zhonghua Fu Chan Ke Za Zhi. 2015 doi: 10.1097/IGC.0000000000000749. [DOI] [PubMed] [Google Scholar]
- 18.Zhu T, Chen X, Zhu J, Chen Y, Yu A, Chen L, et al. Surgical and pathological outcomes of laparoscopic versus abdominal radical hysterectomy with pelvic lymphadenectomy and/or para-aortic lymph node sampling for bulky early-stage cervical cancer. Int. J. Gynecol. Cancer. 2017 doi: 10.1097/IGC.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 19.Li X, Li J, Wen H, Ju X, Chen X, Xia L, et al. The survival rate and surgical morbidity of abdominal radical trachelectomy versus abdominal radical hysterectomy for stage IB1 cervical cancer. Ann. Surg. Oncol. 2016 doi: 10.1245/s10434-016-5216-1. [DOI] [PubMed] [Google Scholar]
- 20.Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N. Engl. J. Med. 2018;379(20):1895–1904. doi: 10.1056/NEJMoa1806395. [DOI] [PubMed] [Google Scholar]
- 21.Melamed A, Margul DJ, Chen L, Keating NL, del Carmen MG, Yang J, et al. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N. Engl. J. Med. 2018 doi: 10.1056/NEJMoa1804923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koh W-J, Abu-Rustum NR, Bean S, Bradley K, Campos SM, Cho KR, et al. Cervical cancer, Version 3.2019, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2019 doi: 10.6004/jnccn.2019.0001. [DOI] [PubMed] [Google Scholar]
- 23.Querleu D, Cibula D, Concin N, Fagotti A, Ferrero A, Fotopoulou C, et al. Laparoscopic radical hysterectomy: A European Society of Gynaecological Oncology (ESGO) statement. Int. J. Gynecol. Cancer. 2020 doi: 10.1136/ijgc-2019-000775. [DOI] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG, Antes G, Atkins D, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Rev. Esp. Nutr. Humana y Diet. 2014 doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. Wiley; 2008. p. 1. [Google Scholar]
- 26.Katz, A. Microsoft Excel 2010. Style (DeKalb, IL) (2010).
- 27.Lebowitz F. Endnote. Aperture; 2021. [Google Scholar]
- 28.Pearson GD, Mensah GA, Rosenberg Y, Stoney CM, Kavounis K, Goff DC. National Heart, Lung, and Blood Institute cardiovascular clinical trial perspective. Am. Heart J. 2020;224:25–34. doi: 10.1016/j.ahj.2020.02.014. [DOI] [PubMed] [Google Scholar]
- 29.Munder T, Barth J. Cochrane’s risk of bias tool in the context of psychotherapy outcome research. Psychother. Res. 2018 doi: 10.1080/10503307.2017.1411628. [DOI] [PubMed] [Google Scholar]
- 30.Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Handbook for Systematic Reviews of Interventions (2019).
- 31.Lee CL, Huang KG, Jain S, Lee PS, Soong YK. Comparison of laparoscopic and conventional surgery in the treatment of early cervical cancer. J. Am. Assoc. Gynecol. Laparosc. 2002;9(4):481–487. doi: 10.1016/s1074-3804(05)60523-3. [DOI] [PubMed] [Google Scholar]
- 32.Li Z, Chen C, Liu P, Duan H, Liu M, Xu Y, et al. Comparison of oncological outcomes and major complications between laparoscopic radical hysterectomy and abdominal radical hysterectomy for stage IB1 cervical cancer with a tumour size less than 2 cm. Eur. J. Surg. Oncol. 2021;47(8):2125–2133. doi: 10.1016/j.ejso.2021.03.238. [DOI] [PubMed] [Google Scholar]
- 33.Lee EJ, Kang H, Kim DH. A comparative study of laparoscopic radical hysterectomy with radical abdominal hysterectomy for early-stage cervical cancer: A long-term follow-up study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011;156(1):83–86. doi: 10.1016/j.ejogrb.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 34.Lim TYK, Lin KKM, Wong WL, Aggarwal IM, Yam PKL. Surgical and oncological outcome of total laparoscopic radical hysterectomy versus radical abdominal hysterectomy in early cervical cancer in Singapore. Gynecol. Minim. Invasive Ther. 2019;8(2):53–58. doi: 10.4103/GMIT.GMIT_43_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steed H, Rosen B, Murphy J, Laframboise S, De Petrillo D, Covens A. A comparison of laparascopic-assisted radical vaginal hysterectomy and radical abdominal hysterectomy in the treatment of cervical cancer. Gynecol. Oncol. 2004;93(3):588–593. doi: 10.1016/j.ygyno.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 36.Shanmugam S, Susikar S, Hussain SA, Bharanidharan T, Michael R. A retrospective comparison of the outcomes of laparoscopic and open radical hysterectomy for early and advanced cancer of the cervix, in the post-LACC era. Indian J. Gynecol. Oncol. 2020 doi: 10.1007/s40944-020-00473-w. [DOI] [Google Scholar]
- 37.Rodriguez J, Rauh-Hain JA, Saenz J, Isla DO, Rendon Pereira GJ, Odetto D, et al. Oncological outcomes of laparoscopic radical hysterectomy versus radical abdominal hysterectomy in patients with early-stage cervical cancer: A multicenter analysis. Int. J. Gynecol. Cancer. 2021;31(4):504–511. doi: 10.1136/ijgc-2020-002086. [DOI] [PubMed] [Google Scholar]
- 38.Sert MB, Abeler V. Robot-assisted laparoscopic radical hysterectomy: Comparison with total laparoscopic hysterectomy and abdominal radical hysterectomy; One surgeon’s experience at the Norwegian Radium Hospital. Gynecol. Oncol. 2011;121(3):600–604. doi: 10.1016/j.ygyno.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Park JY, Kim D, Suh DS, Kim JH, Kim YM, Kim YT, et al. The role of laparoscopic radical hysterectomy in early-stage adenocarcinoma of the uterine cervix. Ann. Surg. Oncol. 2016;23:825–833. doi: 10.1245/s10434-016-5489-4. [DOI] [PubMed] [Google Scholar]
- 40.Qin M, Siyi L, Huang HF, Li Y, Gu Y, Wang W, et al. A comparison of laparoscopies and laparotomies for radical hysterectomy in stage IA1–IB1 cervical cancer patients: A single team with 18 years of experience. Front. Oncol. 2020;10:1–12. doi: 10.3389/fonc.2020.01738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Laparoscopic versus open radical hysterectomy in patients with stage IB2 and IIA2 cervical cancer. J. Surg. Oncol. 2013;108(1):63–69. doi: 10.1002/jso.23347. [DOI] [PubMed] [Google Scholar]
- 42.Soliman PT, Frumovitz M, Sun CC, Dos Reis R, Schmeler KM, Nick AM, et al. Radical hysterectomy: A comparison of surgical approaches after adoption of robotic surgery in gynecologic oncology. Gynecol. Oncol. 2011;123(2):333–336. doi: 10.1016/j.ygyno.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xiao M, Gao H, Bai H, Zhang Z. Quality of life and sexuality in disease-free survivors of cervical cancer after radical hysterectomy alone: A comparison between total laparoscopy and laparotomy. Medicine (United States) 2016;95(36):4787. doi: 10.1097/MD.0000000000004787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu Q, Dong M, Dong W, Yang D, Zhang J, Liu J, et al. Postoperative comparison of laparoscopic radical resection and open abdominal radical hysterectomy for cervical cancer patient. Arch. Gynecol. Obstet. 2020;302(2):473–479. doi: 10.1007/s00404-020-05606-2. [DOI] [PubMed] [Google Scholar]
- 45.Xiao M, Zhang Z. Total laparoscopic versus laparotomic radical hysterectomy and lymphadenectomy in cervical cancer an observational study of 13-year experience. Medicine (United States) 2015;94(30):1–6. doi: 10.1097/MD.0000000000001264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang W, Li L, Wu M, Ma S, Tan X, Zhong S. Laparoscopic vs. abdominal radical hysterectomy for locally advanced cervical cancer. Front. Oncol. 2019;9:1–10. doi: 10.3389/fonc.2019.01331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wright JD, Herzog TJ, Neugut AI, Burke WM, Lu YS, Lewin SN, et al. Comparative effectiveness of minimally invasive and abdominal radical hysterectomy for cervical cancer. Gynecol. Oncol. 2012;127(1):11–17. doi: 10.1016/j.ygyno.2012.06.031. [DOI] [PubMed] [Google Scholar]
- 48.Suh DH, Cho HY, Kim K, No JH, Kim YB. Matched-case comparisons in a single institution to determine critical points for inexperienced surgeons’ successful performances of laparoscopic radical hysterectomy versus abdominal radical hysterectomy in stage IA2-IIA cervical cancer. PLoS ONE. 2015;10(6):1–14. doi: 10.1371/journal.pone.0131170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taylor SE, McBee WC, Richard SD, Edwards RP. Radical hysterectomy for early stage cervical cancer: Laparoscopy versus laparotomy. J. Soc. Laparoendosc. Surg. 2011;15(2):213–217. doi: 10.4293/108680811X13022985132218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sharma R, Bailey J, Anderson R, Murdoch J. Laparoscopically assisted radical vaginal hysterectomy (Coelio-Schauta): A comparison with open Wertheim/Meigs hysterectomy. Int. J. Gynecol. Cancer. 2006;16(5):1927–1932. doi: 10.1111/j.1525-1438.2006.00661.x. [DOI] [PubMed] [Google Scholar]
- 51.Zhao W, Yang Q. Lymph-vascular space invasion in patients with stages ia2–iia2 cervical cancer treated with laparoscopic versus open radical hysterectomy. Cancer Manag. Res. 2021;13:1179–1186. doi: 10.2147/CMAR.S292477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang S, Ma L, Meng QW, Zhou D, Moyiding T. Comparison of laparoscopic-assisted radical vaginal hysterectomy and abdominal radical hysterectomy in patients with early stage cervical cancer. Medicine (United States) 2017;96(36):e8005. doi: 10.1097/MD.0000000000008005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yuan Z, Cao D, Yang J, Yu M, Shen K, Yang J, et al. Laparoscopic vs. Open abdominal radical hysterectomy for cervical cancer: A single-institution, propensity score matching study in China. Front. Oncol. 2019;9:1–7. doi: 10.3389/fonc.2019.01107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen CH, Chiu LH, Chang CW, Yen YK, Huang YH, Liu WM. Comparing robotic surgery with conventional laparoscopy and laparotomy for cervical cancer management. Int. J. Gynecol. Cancer. 2014;24(6):1105–1111. doi: 10.1097/IGC.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 55.Campos LS, Limberger LF, Stein AT, Caldas JM. Survival after laparoscopic versus abdominal radical hysterectomy in early cervical cancer: A randomized controlled trial. Asian Pac. J. Cancer Prev. 2021;22(1):93–97. doi: 10.31557/APJCP.2021.22.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Campos LS, Limberger LF, Stein AT, Kalil AN. Postoperative pain and perioperative outcomes after laparoscopic radical hysterectomy and abdominal radical hysterectomy in patients with early cervical cancer: A randomised controlled trial. Trials. 2013 doi: 10.1186/1745-6215-14-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pedone Anchora L, Turco LC, Bizzarri N, Capozzi VA, Lombisani A, Chiantera V, et al. How to select early-stage cervical cancer patients still suitable for laparoscopic radical hysterectomy: A propensity-matched study. Ann. Surg. Oncol. 2020;27(6):1947–1955. doi: 10.1245/s10434-019-08162-5. [DOI] [PubMed] [Google Scholar]
- 58.Bogani G, Ghezzi F, Chiva L, Gisone B, Pinelli C, Dell’acqua A, et al. Patterns of recurrence after laparoscopic versus open abdominal radical hysterectomy in patients with cervical cancer: A propensity-matched analysis. Int. J. Gynecol Cancer. 2020;30(7):987–992. doi: 10.1136/ijgc-2020-001381. [DOI] [PubMed] [Google Scholar]
- 59.Corrado G, Vizza E, Legge F, Pedone Anchora L, Sperduti I, Fagotti A, et al. Comparison of different surgical approaches for stage IB1 cervical cancer patients: A multi-institution study and a review of the literature. Int. J. Gynecol. Cancer. 2018;28(5):1020–1028. doi: 10.1097/IGC.0000000000001254. [DOI] [PubMed] [Google Scholar]
- 60.Bogani G, Cromi A, Uccella S, Serati M, Casarin J, Pinelli C, et al. Laparoscopic versus open abdominal management of cervical cancer: Long-term results from a propensity-matched analysis. J. Minim. Invasive Gynecol. 2014 doi: 10.1016/j.jmig.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 61.Anagnostopoulos A, Mitra S, Decruze B, Macdonald R, Kirwan J. Safety and cost considerations during the introduction period of laparoscopic radical hysterectomy. Obstet. Gynecol. Int. 2017 doi: 10.1155/2017/2103763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gil-Moreno A, Carbonell-Socias M, Salicrú S, Centeno-Mediavilla C, Franco-Camps S, Colas E, et al. Radical hysterectomy: Efficacy and safety in the dawn of minimally invasive techniques. J. Minim. Invasive Gynecol. 2019;26(3):492–500. doi: 10.1016/j.jmig.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 63.Gortchev G, Tomov S, Tantchev L, Velkova A, Radionova Z. Robot-assisted radical hysterectomy-perioperative and survival outcomes in patients with cervical cancer compared to laparoscopic and open radical surgery. Gynecol. Surg. 2012;9(1):81–88. [Google Scholar]
- 64.Li G, Yan X, Shang H, Wang G, Chen L, Han Y. A comparison of laparoscopic radical hysterectomy and pelvic lymphadenectomy and laparotomy in the treatment of Ib–IIa cervical cancer. Gynecol. Oncol. 2007;105(1):176–180. doi: 10.1016/j.ygyno.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 65.Guo J, Yang L, Cai J, Xu L, Min J, Shen Y, et al. Laparoscopic procedure compared with open radical hysterectomy with pelvic lymphadenectomy in early cervical cancer: A retrospective study. Onco Targets Ther. 2018;11:5903–5908. doi: 10.2147/OTT.S156064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.He J, Hao M, Liu P, Liu Z, Lang J, Bin X, et al. Comparison of laparoscopic and abdominal radical hysterectomy for early stage cervical cancer: Oncologic outcomes based on tumor diameter. Int. J. Gynecol. Cancer. 2020;30(9):1308–1316. doi: 10.1136/ijgc-2020-001504. [DOI] [PubMed] [Google Scholar]
- 67.Kanao H, Matsuo K, Aoki Y, Tanigawa T, Nomura H, Okamoto S, et al. Feasibility and outcome of total laparoscopic radical hysterectomy with no-look no-touch technique for FIGO IB1 cervical cancer. J. Gynecol. Oncol. 2019;30(3):1–12. doi: 10.3802/jgo.2019.30.e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen X, Zhao N, Ye P, Chen J, Nan X, Zhao H, et al. Comparison of laparoscopic and open radical hysterectomy in cervical cancer patients with tumor size ≤2 cm. Int. J. Gynecol. Cancer. 2020;30(5):564–571. doi: 10.1136/ijgc-2019-000994. [DOI] [PubMed] [Google Scholar]
- 69.Kim SI, Lee M, Lee S, Suh DH, Kim HS, Kim K, et al. Impact of laparoscopic radical hysterectomy on survival outcome in patients with FIGO stage IB cervical cancer: A matching study of two institutional hospitals in Korea. Gynecol. Oncol. 2019;155(1):75–82. doi: 10.1016/j.ygyno.2019.07.019. [DOI] [PubMed] [Google Scholar]
- 70.Kim JH, Kim K, Park SJ, Lee JY, Kim K, Lim MC, et al. Comparative effectiveness of abdominal versus laparoscopic radical hysterectomy for cervical cancer in the postdissemination era. Cancer Res. Treat. 2019;51(2):788–796. doi: 10.4143/crt.2018.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen C, Liu P, Ni Y, Tang L, Xu Y, Bin X, et al. Laparoscopic versus abdominal radical hysterectomy for stage IB1 cervical cancer patients with tumor size ≤ 2 cm: A case-matched control study. Int. J. Clin. Oncol. 2020;25(5):937–947. doi: 10.1007/s10147-020-01630-z. [DOI] [PubMed] [Google Scholar]
- 72.Estape R, Lambrou N, Diaz R, Estape E, Dunkin N, Rivera A. A case matched analysis of robotic radical hysterectomy with lymphadenectomy compared with laparoscopy and laparotomy. Gynecol. Oncol. 2009;113(3):357–361. doi: 10.1016/j.ygyno.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 73.Chen X, Yu J, Zhao H, Hu Y, Zhu H. Laparoscopic radical hysterectomy results in higher recurrence rate versus open abdominal surgery for stage IB1 cervical cancer patients with tumor size less than 2 centimeter: A retrospective propensity score-matched study. Front. Oncol. 2021;11:1–9. doi: 10.3389/fonc.2021.683231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Magrina JF, Kho RM, Weaver AL, Montero RP, Magtibay PM. Robotic radical hysterectomy: Comparison with laparoscopy and laparotomy. Gynecol. Oncol. 2008 doi: 10.1016/j.ygyno.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 75.Liu Y, Li L, Wu M, Ma S, Tan X, Zhong S, et al. The impact of the surgical routes and learning curve of radical hysterectomy on the survival outcomes in stage IB cervical cancer: A retrospective cohort study. Int. J. Surg. 2019;68:72–77. doi: 10.1016/j.ijsu.2019.06.009. [DOI] [PubMed] [Google Scholar]
- 76.Ditto A, Martinelli F, Bogani G, Gasparri ML, Di Donato V, Zanaboni F, et al. Implementation of laparoscopic approach for type B radical hysterectomy: A comparison with open surgical operations. Eur. J. Surg. Oncol. 2015;41(1):34–39. doi: 10.1016/j.ejso.2014.10.058. [DOI] [PubMed] [Google Scholar]
- 77.Frumovitz M, Dos Reis R, Sun CC, Milam MR, Bevers MW, Brown J, et al. Comparison of total laparoscopic and abdominal radical hysterectomy for patients with early-stage cervical cancer. Obstet. Gynecol. 2007;110(1):96–102. doi: 10.1097/01.AOG.0000268798.75353.04. [DOI] [PubMed] [Google Scholar]
- 78.Ghezzi F, Cromi A, Ciravolo G, Volpi E, Uccella S, Rampinelli F, et al. Surgicopathologic outcome of laparoscopic versus open radical hysterectomy. Gynecol. Oncol. 2007;106(3):502–506. doi: 10.1016/j.ygyno.2007.04.027. [DOI] [PubMed] [Google Scholar]
- 79.Malzoni M, Tinelli R, Cosentino F, Fusco A, Malzoni C. Total laparoscopic radical hysterectomy versus abdominal radical hysterectomy with lymphadenectomy in patients with early cervical cancer: Our experience. Ann. Surg. Oncol. 2009;16(5):1316–1323. doi: 10.1245/s10434-009-0342-7. [DOI] [PubMed] [Google Scholar]
- 80.Paik ES, Lim MC, Kim MH, Kim YH, Song ES, Seong SJ, et al. Comparison of laparoscopic and abdominal radical hysterectomy in early stage cervical cancer patients without adjuvant treatment: Ancillary analysis of a Korean Gynecologic Oncology Group Study (KGOG 1028) Gynecol. Oncol. 2019;154(3):547–553. doi: 10.1016/j.ygyno.2019.06.023. [DOI] [PubMed] [Google Scholar]
- 81.Mendivil AA, Rettenmaier MA, Abaid LN, Brown JV, Micha JP, Lopez KL, et al. Survival rate comparisons amongst cervical cancer patients treated with an open, robotic-assisted or laparoscopic radical hysterectomy: A five year experience. Surg. Oncol. 2016;25(1):66–71. doi: 10.1016/j.suronc.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 82.Kim S, Min KJ, Lee S, Hong JH, Song JY, Lee JK, et al. Learning curve could affect oncologic outcome of minimally invasive radical hysterectomy for cervical cancer. Asian J. Surg. 2021;44(1):174–180. doi: 10.1016/j.asjsur.2020.05.006. [DOI] [PubMed] [Google Scholar]
- 83.Naik R, Jackson KS, Lopes A, Cross P, Henry JA. Laparoscopic assisted radical vaginal hysterectomy versus radical abdominal hysterectomy—A randomised phase II trial: Perioperative outcomes and surgicopathological measurements. BJOG Int. J. Obstet. Gynaecol. 2010;117(6):746–751. doi: 10.1111/j.1471-0528.2010.02479.x. [DOI] [PubMed] [Google Scholar]
- 84.Kong TW, Chang SJ, Lee J, Paek J, Ryu HS. Comparison of laparoscopic versus abdominal radical hysterectomy for FIGO stage IB and IIA cervical cancer with tumor diameter of 3 cm or greater. Int. J. Gynecol. Cancer. 2014;24(2):280–288. doi: 10.1097/IGC.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 85.Laterza RM, Uccella S, Casarin J, Morosi C, Serati M, Koelbl H, et al. Recurrence of early stage cervical cancer after laparoscopic versus open radical surgery. Int. J. Gynecol. Cancer. 2016;26(3):547–552. doi: 10.1097/IGC.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 86.Lambaudie E, Narducci F, Bannier M, Jauffret C, Pouget N, Leblanc E, et al. Role of robot-assisted laparoscopy in adjuvant surgery for locally advanced cervical cancer. Eur. J. Surg. Oncol. 2010;36(4):409–413. doi: 10.1016/j.ejso.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 87.Liang C, Liu P, Cui Z, Liang Z, Bin X, Lang J, et al. Effect of laparoscopic versus abdominal radical hysterectomy on major surgical complications in women with stage IA–IIB cervical cancer in China, 2004–2015. Gynecol. Oncol. 2020;156(1):115–123. doi: 10.1016/j.ygyno.2019.10.032. [DOI] [PubMed] [Google Scholar]
- 88.Wang Y, Deng L, Xu H, Zhang Y, Liang Z. Laparoscopy versus laparotomy for the management of early stage cervical cancer. BMC Cancer. 2015 doi: 10.1186/s12885-015-1818-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Smith AJB, Jones TN, Miao D, Fader AN. Minimally invasive radical hysterectomy for cervical cancer: A systematic review and meta-analysis. J. Minim. Invasive Gynecol. 2021;28(3):544–555.e7. doi: 10.1016/j.jmig.2020.12.023. [DOI] [PubMed] [Google Scholar]
- 90.Kampers J, Gerhardt E, Sibbertsen P, Flock T, Klapdor R, Hertel H, et al. Protective operative techniques in radical hysterectomy in early cervical carcinoma and their influence on disease-free and overall survival: A systematic review and meta-analysis of risk groups. Arch. Gynecol. Obstet. 2021;304(3):577–587. doi: 10.1007/s00404-021-06082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.