Figure 2.
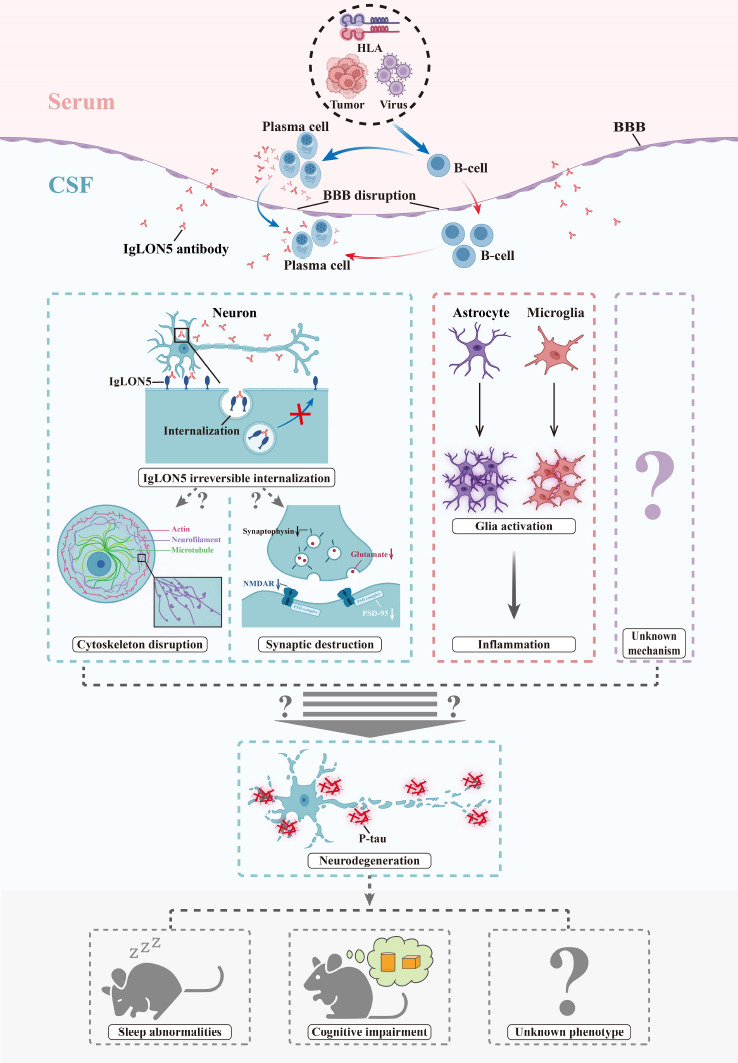
The possible mechanisms underlying the pathophysiology of anti-IgLON5 disease.
HLA genotypes, viruses, and tumors are the probable triggers of anti-IgLON5 disease in clinical cases; these may induce B cell immunity. B cells may differentiate into plasma cells and produce IgLON5 antibodies in the peripheral blood. Moreover, lymphocytes may infiltrate the central nervous systems through the disrupted BBB. Peripheral infiltration or intrathecal synthesis of IgLON5 antibodies can further cause neuronal damage via two or more possible mechanisms. These include the irreversible internalization of IgLON5 and the induction of inflammation in the microenvironment, such as glia activation. The internalization of IgLON5 may lead to the disruption of the cytoskeleton and synapses through unknown mechanisms. Finally, the resulting neuronal damage may be the cause of the neurodegeneration and p-tau deposition observed during pathological examination. In addition to the already identified pathways, there may be other as yet unknown mechanisms that could lead to neurodegeneration. BBB: Blood-brain barrier; CSF: cerebrospinal fluid; HLA: human leukocyte antigen.
