Background:
The Plastic Surgery Common Application (PSCA) was introduced as a free and specialty-specific application for plastic surgery applicants in the 2020–2021 cycle. Now in its second year, the PSCA is being piloted by all integrated residency programs with future plans to replace Electronic Residency Application Service (ERAS) in the 2022–2023 cycle. This study aimed to explore applicant perspectives related to the PSCA and ERAS applications.
Methods:
An anonymous survey was distributed to integrated plastic surgery residency applicants from the 2021–2022 application cycle. Participants were asked to provide basic demographic information, their perspectives of the PSCA, and overall application preference.
Results:
One hundred forty (43.1%) applicants completed the survey. Nearly, 63% of applicants responded “slightly well” or “not well at all” regarding their ability to highlight at least one aspect of their application. Forty-one percent of applicants believed ERAS best highlighted the strengths of their application compared with 27% who believed their strengths were better highlighted by the PSCA. Seventy-nine percent reported the cost savings associated with the PSCA were “very” or “extremely important.” Overall, 63% of respondents reported a preference to apply with the PSCA alone.
Conclusions:
This is the first study to provide insight on applicants' perspectives of the PSCA. Although the majority preferred applying with the PSCA, there may be challenges with transitioning to this application solely. Future iterations of the PSCA may aim to ameliorate functionality concerns, optimize application content, and incorporate plastic surgery-specific information that may be important to selection committees.
Takeaways
Question: What is the integrated plastic surgery applicant perspective on the plastic surgery common application (PSCA) compared to ERAS?
Findings: Sixty-three percent of applicants reported a preference to apply with the PSCA alone. Seventy-nine percent reported that the cost savings associated with the PSCA were “very” or “extremely important.” Sixty-three percent of applicants responded “slightly well” or “not well at all” regarding their ability to highlight at least one aspect of their application with the PSCA.
Meaning: Integrated plastic surgery residency applicants are in favor of an alternative and cost-mitigating application that allows them to showcase their experiences and accolades while being user friendly.
INTRODUCTION
Integrated plastic surgery residency is the most competitive specialty per the National Resident Matching Program match, with a successful match rate of 72.1% in 2020, the lowest among all specialties.1 In an effort to maximize the probability of successfully matching, many applicants apply to most, if not all, available training programs.2 Since its establishment in 1995, Electronic Residency Application Service (ERAS) has become the dominant application service for applying to plastic surgery residency in the United States. Despite its widespread use among most specialties, ERAS is associated with high costs to applicants who may spend up to $2000 sending their application to residency programs.3
In an effort to promote a more equitable application process, the Plastic Surgery Common Application (PSCA) was developed.4,5 This application is unique in that it is free for applicants and allows for the incorporation of plastic surgery-specific content.5 The pilot of the PSCA during the 2020–2021 application cycle was reportedly met with positive reviews from both applicants and participating programs.5 In response, the American Council of Academic Plastic Surgeons (ACAPS) elected to sponsor a specialty-wide pilot of the PSCA for the 2021–2022 application cycle with the plan to replace ERAS for the 2022–2023 academic year.4
To better understand the effects of the proposed transition from ERAS to the PSCA, this study aims to compare the perspectives of plastic surgery applicants during the 2021–2022 cycle regarding the strengths and weaknesses of the PSCA and ERAS. Additionally, this study aims to evaluate applicant preferences and provide recommendations for future efforts to develop an application customized for integrated plastic surgery applicants.
METHODS
Study Participants
Our hospital’s institutional review board reviewed and granted exempt status for the study (protocol 2021P000596). All applicants interested in the integrated plastic surgery residency program at our institution during the 2021–2022 application cycle were recruited as participants. A total of 325 potential participants were identified. An email detailing study objectives with a link to the REDCap electronic survey was distributed to all potential participants on November 5, 2021. Four reminder e-mails were sent, and the survey was closed on November 30, 202l.
Survey Content
Participants were asked to provide demographic information as well as information relating to components of their application. Next, participants were asked to rate how well they were able to highlight certain aspects of their application on a Likert scale ranging from 1 (not well at all) to 5 (extremely well). Participants were then asked whether the PSCA or ERAS better highlighted the strengths and weaknesses of their application. Finally, preference for applying to plastic surgery residency using the PSCA and/or ERAS applications as well as thoughts on the future of the PSCA was evaluated. (See survey, Supplemental Digital Content 1, which displays perspectives of the PSCA survey, http://links.lww.com/PRSGO/C348.)
Statistical Analysis
Analysis was performed using STATA statistical software (STATA Corp., version 16.1). Adjusted multinomial logistic regression modeling was used to evaluate associations between groups and overall application preference. A P value of less than 0.05 was considered significant. For questions with free-text responses, equivalent phrases and statements were identified within the body of the response and counted as the same answer to simplify quantification of our results and understand overarching qualitative themes.
RESULTS
Demographics
Of the 325 surveys provided to our institution’s integrated plastic surgery applicants, a total of 140 responses were received for a response rate of 43.1%. Most respondents (88.6%) were United States allopathic (MD) applicants with international medical graduates comprising another 10.7% (Table 1). Roughly 49% of respondents identified as men and 46% identified as women. The most common race applicants identified as was White (62.1%), with Asian being the second most common (17.1%). The regional distribution of the respondents was as follows: South (27.5%), Midwest (25.4%), Northeast (23.3%), West (11.3%), and International (10.7%).
Table 1.
Respondent Demographics, n (%)
| Respondent Characteristics | Number (%) |
|---|---|
| Medical degree program | |
| United States allopathic (MD) | 124 (88.6) |
| United States osteopathic (DO) | 1 (0.7) |
| International medical degree | 15 (10.7) |
| Gender | |
| Female | 65 (46.4) |
| Male | 68 (48.6) |
| Nonbinary | 4 (2.9) |
| Prefer not to say | 3 (2.1) |
| Race | |
| White | 87 (62.1) |
| Black/African American | 8 (5.7) |
| Asian | 24 (17.1) |
| Other | 17 (12.1) |
| Prefer not to say | 3 (2.1) |
| Region of medical school | |
| Northeast | 33 (23.2) |
| South | 39 (27.5) |
| Midwest | 36 (25.4) |
| West | 16 (11.3) |
| International | 15 (10.7) |
Application Information
Twenty-eight percent of respondents attended a top 40 medical school based on the U.S. News & World Report 2022 Research Rankings (Table 2).6 Thirty-three percent of respondents reported being inducted into their medical school’s chapter of Alpha Omega Alpha (AOA). The mean (SD) United States Medical Licensing Exam (USMLE) step 1 and 2 scores reported by the respondents were 246 (14) and 254 (14), respectively. Twenty-nine percent of respondents reported spending one or more years of dedicated research during or after medical school.
Table 2.
Respondent Application Information
| Application Information | n (%) |
|---|---|
| USMLE step examination scores* | |
| Step 1 | 246 (SD, 14) |
| Step 2 | 254 (SD, 14) |
| AOA status | |
| Inducted | 46 (32.9) |
| Not inducted | 56 (40.0) |
| School does not have a chapter | 38 (27.1) |
| Medical school ranking† | |
| Top 40 | 39 (27.9) |
| Other | 101 (72.1) |
| Medical school class rank‡ | |
| Top third | 12 (21.4) |
| Middle third | 5 (8.9) |
| Bottom third | 1 (1.8) |
| Top quartile | 25 (44.6) |
| Second quartile | 7 (12.5) |
| Third quartile | 4 (7.1) |
| Bottom quartile | 2 (3.6) |
| Research productivity* | |
| Research experiences | 6.6 (5.5) |
| Abstracts, posters, and oral presentations | 13.7 (13.6) |
| Peer-reviewed publications (accepted + submitted) | 12.4 (12.4) |
| Dedicated research time | |
| Yes, 1 y | 28 (20.0) |
| Yes, more than 1 y | 12 (8.6) |
| No | 100 (71.4) |
| Participating in the couples' match | |
| Yes | 11 (7.9) |
| No | 129 (92.1) |
| Additional graduate-level degrees | |
| MBA | 4 (2.9) |
| MPH | 5 (3.6) |
| PhD | 3 (2.1) |
| MS | 17 (12.1) |
| Other | 7 (5.0) |
| None | 105 (75.0) |
Values for USMLE Step Examination scores and research productivity (experiences, abstracts/presentations, and publications) were calculated as mean (SD).
Medical school ranking based on U.S. News & World Report 2022 Research Rankings and included in survey for reference.6
Forty percent (56/140) of respondent’s medical schools ranked students and were included in this table.
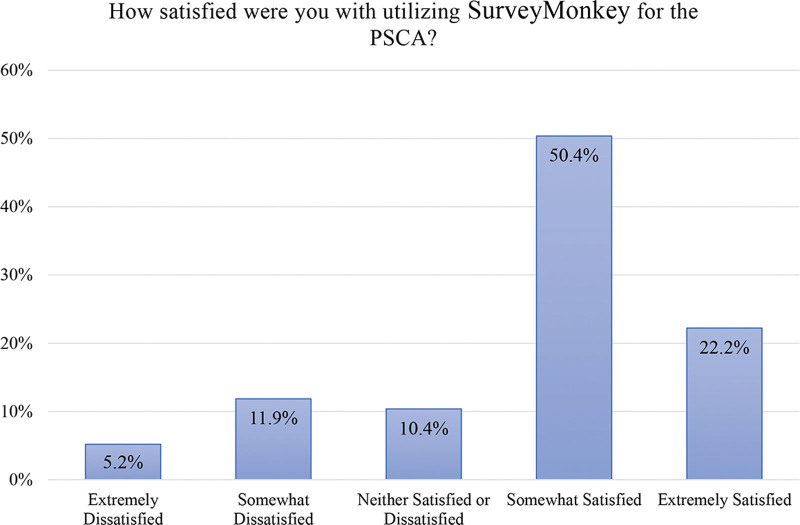
Perspectives on the SurveyMonkey/Momentive Apply Survey Tool Used for the PSCA
Most (72.6%) respondents felt “somewhat” or “extremely satisfied” with the SurveyMonkey/Momentive Apply survey tool utilized by the PSCA (Fig. 1). Of the 17% who reported being “very” or “extremely dissatisfied” by the SurveyMonkey tool, qualitative analysis of free responses revealed that the most common reasons for dissatisfaction were related to the process of obtaining letters of recommendation, a lack of technical support offered by the application platform, and a difficult to navigate user interface.
Fig. 1.
Satisfaction with SurveyMonkey survey tool.
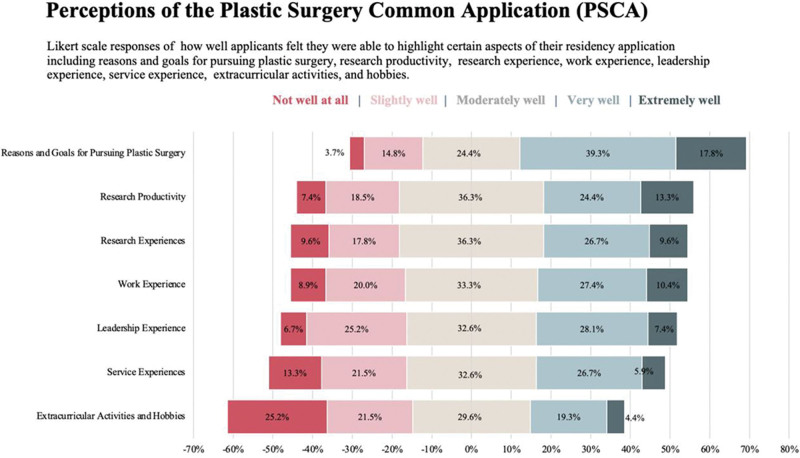
Perspectives on the PSCA Content
Applicants were asked to disclose how well they were able to highlight different aspects of their residency application with the PSCA (Fig. 2). Overall, 57% of applicants felt that they were able to highlight the reasons and goals for pursuing plastic surgery as a career “very” or “extremely well.” Over a third of the applicants who responded felt they were able to highlight their research productivity (38%) and experiences (36%) “very” or “extremely well.” There were a range of responses when applicants were asked how effective the PSCA was able to highlight other experiences on their application (Fig. 2). Nearly 63% (88/140) of applicants answered “slightly well” or “not well at all” regarding their ability to highlight at least one aspect of their application. The limited number of entries for experiences (89.8%, 79/88) and limited word count for detailing experiences (56.8%, 50/88) were the most commonly cited reasons for those who reported answers of “slightly well” or “not well at all.”
Fig. 2.
Perspectives on PSCA content.
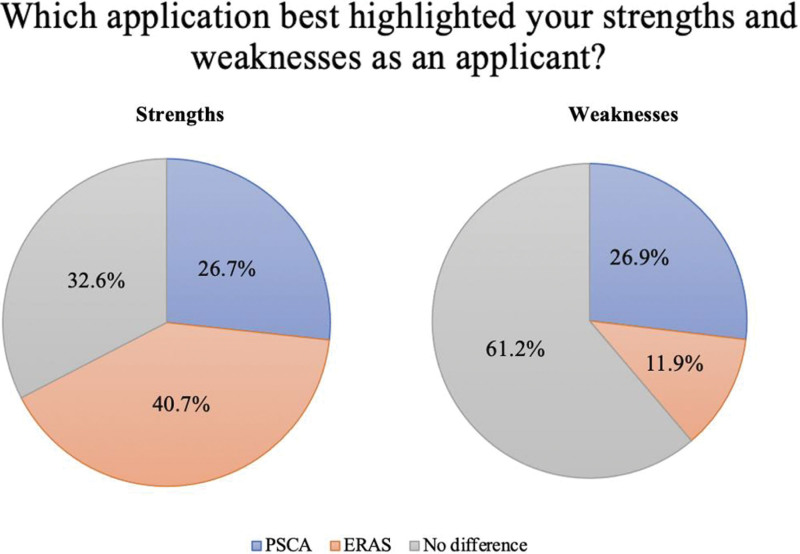
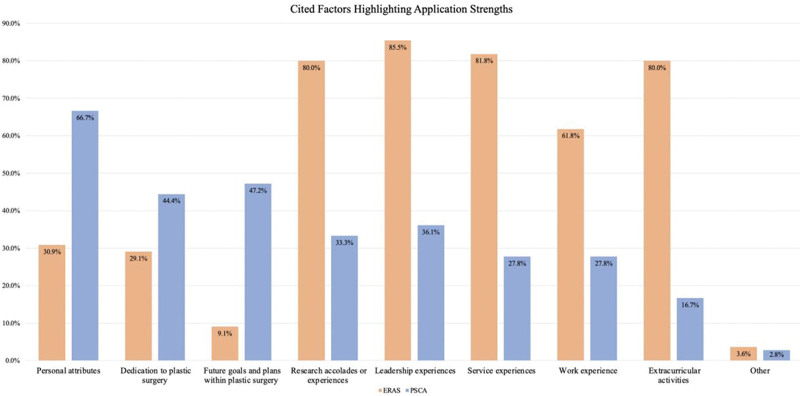
Strengths and Weaknesses: PSCA versus ERAS
Applicants were then asked to report whether they believed the PSCA or ERAS better highlighted their perceived strengths and weaknesses as an applicant. Forty-one percent of applicants believed that ERAS best highlighted the strengths of their application compared with 27% who believed their strengths were better represented with the PSCA (Fig. 3). Another 33% believed that there was no difference in highlighting overall strengths between the two applications. For those who believed ERAS better highlighted their strengths, most believed ERAS performed better at highlighting experiences related to service, leadership, research, work, and extracurricular activities (Fig. 4). In contrast, those who believed the PSCA better highlighted their strengths cited this application allowed them to better highlight personal attributes, dedication to plastic surgery, and future goals and plans within plastic surgery.
Fig. 3.
Application that best highlighted strengths and weaknesses.
Fig. 4.
Strengths highlighted based on application.
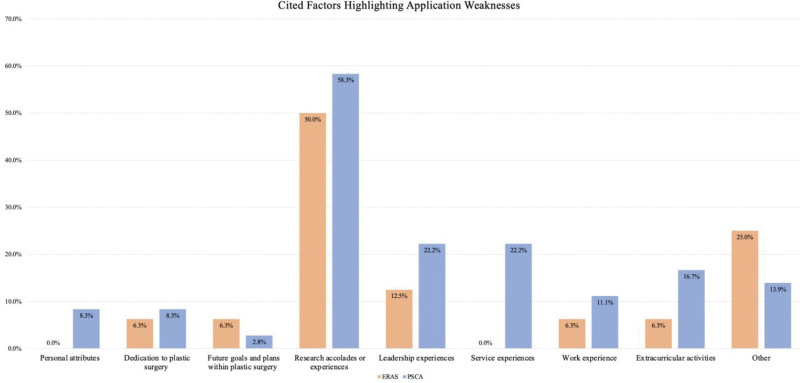
When asking whether the PSCA or ERAS highlighted the applicant’s perceived weaknesses of their application, 61% reported there was no difference (Fig. 3). Another 27% reported that the PSCA highlighted weaknesses of their application, whereas 12% believed their weaknesses were more apparent with ERAS. Of the 27% who believed the PSCA better highlighted their weaknesses, 58% reported that the format of the PSCA did not allow for research accolades and experiences to be well represented (Fig. 5). Of the 12% who believed ERAS better highlighted their weaknesses, 50% also cited research accolades and experiences. Figures 4 and 5 provide more granular and detailed information on the specific components of each application that were captured better or worse and may be valuable in finding novel solutions in future iterations of the plastic surgery residency application.
Fig. 5.
Weaknesses highlighted based on application.
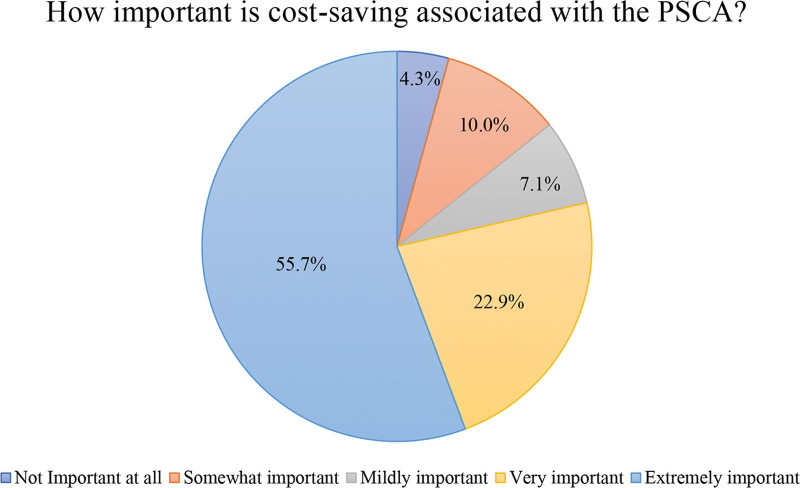
Most respondents (70.4%) believed that the short answer prompts of the PSCA added meaningful information that ERAS did not capture, while only 46% of respondents felt these would help them receive interview invitations. The majority (79%) of the respondents reported that the cost savings associated with the PSCA were “very” or “extremely important” (Fig. 6).
Fig. 6.
Importance of cost savings with the PSCA.
Overall Application Preference
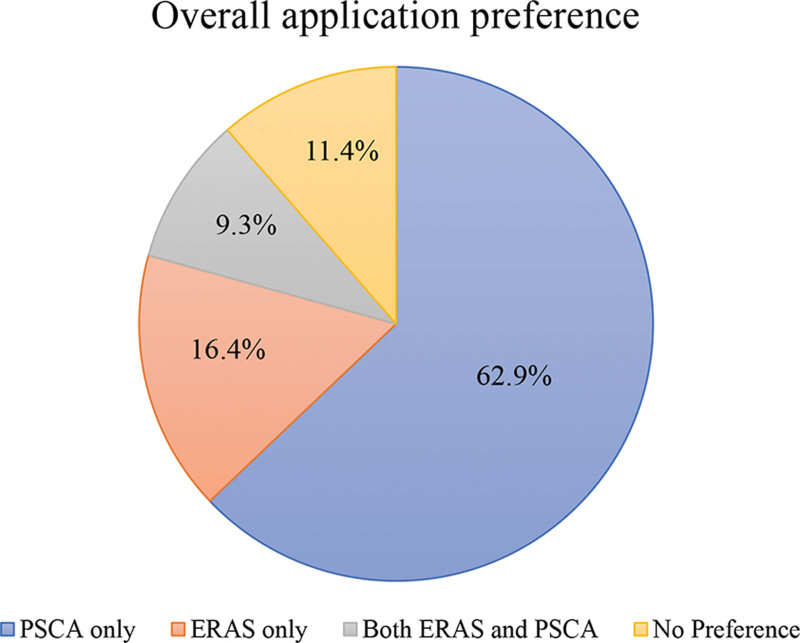
When asked which application was preferred when applying to integrated plastic surgery residency programs, 63% chose the PSCA alone. An additional 16.4% preferred to apply with ERAS and 11.4% had no preference (Fig. 7). On multivariable logistical regression analysis, we found that respondents who identified as Asian and those who identified as “other/prefer not to say” were significantly more likely to prefer ERAS when compared with respondents who identified as White (P < 0.05) (Table 3). Additionally, applicants who reported cost savings as “very” or “extremely” important and those who performed a year of dedicated research were significantly more likely to prefer the PSCA over ERAS (P < 0.05).
Fig. 7.
Overall preferred application.
Table 3.
Multinomial Logistic Regression Analysis for Application Preference
| Factors for Preference of ERAS over PSCA Application | |||
|---|---|---|---|
| Variable | RRR | 95% CI | P |
| Degree of applicant | |||
| MD | Reference | ||
| Other (IMG and DO) | 1.01 | 0.01 – 111.96 | 0.99 |
| Sex | |||
| Male | Reference | ||
| Female | 1.81 | 0.36–9.05 | 0.47 |
| Other/prefer not to say | 3.49 | 0.12–103.0 | 0.47 |
| Race* | |||
| White | Reference | ||
| Asian | 17.28 | 1.83–163.08 | 0.01* |
| Other/prefer not to say | 30.03 | 2.05–440.26 | 0.01* |
| Region | |||
| Midwest | Reference | ||
| Northeast | 9.81 | 0.72–133.0 | 0.09 |
| South | 9.30 | 0.93–93.37 | 0.058 |
| West | 7.79 | 0.48–126.27 | 0.15 |
| Higher USMLE step 1 examination score | 1.01 | 0.93–1.09 | 0.87 |
| AOA status | |||
| Inducted | Reference | ||
| Not inducted | 0.50 | 0.07–3.37 | 0.47 |
| School does not have a chapter | 0.21 | 0.02–2.00 | 0.18 |
| Medical school ranking | |||
| Top 40 medical school | Reference | ||
| Other medical school | 0.98 | 0.17–5.53 | 0.98 |
| Dedicated research time* | |||
| No research year | Reference | ||
| One dedicated research year | 0.04 | 0.003–0.60 | 0.02* |
| Reported importance of cost saving | |||
| “Extremely” or “very” important | Reference | ||
| “Somewhat” or “not at all” important | 17.13 | 2.94–99.91 | 0.002* |
African American race and more than one dedicated research year were excluded from the model due to insufficient sample size for analysis.
DO, Doctor of Osteopathic Medicine; IMG, International Medical Graduate; RRR, Relative Risk Ratio.
Future Directions for the PSCA: Qualitative Results
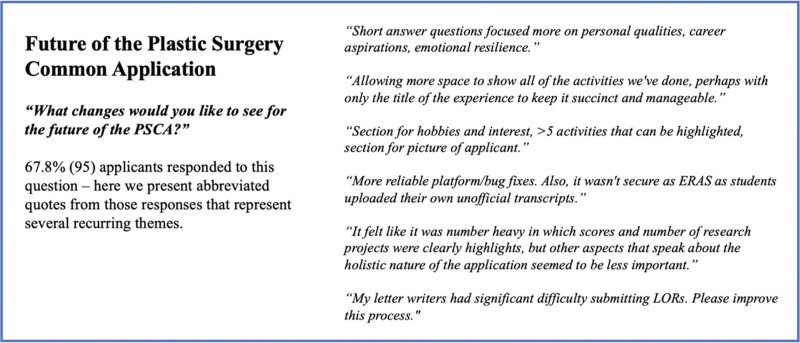
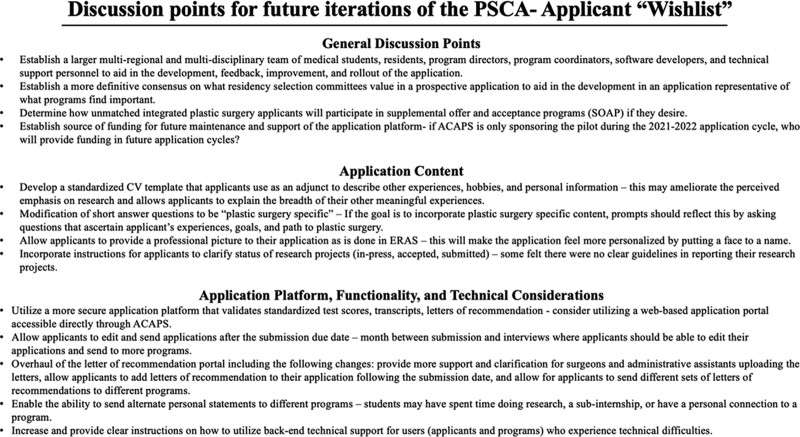
Applicants were asked three short-answer questions to capture their thoughts on future directions of the PSCA. The first of these questions was “What changes would you like to see for the future of the PSCA?,” which was answered by 67.8% (95) of respondents. This question yielded a wide range of responses with multiple recurring themes. These themes represented general and specific recommendations for the PSCA, ranging from ideal application content, reliable survey tool infrastructure and support, letter of recommendation functionality, and potential supplemental features. Figure 8 contains selected responses that represent overarching qualitative themes for this question.
Fig. 8.
Applicant recommendations for future of PSCA.
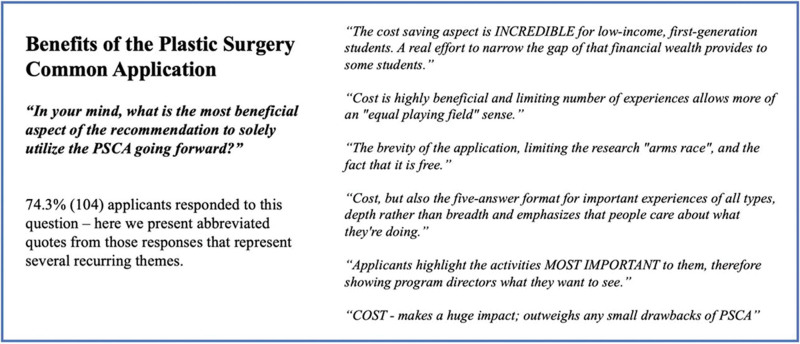
The second free response question asked was “In your mind, what is the most beneficial aspect of the ACAPS recommendation to solely utilize the PSCA going forward?” which was answered by 74.3% (104) of respondents. The overwhelming majority of applicants who responded, 86.5% (90), mentioned the cost savings associated with the PSCA as a benefit for future use (Fig. 9).
Fig. 9.
Applicant reported benefits of the PSCA.
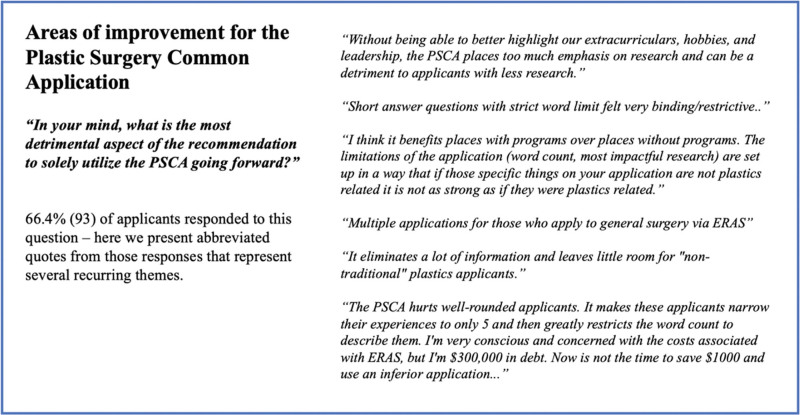
The third free-response question asked the applicants “In your mind, what is the most detrimental aspect of the ACAPS recommendation to solely utilize the PSCA going forward?” This question was answered by 66.4% (93) of respondents. The responses to this question were heterogeneous and included several themes that centered around limitations imposed by the PSCA including experience and word limits, which makes it hard for applicants to highlight their breadth of experiences and personal background (Fig. 10).
Fig. 10.
Applicant reported areas of improvement for the PSCA.
DISCUSSION
History and Development of the PSCA
During the 2020–2021 application cycle, the first version of the PSCA was piloted by 20 integrated plastic surgery residency programs. This version of the PSCA was reportedly met with positive feedback and led to the development of a second version of the PSCA, which incorporated several modifications based on feedback from applicants and programs. In the spring of 2021, ACAPS recommended all integrated plastic surgery residency programs to utilize the second version PSCA for the 2021–2022 application cycle with the plan to replace ERAS for the 2022–2023 cycle.4 While multiple specialties have expressed interest in alternative application processes outside of ERAS, the PSCA places the field of plastic surgery in a unique position as the only specialty to utilize a non-ERAS, specialty-wide application that is free to applicants. In an effort to evaluate the utility of this application, we performed a survey of integrated plastic surgery applicants during the 2021–2022 application cycle.
We respectfully commend and thank the PSCA team for their efforts and dedication to providing integrated plastic surgery applicants with a cost-effective residency application that aims to improve the ability of applicants to showcase their noteworthy experiences. This novel and innovative endeavor will lead to continued collaboration and efforts to establish an effective, reliable, and affordable application for future plastic surgeons.
Importance of the Residency Application and Goals of the PSCA
Identification and selection of residents who will be successful trainees and future leaders in plastic surgery are vital to the specialty. Therefore, training institutions must select those applicants who demonstrate superb leadership skills, personal accountability, and an unwavering sense of dedication to the specialty. The first step in doing so is providing applicants with the opportunity to showcase these characteristics with a comprehensive, reliable, and equitable application process.
To best understand and contextualize applicant’s perspectives as it relates to the PSCA, it is important to highlight the goals and anticipated benefits of this application. The overall goals of the PSCA are to provide a more relevant plastic surgery-specific application while reducing the financial costs to applicants and minimizing the administrative burden for program directors.5 Since the inception of ERAS, residency applicants have been subjected to a “one-size-fits-all” template, which is ubiquitous among all specialties. To this end, ERAS may not capture specific elements that are important for individual specialties like plastic surgery.
Comparing the PSCA and ERAS
Overall, the majority (63%) of applicants who responded to this survey would prefer applying with the PSCA alone. This finding is in contrast to the 41% of applicants who believed that ERAS better highlighted the strengths of their application when compared with the 27% who reported that the PSCA best highlighted their strengths. Therefore, despite a 14% increase in the percentage of applicants who believe the ERAS highlights strengths better, most (63%) still prefer to apply with the PSCA. This paradox may be partly due to the relative tradeoffs of the two applications, whereby the importance of cost may take precedence over marginal differences in the ability to showcase certain strengths. Additionally, this contradiction may be representative of applicant’s predilection toward the potential of the PSCA as future iterations continue to undergo refinement and address concerns raised by applicants from the initial cohorts.
Most applicants (70%) felt that the short answer prompts of the PSCA added meaningful information that would otherwise not be captured through ERAS. Cost was by far the most commonly cited benefit of the PSCA, with 85% of respondents mentioning cost savings in reference to the perceived benefits of permanently transitioning to the PSCA in 2022–2023. Despite this finding, previous research has demonstrated that applicants may not place as much importance on the overall cost of the application process, including interviews that may incur costs up to $10,000 during the application cycle.7
Interestingly, those who performed a dedicated research year during or after medical school were significantly more likely to prefer the PSCA (Table 3). This finding corroborates what many applicants mentioned in the free response texts in that the ability to upload a bibliography of research publications and presentations without a similar option for highlighting other experiences may unfairly favor those who performed research years. This will be important in future years as previously used objective metrics, such as USMLE test scores, clerkship grades, and AOA, continue to become less common, leaving students with fewer opportunities to differentiate themselves.
Challenges Regarding the PSCA
Despite the overall preference toward the PSCA, many respondents had concerns regarding its infrastructure, content, and future. Some of the most commonly cited concerns stemmed from limitations in reporting breadth of experiences, technical issues with features of the application, a lack of user support, and a perceived emphasis on research compared with other experiences. Many respondents found that they were unable to highlight their experiences well with the PSCA due to inherent limitations of the application itself. Applicants believed that the PSCA should not strictly limit reporting of experiences, and that they should have the opportunity to detail the breadth of their efforts and time commitments, as these experiences likely required extensive energy and dedication.
In addition to the concerns over the application’s content, the current iteration of the PSCA lacks the ability to verify licensing examination scores, transcripts, and other application materials. In contrast, ERAS utilizes an interconnected process linking individual dean’s offices and National Board of Medical Examiners test scores to student’s applications, thus providing confidential and verified information.8 Of note, the Central Application Service of the SF Match system (utilized by independent plastic surgery residency programs) allows applicants to upload unofficial transcripts and licensing examination scores.9
A final concern pertains to applicants who do not successfully match into an integrated plastic surgery residency program. Despite the majority of the applicants attaching extreme or very high importance to the cost-saving aspects, it is possible that applicants may complete ERAS as a safeguard to participate in the Supplemental Offer an Acceptance Program (SOAP) for open residency positions in other specialties as well as those who plan to dual apply into other specialties. The SOAP process utilizes the ERAS application; therefore, applicants who wish to have an opportunity to apply for programs in other specialties during this process will have to complete ERAS before finding out whether they matched to participate. Additionally, given the increasing level of competition to match into an integrated plastic surgery residency, some applicants may choose to dual apply into other specialties to increase their odds of matching into a position. Both of these instances may represent situations that would benefit from further troubleshooting to eliminate the need for applicants to also complete the ERAS application.
Applicant Feedback and Future Directions
There are several major takeaways from this study. Most notably, integrated plastic surgery applicants prefer a more affordable application process. Second, applicants want the opportunity to demonstrate their hard work and dedication to a myriad of different experiences with less limitations. Finally, there are still several concerns regarding the technical infrastructure, validity, and content of the PSCA. To this end, we discuss several themes that were voiced by applicants for the future of the application and the process of applying for integrated plastic surgery residency (Fig. 11). Included in this discussion is the development of a standardized CV that applicants may use as an adjunct to describe their experiences, similar to the research portion of the application. (See appendix, Supplemental Digital Content 2, which displays example CV template for PSCA, http://links.lww.com/PRSGO/C349.) Applicant reported future directions included the incorporation of more plastic surgery-specific short answer questions related to plastic surgery and goals in the field, modifications to the letter of recommendation and personal statement system, and a myriad of technical recommendations that will allow for a more user-friendly experience while ensuring a process of verification with ample back-end support. We believe addressing these commonly voiced concerns will be critical for the future efforts of the process of applying into plastic surgery residency.
Fig. 11.
Discussion points for future iterations of the PSCA-applicant “wishlist.”
Strengths and Limitations
There are several shortcomings of this study. Notably, the timing that the survey was issued may bias the results insofar as the association with the first interview release date that was on December 11, 2021. The survey was administered during the week before and several weeks after the interview release date, which may have biased responses after this date to favor one application versus another based on an applicant’s interview yield.
Our study also has several important strengths to highlight. The metrics obtained by the cohort in our study accurately recapitulate those from previous years based on available National Ranking Matching Program data reports, and therefore, we believe that our cohort is consistent with the entire cohort of applicants during the 2021–2022 cycle. Additionally, data suggest that most plastic surgery applicants apply to most, if not all, available training programs, allowing us to distribute the survey to a wide range of applicants.
CONCLUSIONS
As we continue to push for equity in the process of applying to residency, we should continue to seek opportunities to minimize expenses for applicants while maximizing their ability to highlight their attributes through a secure and seamless application process. The majority of applicants in this study favored the PSCA, notably for its associated cost savings. With that, there were still concerns that may warrant the reconsideration of replacing ERAS with the PSCA in the 2022–2023 cycle. Ultimately, the PSCA represents a great step for specialties to have more control over their application and selection process as well as allowing for the implementation of specialty-specific information that may allow programs to find candidates that best fit their goals, mission, and culture.
Supplementary Material
Footnotes
Published online 13 January 2023.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.National Resident Matching Program. Charting outcomes in the match. Washington, D.C.: National Resident Matching Program; 2020:180–197. Available at https://mk0nrmp3oyqui6wqfm.kinstacdn.com/wp-content/uploads/2020/07/Charting-Outcomes-in-the-Match-2020_MD-Senior_final.pdf. Accessed November 9, 2021. [Google Scholar]
- 2.National Resident Matching Program, Data Release and Research Committee. Results of the 2021 NRMP Applicant Survey by Preferred Specialty and Applicant Type. Washington, D.C.: NRMP; 2021. [Google Scholar]
- 3.Carmody JB, Rosman IS, Carlson JC. Application fever: reviewing the causes, costs, and cures for residency application inflation. Cureus. 2021;13:e13804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weber R. Message from ACAPS president Robert Weber. Am Council Acad Plast Surg. Available at https://acaplasticsurgeons.org/president-message.cgi. Accessed November 10, 2021. [Google Scholar]
- 5.American Council of Academic Plastic Surgeons. Plastic surgery common application. Available at https://acaplasticsurgeons.org/PSCA/. Accessed November 10, 2021.
- 6.US News. Best Medical Schools (Research) ranked in 2022 —n.d. Available at https://www.usnews.com/best-graduate-schools/top-medical-schools/research-rankings. Accessed December 16, 2021.
- 7.Sarac BA, Rangwani SM, Schoenbrunner AR, et al. The cost of applying to integrated plastic surgery residency. Plast Reconstr Surg Global Open. 2021;9:e3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.AAMC. About eras. n.d. Available at https://students-residents.aamc.org/applying-residencies-eras/about-eras. Accessed January 11, 2022.
- 9.SF match. Residency and fellowship matching services. n.d. Available at https://www.sfmatch.org/. Accessed January 24, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.