Abstract
Introduction
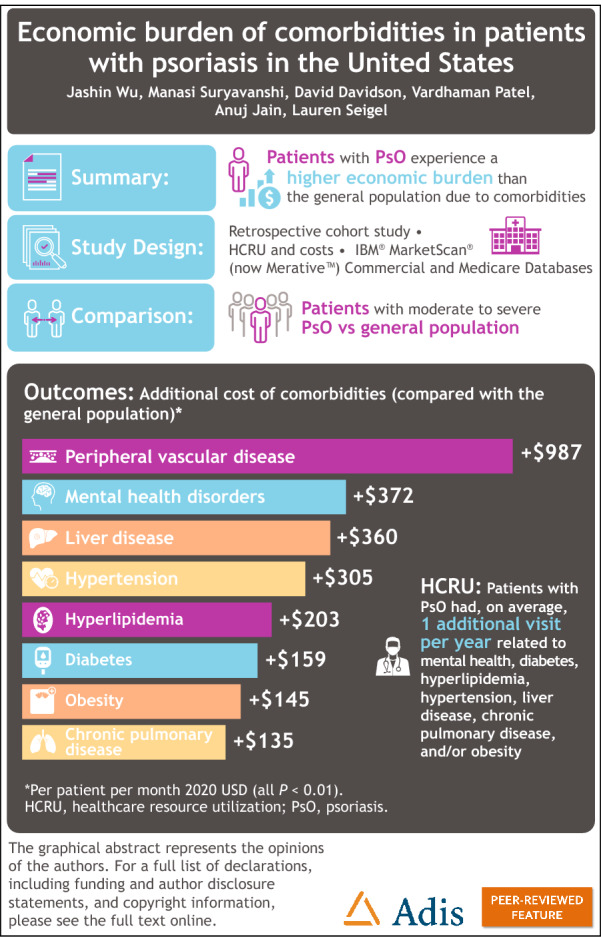
This study assessed the comorbidity burden, healthcare resource utilization (HCRU), and costs associated with patients with moderate to severe psoriasis (PsO) compared with a matched cohort of the general population without PsO in the USA.
Methods
Comorbidity-related HCRU (incidence rate ratios [IRRs]) and direct medical cost burden (per patient per month [PPPM] 2020 USD) in patients with moderate to severe PsO in the USA, previously apremilast- and biologic-naive, but currently treated, versus the general population were assessed through a retrospective cohort study using IBM (now Merative) MarketScan Commercial and Medicare Claims data (1 January 2006 to 31 December 2019). Comorbidities included cardiovascular, mental health, pulmonary, diabetes, hyperlipidemia, hypertension, peripheral vascular, liver, obesity, and other autoimmune disorders.
Results
There are increased all-cause HCRU and costs in patients with PsO compared with the general population. These differences (PsO–general population) in HCRU and costs (IRR visits; PPPM) are associated with specific comorbidities, including mental health (1.08; $372), chronic pulmonary disease (1.07; $135), diabetes (1.10; $159), hyperlipidemia (1.13; $203), hypertension (1.13; $305), liver disease (1.21; $360), and obesity (1.12; $145, all P < 0.01).
Conclusions
Patients with PsO experience a higher economic burden of comorbidities than the general population despite using currently available systemic treatments for PsO.
Keywords: Biologics, Claims data, Cohort, Cost, Healthcare resource utilization
Plain Language Summary
Psoriasis is a disease that causes itchy and painful sores on the skin. People with psoriasis can develop several other diseases, known as comorbidities. These comorbidities include cardiovascular disease, depression, diabetes, hypertension, and obesity, and they pose a large economic burden to individuals, households, and society. Existing estimates of this burden are outdated because new treatments have become available for psoriasis. The aim of this study was to assess the economic burden of comorbidities in people with psoriasis compared with the economic burden in the general population in the USA. Healthcare claims reported in the IBM (now Merative) MarketScan Commercial and Medicare Claims database were used. This study assessed the total number of health-related visits to a doctor’s office, hospital, or emergency department and the total costs of these visits in both groups. This study found that people with psoriasis had more health visits and costs because of comorbidities than the general population, despite using advanced treatments for their psoriasis.
Key Summary Points
| Psoriasis is a highly prevalent inflammatory disease associated with the following comorbidities: psoriatic arthritis, cardiovascular disease, depression, diabetes, hyperlipidemia, hypertension, obesity, cerebrovascular disease, and peripheral vascular disease. |
| In 2013, the economic burden of these comorbidities was estimated at $36.4 billion annually; since then, new systemic treatments and biologics have become widely available, potentially impacting this estimate. |
| The aim of this study was to assess comorbidity-related healthcare resource utilization (HCRU) and direct medical cost burden in biologic- and apremilast-naive patients with psoriasis versus a matched control cohort of the general population without psoriasis in the USA. |
| This study found increased all-cause HCRU and costs due to comorbidities in patients with psoriasis compared with the general population with the same comorbidities. |
| The increased economic burden ranged from 30% to 194% in total medical costs, despite the use of currently available systemic treatments for psoriasis. |
Graphical abstract
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article go to 10.6084/m9.figshare.21261999.
Introduction
Psoriasis (PsO) is a widely prevalent, chronic, systemic, immune-mediated inflammatory disease [1–3]. Symptoms include plaques, usually covered in scales, that cause itching, pain, and decreased quality of life [4]. Typically affecting the skin, PsO can also affect joints and is associated with several comorbid conditions affecting multiple organ systems, underscoring the systemic inflammatory burden of the disease [3]. Patients may feel stigmatized when their PsO is visible and may report depression [5]. Some of the most frequently reported comorbidities in patients with PsO are psoriatic arthritis, cardiovascular disease, depression, diabetes, hyperlipidemia, hypertension, obesity, cerebrovascular disease, peripheral vascular disease, and ophthalmologic conditions, such as uveitis, dry eye, cataracts, and visual fogging [6–8]. The burden of these comorbidities increases along with increasing PsO severity [9]. Treatment guidelines recommend that dermatologists discuss potential comorbidities with patients to facilitate patient-engaged, comprehensive care and to enhance quality of life [10].
Patients with PsO have considerable comorbidity, healthcare resource utilization (HCRU), and expenditures [5–7]. Previous database studies have estimated the general costs of PsO [7], compared the costs of patients with PsO with and without comorbidities [6], or estimated comorbidity burden of patients with PsO compared with the general population at a time when the introduction of biologics occurred [5]. Among all patients with PsO, those with comorbidities had significantly higher healthcare costs compared with patients without comorbidities [6]. Patients with PsO with selected comorbidities had significantly higher mean total healthcare expenditures compared with individuals without PsO with the same comorbidities [7]. An earlier systematic review estimated that the direct costs for PsO ranged from $51.7 billion to $63.2 billion, and comorbidities contributed $36.4 billion annually in 2013 [11]. As that estimate was from a 2011 study [6] adjusted to 2013 USD [11], an updated estimate of PsO comorbidity burden of apremilast- and biologic-naive patients treated with modern systemic treatments is warranted.
The literature on PsO comorbidity burden is dated [6, 7, 11], with the most recent database review examining individuals through March 2012 [5]. These prior studies assessed economic burden of PsO before biologics were widely available; therefore, a new study is called for to update estimates of comorbidity burden since the introduction of more treatment options using more recent claims data. The aim of this study was to assess comorbidity-related HCRU and direct medical cost burden in biologic- and apremilast-naive patients with moderate to severe PsO versus a matched control cohort of the general population without PsO in the USA.
Methods
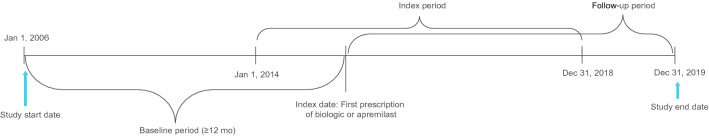
We assessed comorbidity-related HCRU and direct medical cost burden in patients who were biologic- and apremilast-naive in the USA who newly initiated treatment for moderate to severe PsO versus the general population through a retrospective database study using IBM MarketScan (now Merative) Commercial and Medicare Claims data from 1 January 2006 to 31 December 2019 (Fig. 1). The study population included adult patients (≥ 18 years) in the USA who were identified as having moderate to severe PsO [12], based on International Classification of Diseases (ICD) codes ICD-9-CM 696.1; ICD-10-CM L40.0-L40.4, L40.8-L40.9, who newly initiated treatment with apremilast, an interleukin inhibitor (ILi; ustekinumab, secukinumab, ixekizumab, brodalumab, guselkumab, tildrakizumab, or risankizumab), or a tumor necrosis factor inhibitor (TNFi; adalimumab, etanercept, infliximab, or certolizumab pegol) during the index period of 1 January 2014 to 31 December 2018. Patients also must have had continuous medical and pharmacy enrollment for ≥ 1 year before and after the index date (first apremilast, ILi, or TNFi prescription), and ≥ 2 PsO claims on or in the 12 months before the index date. Patients were excluded for a diagnosis of rheumatoid arthritis, ankylosing spondylitis, Crohn disease, ulcerative colitis, hidradenitis suppurativa, uveitis, Behçet disease, or juvenile idiopathic arthritis at any point during the study period. Patients with biologic or apremilast use at any time during the baseline period or any claim for psoriatic arthritis in the 12 months before index date were also excluded.
Fig. 1.
Study design overview
The PsO cohort was exact-matched 1:2 on age, sex, and region to general population controls aged ≥ 18 years on the index date who had ≥ 1 year of continuous enrollment in the baseline and follow-up periods. Control patients with PsO and psoriatic arthritis during the baseline period or follow-up were excluded. Patients were followed from their index date until the insurance enrollment end date, index drug discontinuation date, switch date, or study end date, whichever came first. Follow-up for each patient with PsO and their matched controls was stopped at the date when follow-up ended for either the patient with PsO or matched control. Comorbidities for which HCRU and costs were compared between PsO and general population cohorts included cardiovascular (i.e., myocardial infarction, coronary heart disease, or stroke), mental health (i.e., anxiety, depression, or suicidal ideation), chronic pulmonary disease, diabetes, hyperlipidemia, hypertension, peripheral vascular disease, liver disease, obesity, and other autoimmune disorders (i.e., alopecia areata, celiac disease, systemic sclerosis, Sjögren syndrome, vitiligo, chronic urticaria, systemic lupus erythematosus, Addison disease, giant cell arteritis, chronic glomerulonephritis, or pulmonary fibrosis).
Baseline patient demographic and clinical characteristics are summarized using descriptive statistics and compared between patients with PsO and matched controls using Wilcoxon signed-rank tests for continuous variables and McNemar tests for categorical variables. All-cause comorbidity-related HCRU, including outpatient visits, inpatient visits, emergency department (ED) visits, and total medical visits (sum of inpatient, outpatient, and ED visits), was compared between matched PsO patients and the general population controls using multivariate regression models. Adjusted incidence rate ratios (IRRs; adjusted for comorbidities, insurance type, and baseline HCRU/costs) were generated for HCRU. A two-part generalized estimating equation regression model with appropriate distribution (negative binomial and zero-inflated Poisson) and log link was used to estimate IRRs and 95% confidence intervals.
Total medical costs (sum of inpatient, outpatient, and ED-adjusted costs) were estimated and inflated to 2020 using the medical care component of the consumer price index (CPI). For adjusted cost models, gamma regression and log link were used after adding $1 to zero costs. HCRU and cost models were adjusted for age, sex, region, insurance plan type, Charlson comorbidity index (CCI), cohort (PsO/control), comorbidity, interaction of comorbidity and cohort, and baseline HCRU and cost for respective models. Differences in medication use, inpatient length of stay, and prescription fills and their associated costs were examined between groups. A sensitivity analysis was performed excluding HCRU/costs associated with PsO treatment from pharmacy costs to attempt to minimize their influence on costs.
Compliance with Ethics Guidelines
This study used data from the MarketScan database. Access to the database was granted by MarketScan under license. No patients were directly involved in the study, and only deidentified patient information was used; thus, institutional review board approval was waived.
Results
A total of 28,347 patients were included (Table 1). Patients in the PsO cohort did not differ from the matched controls in terms of age, sex, or region. However, there were differences (P < 0.001) in insurance plan type, with patients with PsO more often in preferred provider organization (PPO) plans (58.1% PsO cohort versus 51.1% matched controls). The most prevalent comorbidities in the PsO and matched cohorts were hypertension (33.2% and 25.9%, respectively), hyperlipidemia (30.5% and 23.4%), mental disorders (16.6% and 11.5%), and diabetes (14.2% and 9.9%). All comorbidities under study were more prevalent in patients with PsO versus matched controls (P < 0.01).
Table 1.
Baseline characteristicsa
| Parameter | All patients (N = 28,347) |
PsO Cohort (N = 9449) |
Matched controls (N = 18,898) | P value |
|---|---|---|---|---|
| Age, mean (SD), years | 47.6 (13.4) | 47.6 (13.4) | 47.6 (13.4) | – |
| Female sex, n (%) | 14,067 (49.6) | 4689 (49.6) | 9378 (49.6) | – |
| Region, n (%) | ||||
| North Central | 6039 (21.3) | 2013 (21.3) | 4026 (21.3) | – |
| Northeast | 5664 (20.0) | 1888 (20.0) | 3776 (20.0) | |
| West | 13,215 (46.6) | 4405 (46.6) | 8810 (46.6) | |
| South | 3429 (12.1) | 1143(12.1) | 2286 (12.1) | |
| Insurance plan type, n (%) | ||||
| EPO & POS | 2056 (7.3) | 647 (6.9) | 1409 (7.5) | < 0.0001 |
| HMO | 2921 (10.3) | 910 (9.6) | 2011 (10.6) | |
| HDP | 6225 (22.0) | 1777 (18.8) | 4448 (23.5) | |
| PPO | 15,173 (53.5) | 5525 (58.5) | 9648 (51.1) | |
| Other | 1972 (7.0) | 590 (6.2) | 1382 (7.3) | |
| CCI score, mean (SD) | 0.33 (0.9) | 0.38 (0.9) | 0.31 (0.9) | < 0.0001 |
| Comorbidities, n (%) | ||||
| Hypertension | 8039 (28.4) | 3140 (33.2) | 4899 (25.9) | < 0.0001 |
| Hyperlipidemia | 7309 (25.8) | 2881 (30.5) | 4428 (23.4) | < 0.0001 |
| Mental healthb | 3738 (13.5) | 1566 (16.6) | 2172 (11.5) | < 0.0001 |
| Diabetes | 3209 (11.9) | 1345 (14.2) | 1864 (9.9) | < 0.0001 |
| Obesity | 2877 (10.2) | 1207 (12.8) | 1670 (8.8) | < 0.0001 |
| Cardiovascular diseasec | 1594 (5.6) | 648 (6.9) | 946 (5.0) | < 0.0001 |
| COPD | 1722 (6.1) | 655 (6.9) | 1067 (5.7) | < 0.0001 |
| Liver diseased | 889 (3.1) | 433 (4.6) | 456 (2.4) | < 0.0001 |
| Peripheral vascular disease | 604 (2.1) | 236 (2.5) | 368 (2.0) | 0.0002 |
| Other autoimmune disorderse | 383 (148) | 174 (1.8) | 209 (1.1) | < 0.0001 |
aComorbidities identified during 1-year baseline; other characteristics as identified on index date
bAnxiety + depression + suicidal ideation
cMyocardial infarction + coronary heart disease + stroke
dMild, moderate, and severe
eAlopecia areata, celiac disease, systemic sclerosis, Sjögren syndrome, vitiligo, chronic urticaria, systemic lupus erythematosus, Addison disease, giant cell arteritis, pulmonary fibrosis, and chronic glomerulonephritis
Note: (1) Age, sex, region, insurance plan type as identified on index date; (2) Comorbidities identified during 1-year baseline
CCI, Charlson comorbidity index; COPD, chronic obstructive pulmonary disorder; EPO, exclusive provider organization; HDP, high deductible plan; HMO, health maintenance organization; POS, point of service; PPO, preferred provider organization; PsO, psoriasis
Adjusted incidence for total medical visits was higher among PsO patients compared with matched controls. Total medical visit rates were higher (P < 0.01) in patients with PsO with mental health disorders (IRR 1.08, 95% CI 1.02–1.14), diabetes (IRR 1.10, 95% CI 1.04–1.17), hyperlipidemia (IRR 1.13, 95% CI 1.08–1.18), hypertension (IRR 1.13, 95% CI 1.09–1.18), liver disease (IRR 1.21, 95% CI 1.07–1.36), and obesity (IRR 1.12, 95% CI 1.05–1.20) compared with matched controls (Table 2).
Table 2.
Adjusted PPPY HCRU and IRRs
| Comorbidity | HCRU (PPPY) PsO cohort (95% CI) |
HCRU (PPPY) matched controls (95% CI) | IRR PsO versus control (95% CI) |
IRR P value |
|---|---|---|---|---|
| Cardiovascular diseasea |
10.02 (9.35–10.75) |
9.58 (9.03–10.17) |
1.05 (0.96–1.14) |
0.3144 |
| Mental healthb |
11.63 (11.10–12.18) |
10.77 (10.35–11.20) |
1.08 (1.02–1.14) |
0.0086 |
| Chronic pulmonary disease |
10.27 (9.57–11.01) |
9.57 (9.05–10.13) |
1.07 (0.98–1.17) |
0.1111 |
| Diabetes |
11.06 (10.53–11.62) |
10.04 (9.62–10.48) |
1.10 (1.04–1.17) |
0.0021 |
| Hyperlipidemia |
11.15 (10.76–11.54) |
9.87 (9.58–10.16) |
1.13 (1.08–1.18) |
< 0.0001 |
| Hypertension |
10.91 (10.55–11.30) |
9.64 (9.37–9.92) |
1.13 (1.09–1.18) |
< 0.0001 |
| Peripheral vascular disease |
9.59 (8.57–10.73) |
9.28 (8.47–10.17) |
1.03 (0.90–1.19) |
0.6541 |
| Liver diseasec |
9.56 (8.73–10.46) |
7.93 (7.25–8.67) |
1.21 (1.07–1.36) |
0.0018 |
| Obesity |
10.88 (10.32–11.46) |
9.71 (9.29–10.16) |
1.12 (1.05–1.20) |
0.0008 |
| Other autoimmune disordersd |
10.09 (8.83–11.54) |
9.57 (8.49–10.79) |
1.05 (0.88–1.26) |
0.5614 |
aMyocardial infarction + coronary heart disease + stroke
bAnxiety + depression + suicidal ideation
cMild, moderate, and severe
dAlopecia areata, celiac disease, systemic sclerosis, Sjögren syndrome, vitiligo, chronic urticaria, systemic lupus erythematosus, Addison disease, giant cell arteritis, pulmonary fibrosis, and chronic glomerulonephritis
ED, emergency department; HCRU, healthcare resource utilization; IRR, incidence risk ratio; PPPY, per patient per year; PsO, psoriasis
Compared with matched controls, adjusted total medical costs per patient per month (PPPM) were higher (P < 0.01) for patients with PsO for all comorbidities except for cardiovascular disease and other autoimmune disorders (Table 3). Among the comorbidities that had significant differences, those with the greatest magnitude were peripheral vascular disease ($987; P < 0.0001), mental health disorders ($372; P < 0.0001), liver disease ($360; P < 0.0001), and hypertension ($305; P < 0.0001).
Table 3.
Mean (95% CI) adjusted total medical costsa PPPM (2020 USD)
| Comorbidity | PsO cohort ($) | Matched controls ($) | Difference ($) | P value |
|---|---|---|---|---|
| Cardiovascular diseaseb |
732.18 (636.61–843.41) |
655.28 (583.01–736.26) |
76.90 | 0.2191 |
| Mental healthc |
910.53 (832.35–996.06) |
538.15 (498.01–581.53) |
372.38 | < 0.0001 |
| Chronic pulmonary disease |
581.51 (505.67–668.72) |
447.00 (400.39–499.04) |
134.51 | 0.0027 |
| Diabetes |
658.45 (596.50–726.85) |
499.87 (459.36–543.96) |
158.58 | < 0.0001 |
| Hyperlipidemia |
723.39 (675.44–774.73) |
520.64 (491.30–551.74) |
202.75 | < 0.0001 |
| Hypertension |
840.61 (787.49–897.32) |
535.30 (506.11–566.18) |
305.31 | < 0.0001 |
| Peripheral vascular disease |
1496.28 (1191.58–1878.89) |
508.82 (423.63–611.15) |
987.46 | < 0.0001 |
| Liver diseased |
689.40 (572.21–830.58) |
329.46 (275.60–393.85) |
359.94 | < 0.0001 |
| Obesity |
731.93 (660.53–811.05) |
586.55 (537.33–640.29) |
145.38 | 0.0009 |
| Other autoimmune disorderse |
572.79 (440.19–745.33) |
519.13 (408.22–660.18) |
53.99 | 0.5869 |
aSum of inpatient, outpatient, and emergency department–adjusted costs
bMyocardial infarction + coronary heart disease + stroke
cAnxiety + depression + suicidal ideation
dMild, moderate, and severe
eAlopecia areata, celiac disease, systemic sclerosis, Sjögren syndrome, vitiligo, chronic urticaria, systemic lupus erythematosus, Addison disease, giant cell arteritis, pulmonary fibrosis, and chronic glomerulonephritis
PPPM, per patient per month; PsO, psoriasis; USD, US dollars
Antidepressant, antidiabetic, and cardiovascular/antihypertensive agent medication use, corresponding pharmacy prescription fills, and inpatient length of stay were higher in the PsO cohort compared with the matched controls (Tables 4–6). Antidepressant and antidiabetic PPPM pharmacy costs were higher in the PsO cohort ($3.59 versus $2.92, and $6.71 versus $5.77; P < 0.01, respectively); however, cardiovascular drugs/antihypertensives were comparable across groups ($9.42 versus $9.44; P = 0.93) (Table 7). The sensitivity analysis excluding HCRU visits and costs of PsO index treatment from pharmacy visits/costs found adjusted pharmacy visits to be generally lower in the PsO cohort (diabetes: IRR 0.88, 95% CI 0.83–0.93, P < 0.0001; hypertension: IRR 0.95, 95% CI 0.91–0.98, P = 0.0028; peripheral vascular disease: IRR 0.85, 95% CI 0.75–0.97, P = 0.0150; Table 8). However, the resulting adjusted pharmacy costs were still significantly higher in the PsO cohort for mental health disorders, chronic pulmonary disease, diabetes, hyperlipidemia, hypertension, liver disease, and obesity.
Table 5.
Adjusted count of total unique pharmacy fills in follow-up
| Medication | Cohort | Adjusted Count Rx filled | Adjusted Count 95% CI | IRR (PsO–Control) | IRR 95% CI | P value |
|---|---|---|---|---|---|---|
| Antidepressants | PsO | 0.48 | 0.45–0.52 | 1.37 | 1.28–1.48 | < .0001 |
| Control | 0.35 | 0.33–0.37 | ||||
| Antidiabetic drugs | PsO | 0.20 | 0.18–0.22 | 1.48 | 1.34–1.63 | < .0001 |
| Control | 0.13 | 0.12–0.15 | ||||
| Cardiovascular drugs or antihypertensive agents | PsO | 1.71 | 1.63–1.80 | 1.27 | 1.21–1.34 | < .0001 |
| Control | 1.35 | 1.30–1.40 |
CI, confidence interval; IRR, incidence rate ratio; PsO, psoriasis; Rx, pharmacy prescription
Table 4.
Adjusted medication usea
| Medication of interest | Conditional odds ratio (PsO versus control) | 95% CI | P value |
|---|---|---|---|
| Antidepressants | 1.42 | 1.26-1.60 | < .0001 |
| Antidiabetic drugs | 1.43 | 1.19-1.71 | 0.0001 |
| Cardiovascular/antihypertensive agents | 1.26 | 1.14-1.40 | < .0001 |
aMedication use was a binary 0/1 variable
CI, confidence interval; PsO, psoriasis
Table 6.
Adjusted inpatient total length of stay, in days
| Cohort | Adjusted total inpatient LOS | Adjusted total inpatient LOS 95% CI | IRR (PsO versus control) | IRR 95% CI | P value |
|---|---|---|---|---|---|
| PsO | 0.17 | 0.12–0.23 | 1.58 | 1.24–2.02 | 0.0002 |
| Control | 0.11 | 0.08–0.14 |
CI, confidence interval; IRR, incidence rate ratio; LOS, length of stay; PsO, psoriasis
Table 7.
Adjusted pharmacy prescription costs per-patient per-month, USD
| Comorbidity | Cohort | Adjusted Rx cost (PPPM, $) | Adjusted Rx cost 95% CI ($) | Difference (PsO–control, $) |
P value |
|---|---|---|---|---|---|
| Antidepressants | PsO | 3.59 | 3.44–3.76 | 0.67 | < .0001 |
| Control | 2.92 | 2.82–3.02 | |||
| Antidiabetic drugs | PsO | 6.71 | 6.38–7.06 | 0.94 | < .0001 |
| Control | 5.77 | 5.54–6.01 | |||
| Cardiovascular drugs or antihypertensive agents | PsO | 9.42 | 9.00–9.87 | −0.02 | 0.9327 |
| Control | 9.44 | 9.11–9.78 |
CI, confidence interval; Rx, pharmacy prescription; PsO, psoriasis; USD, US dollars
Table 8.
Adjusted pharmacy healthcare resource utilization, excluding psoriasis-related index treatment visits
| Comorbidity | Cohort | Adjusted HCRU (PPPY) | Adjusted HCRU 95% CI |
IRR (PsO versus control) |
IRR 95% CI |
P value |
|---|---|---|---|---|---|---|
| Diabetes | PsO | 8.94 | 8.55–9.35 | 0.88 | 0.83–0.93 | < .0001 |
| Control | 10.16 | 9.77–10.55 | ||||
| Hyperlipidemia | PsO | 9.72 | 9.41–10.04 | 0.98 | 0.94–1.01 | 0.2021 |
| Control | 9.96 | 9.70–10.23 | ||||
| Hypertension | PsO | 9.81 | 9.51–10.12 | 0.95 | 0.91–0.98 | 0.0028 |
| Control | 10.35 | 10.09–10.62 | ||||
| Peripheral vascular disease | PsO | 7.48 | 6.75–8.30 | 0.85 | 0.75–0.97 | 0.0150 |
| Control | 8.79 | 8.09–9.55 | ||||
| Liver disease (mild, moderate, or severe) | PsO | 8.51 | 7.83–9.24 | 0.93 | 0.83–1.03 | 0.1643 |
| Control | 9.18 | 8.46–9.96 | ||||
| Obesity | PsO | 9.11 | 8.69–9.56 | 0.96 | 0.90–1.02 | 0.1786 |
| Control | 9.50 | 9.12–9.90 | ||||
| Peptic ulcer | PsO | 6.55 | 5.02–8.56 | 0.90 | 0.65–1.26 | 0.5414 |
| Control | 7.27 | 5.94–8.91 | ||||
| Other autoimmune disorders | PsO | 8.35 | 7.36–9.47 | 0.96 | 0.81–1.14 | 0.6365 |
| Control | 8.69 | 7.78–9.70 |
CI, confidence interval; HCRU, healthcare-related resource use; IRR, incidence rate ratio; PPPY, per-patient per-year
Discussion
With respect to several comorbidities, there are significant differences in both all-cause HCRU and all-cause medical costs for patients with moderate to severe PsO who initiated treatment with apremilast, a TNFi, or ustekinumab compared with matched controls from the general population.
Previous studies of patients with PsO and patients with other autoimmune disorders, such as inflammatory bowel disease or systemic lupus erythematosus, focused on differences in HCRU between treatment groups or between treated and untreated patients, without regard to comorbidities [13–15]. Our study, which focused specifically on patients with PsO and other comorbid conditions, confirmed these trends with respect to adjusted HCRU, namely that patients with PsO showed a higher incidence of total medical visits than their non-PsO counterparts. Moreover, our study demonstrated that differences in HCRU were associated with specific comorbidities, including mental health disorders, diabetes, hyperlipidemia, hypertension, liver disease, and obesity. Patients with PsO and these comorbidities had a rate of medical visits 1.08–1.13 times that of a matched control population.
Regarding costs, few studies have quantified the effect of comorbidities in total medical costs for patients with moderate to severe PsO, focusing instead on other cost drivers, including switching or discontinuing biologic therapy, among others [12, 16–19]. Nonetheless, our study confirmed an association between comorbidities and increased costs [5–7]. Specifically, of the ten comorbidities considered in this study, all but two—cardiovascular disease and other autoimmune disorders—showed a significant relationship to PPPM costs. The increased total medical costs ranged in magnitude from a 30% to 194% increase in PPPM costs for the PsO cohort, suggesting that comorbidity status is another factor to consider when examining cost differences across patient populations with PsO.
Given the limited number of studies on the economic burden of comorbidities among patients with moderate to severe PsO, our data may be useful in exploring the dynamics that characterize HCRU and costs within a specific setting. Our data suggest that comorbidities are generally linked to higher HCRU and costs, and the relationships are comorbidity specific and extend to multiple treatment settings. Compared with matched controls, for example, patients with PsO had a greater number of total medical visits related to the comorbidities studied.
A key strength of this study is the use of data from a large US claims database that is national in scope, provides a high level of diversity, and represents overall trends in the managed care setting. In addition, the database is comprehensive, incorporating all medical and pharmacy claims of patients and allowing for longitudinal analysis of a large patient sample. Similarly, this retrospective analysis provides a better understanding of the PsO population in real-world clinical practice compared with the controlled conditions of a clinical trial, in part by allowing observation of patients who are often underrepresented in clinical trials, such as those with comorbidities, multiple treatment failures, and greater baseline disease severity, and those who are elderly [20–23]. Additionally, real-world studies offer insight into treatment patterns and the effectiveness of newly approved therapies in typical dermatologic practice [20–23]. Since prescribing patterns in the real world are broader and less limiting, the retrospective analysis provides a more comprehensive picture of how medications are used by clinicians in routine practice and the adherence to treatments. Importantly, the data analyzed in this study capture the use of PsO medications.
Nonetheless, and as with all studies utilizing healthcare claims databases, there are limitations inherent to the use of claims data. Claims are submitted by healthcare providers to insurance companies for reimbursement. Such claims are subject to possible coding errors, coding for the purpose of rule-out rather than actual disease, and undercoding, without the possibility of verifying reported diagnoses. For medications captured in the outpatient pharmacy, it is uncertain whether patients actually administered the medications. Additionally, it was not possible to measure the severity of comorbidity within the database, and there could be an imbalance in the severity of comorbidities between the PsO and the general population studied.
Conclusions
This study described and compared all-cause HCRU and all-cause medical costs associated with comorbidities in patients with moderate to severe PsO who initiated treatment with apremilast, TNFi, or ustekinumab compared with matched controls from a general population. Patients with PsO in this study experienced a higher economic burden of comorbidities, ranging from a 30% to 194% increase in total medical costs for specific comorbidities (chronic obstructive pulmonary disorder and peripheral vascular disease, respectively) compared with the general population, despite using currently available systemic treatments for PsO.
Acknowledgements
Funding
This study was sponsored by Bristol Myers Squibb. Funding for the journal’s Rapid Review Service was provided by Bristol Myers Squibb.
Medical Writing, Editorial, and Other Assistance
Medical writing and editorial assistance was provided by Nicole Boyer, PhD, of Peloton Advantage, LLC, an OPEN Health company, and funded by Bristol Myers Squibb.
Author Contributions
JJW, MS, DD, VP, and LS provided substantial contributions to the study design. MS and AJ participated in data acquisition and data analysis. JJW, MS, DD, VP, AJ, and LS participated in data interpretation. All authors had full access to the data and contributed to the drafting, critical review, and revision of the manuscript, with the support of a medical writer provided by Bristol Myers Squibb. All authors granted approval of the final manuscript for submission.
Disclosures
JJW is or has been an investigator for AbbVie, Amgen, Eli Lilly, Janssen, Novartis, and Pfizer; a consultant for AbbVie, Almirall, Amgen, Arcutis, Aristea Therapeutics, Bausch Health, Boehringer Ingelheim, Bristol Myers Squibb, Dermavant, DermTech, Dr. Reddy's Laboratories, Eli Lilly, EPI Health, Galderma, Janssen, LEO Pharma, Mindera Health, Novartis, Regeneron, Samsung Bioepis, Sanofi Genzyme, Solius, Sun Pharmaceutical, UCB, and Zerigo Health; and a speaker for AbbVie, Amgen, Bausch Health, Novartis, Regeneron, Sanofi Genzyme, Sun Pharmaceutical, and UCB. MS, DD, VP, and LS are employees and shareholders of Bristol Myers Squibb. AJ is an employee of Mu Sigma, which has received consulting fees from Bristol Myers Squibb.
Compliance with Ethics Guidelines
This study used data from the MarketScan database. Access to the database was granted by MarketScan under license. No patients were directly involved in the study, and only de-identified patient information was used; thus, institutional review board approval was waived.
Data Availability
The Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.
References
- 1.Mustonen A, Leino M, Mattila K, Koulu L, Tuominen R. Treatment costs of psoriasis in a tertiary-level clinic. BMC Health Serv Res. 2014;14:344. doi: 10.1186/1472-6963-14-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu J, Thatiparthi A, Martin A, Egeberg A, Wu JJ. Prevalence of psoriasis among adults in the US 2009–2010 and 2013–2014 National Health and Nutrition Examination Surveys. J Am Acad Dermatol. 2021;84(3):767–769. doi: 10.1016/j.jaad.2020.10.035. [DOI] [PubMed] [Google Scholar]
- 3.Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20(6):1475. doi: 10.3390/ijms20061475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global Report on Psoriasis. Switzerland: World Health Organization; 2016.
- 5.Feldman SR, Zhao Y, Shi L, Tran MH. Economic and comorbidity burden among patients with moderate-to-severe psoriasis. J Manag Care Spec Pharm. 2015;21(10):874–888. doi: 10.18553/jmcp.2015.21.10.874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kimball AB, Guérin A, Tsaneva M, et al. Economic burden of comorbidities in patients with psoriasis is substantial. J Eur Acad Dermatol Venereol. 2011;25(2):157–163. doi: 10.1111/j.1468-3083.2010.03730.x. [DOI] [PubMed] [Google Scholar]
- 7.Crown WH, Bresnahan BW, Orsini LS, Kennedy S, Leonardi C. The burden of illness associated with psoriasis: cost of treatment with systemic therapy and phototherapy in the US. Curr Med Res Opin. 2004;20(12):1929–1936. doi: 10.1185/030079904X15192. [DOI] [PubMed] [Google Scholar]
- 8.Ruggiero A, Fabbrocini G, Cacciapuoti S, Cinelli E, Gallo L, Megna M. Ocular manifestations in psoriasis screening (OcMaPS) questionnaire: a useful tool to reveal misdiagnosed ocular involvement in psoriasis. J Clin Med. 2021;10(5):1031. doi: 10.3390/jcm10051031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeung H, Takeshita J, Mehta NN, et al. Psoriasis severity and the prevalence of major medical comorbidity: a population-based study. JAMA Dermatol. 2013;149(10):1173–1179. doi: 10.1001/jamadermatol.2013.5015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80(4):1073–1113. doi: 10.1016/j.jaad.2018.11.058. [DOI] [PubMed] [Google Scholar]
- 11.Brezinski EA, Dhillon JS, Armstrong AW. Economic burden of psoriasis in the United States: a systematic review. JAMA Dermatol. 2015;151(6):651–658. doi: 10.1001/jamadermatol.2014.3593. [DOI] [PubMed] [Google Scholar]
- 12.Wu JJ, Pelletier C, Ung B, Tian M. Real-world treatment patterns and healthcare costs among biologic-naive patients initiating apremilast or biologics for the treatment of psoriasis. J Med Econ. 2019;22(4):365–371. doi: 10.1080/13696998.2019.1571500. [DOI] [PubMed] [Google Scholar]
- 13.Fonia A, Jackson K, Lereun C, Grant DM, Barker JN, Smith CH. A retrospective cohort study of the impact of biologic therapy initiation on medical resource use and costs in patients with moderate to severe psoriasis. Br J Dermatol. 2010;163(4):807–816. doi: 10.1111/j.1365-2133.2010.09944.x. [DOI] [PubMed] [Google Scholar]
- 14.Hudesman DP, Chakravarty SD, Emond B, et al. Healthcare resource utilization and costs associated with inflammatory bowel disease among patients with chronic inflammatory diseases: a retrospective cohort study. BMC Rheumatol. 2020;4:16. doi: 10.1186/s41927-020-0115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwarting A, Friedel H, Garal-Pantaler E, et al. The burden of systemic lupus erythematosus in Germany: incidence, prevalence, and healthcare resource utilization. Rheumatol Ther. 2021;8(1):375–393. doi: 10.1007/s40744-021-00277-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feldman SR, Tian H, Wang X, Germino R. Health care utilization and cost associated with biologic treatment patterns among patients with moderate to severe psoriasis: analyses from a large U.S. claims database. J Manag Care Spec Pharm. 2018;25(4):479–88. [DOI] [PMC free article] [PubMed]
- 17.Kaplan DL, Ung BL, Pelletier C, Udeze C, Khilfeh I, Tian M. Switch rates and total cost of care associated with apremilast and biologic therapies in biologic-naive patients with plaque psoriasis. Clinicoecon Outcomes Res. 2020;12:369–377. doi: 10.2147/CEOR.S251775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palmer JB, Li Y, Herrera V, Liao M, Tran M, Ozturk ZE. Treatment patterns and costs for anti-TNFα biologic therapy in patients with psoriatic arthritis. BMC Musculoskelet Disord. 2016;17:261. doi: 10.1186/s12891-016-1102-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Long GH, Tatro AR, Oh YS, Reddy SR, Ananthakrishnan AN. Analysis of safety, medical resource utilization, and treatment costs by drug class for management of inflammatory bowel disease in the United States based on insurance claims data. Adv Ther. 2019;36(11):3079–3095. doi: 10.1007/s12325-019-01095-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Megna M, Cinelli E, Gallo L, Camela E, Ruggiero A, Fabbrocini G. Risankizumab in real life: preliminary results of efficacy and safety in psoriasis during a 16-week period. Arch Dermatol Res. 2022;314(6):619–623. doi: 10.1007/s00403-021-02200-7. [DOI] [PubMed] [Google Scholar]
- 21.Ruggiero A, Fabbrocini G, Cinelli E, Megna M. Real world practice indirect comparison between guselkumab and risankizumab: Results from an Italian retrospective study. Dermatol Ther. 2022;35(1):e15214. doi: 10.1111/dth.15214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruggiero A, Fabbrocini G, Cinelli E, Ocampo Garza SS, Camela E, Megna M. Anti-interleukin-23 for psoriasis in elderly patients: guselkumab, risankizumab and tildrakizumab in real-world practice. Clin Exp Dermatol. 2022;47(3):561–567. doi: 10.1111/ced.14979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caldarola G, Galluzzo M, Bernardini N, et al. Tildrakizumab in moderate-to-severe plaque psoriasis: A multicenter, retrospective, real-life study. Dermatol Ther. 2022;35(6):e15488. doi: 10.1111/dth.15488. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.