Abstract
Objectives
During the pandemic, Switzerland avoided stringent lockdowns and provided funds to stabilize the economy. To assess whether and in what subgroups the pandemic impacted on depressive symptoms in this specific Swiss context, we derived depression trajectories over an extended pandemic period in a Swiss cohort and related them to individuals' sociodemographic characteristics.
Study design
This was a population-based cohort study.
Methods
The population-based COVCO-Basel cohort in North-Western Switzerland invited 112,848 adult residents of whom 12,724 participated at baseline. Between July 2020 and December 2021, 6396 participants answered to additional 18 monthly online questionnaires. Depression symptoms were repeatedly measured by the DASS-21 scale. Group-based Trajectory Models methods were applied to identify clusters of similar depression trajectories. Trajectory clusters were characterized descriptively and with a Multinomial response model.
Results
Three distinct trajectories were identified. The ‘Highly affected’ trajectory (13%) had a larger presence of younger and female participants with lower average income, higher levels of past depression, and living alone. A majority of individuals in the ‘Unaffected’ trajectory (52%) were of medium or high average income, older average age, without previous depression symptoms, and not living alone. The ‘Moderately affected’ trajectory (35%) had a composition intermediate between the two opposite ‘extreme’ trajectories.
Conclusions
This study is among few studies investigating depression trajectories up to the time when COVID-19 vaccination was readily available to the entire population. During these 18 months of the pandemic, depressive symptoms increased in a substantial percentage of participants. Economic support, high-quality health care system, and moderate containment measures did not sufficiently protect all population subgroups from adverse, potentially long-term psychological pandemic impacts.
Keywords: Mental health, COVID-19, Depression, Population-based, Cohort, Longitudinal, Trajectory clusters
Introduction
As health is a state of complete physical, mental and social well-being, efforts to prevent SARS-CoV-2 infections must be parallelled by measures to maintain mental health.1 , 2 Possible pathways from the pandemic to poor mental health include, but are not restricted to, fear of infection, a severe disease course, and vaccination; job loss and financial worries; work-life conflict; conflicts in family and social networks; social isolation; unhealthy or addictive behaviour; cultural and travel restrictions; a general loss of freedom; and feelings of uncertainty.3 , 4 Inadequate utilization of, and access to, mental health care may have contributed to the increasing symptoms burden. The COVID-19 pandemic not only challenged the capacity of infection-related care, but also mental health care, which is in any case often marginalized compared to other health service domains.1 , 5
According to a recent meta-analysis of 43 repeated cross-sectional and longitudinal studies covering the first year of the pandemic, mental health including depression symptoms worsened on average during the first two months of the pandemic and increased in a dose-dependent manner with the number of COVID-19 cases and deaths and with the stringency of governmental lockdown measures. Past the first two pandemic months, the heterogeneity of mental health symptom trajectories was very high,6 thereby questioning the meaning of overall trajectories reported in previous meta-analyses.7 , 8 Evidence on substantial differences in longer-term mental reactions to the pandemic and the numerous pathways potentially affecting mental health during the pandemic point to the need for context- and subgroup-specific evidence on symptom trajectories obtained from longitudinally assessed individuals.
Understanding individual differences in longer-term mental health reactions to pandemic situations is of policy relevance for more precise predictions on the pandemic contribution to the future mental health burden,8 and for future pandemic preparedness in targeting preventive interventions and in designing containment measures to protect the most susceptible groups from adverse mental health effects. It also supports clinicians in paying attention to patients at high risk for developing a clinically relevant mental disorder as a result of the pandemic.
Yet, the studies investigating the trajectories of mental health symptoms based on repeatedly interviewed participants in sufficiently sized adult general population studies are still limited and often cover the first pandemic months only.2 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16, 17, 18 These shorter-term trajectory studies inconsistently point to differences in mental health responses by age, sex, socio-economic status, or pre-existing mental and physical health conditions in the first phases of the pandemic. More recent longitudinal trajectory studies covering a period of at least one year after the start of the pandemic are evolving, covering different cultural contexts, and they confirm the existence of clusters of individuals with higher and lower mental health score trajectories (e.g. depression, anxiety, stress, post-traumatic stress disorder, or a combination thereof),19, 20, 21, 22, 23, 24 with scores seemingly worse during phases of lockdown, in young adults, in women, and in people with pre-existing physical and mental health conditions. Other factors associated with more severe mental health trajectories included social isolation, unhealthy lifestyles and sleep problems, lack of outdoor access, domestic violence, and financial problems.19, 20, 21, 22, 23, 24 Interestingly, in France where financial support was provided to affected occupational groups, financial difficulties were not associated with the level of mental health symptoms19
The aim of this study was, first, to identify clusters of similar depression trajectories over an extended period of the pandemic, and second, to relate these trajectories to individuals' sociodemographic characteristics. The study is based on longitudinal data from more than 10,000 randomly selected residents from North-Western Switzerland, an economically well-off country usually considered as a country with one of the worldwide most highly performing health care systems.25 The country was evaluated to handle the pandemic comparatively well, both from a health26 and from an economic (https://www.admin.ch/gov/en/start/documentation/media-releases.msg-id-86822.html) perspective, and avoided very stringent lockdowns.27
Methods
Study population
We analyzed the trajectories of the depression scores in the digital COVCO-Basel cohort implemented in July 2020 in North-Western Switzerland to investigate the long-term impact of the COVID-19 containment measures on broad health domains.28
Persons aged 18 years or older residing in Basel-Stadt or Basel-Landschaft for at least 5 years were eligible. Equally sized canton and age-stratified (18–49, 50–65, 65+ years) random samples of eligible individual residents were provided by the Federal Statistical Office. Study invitations were sent to the randomly sampled individuals in waves by surface mail. Of 112,848 people receiving an invitation, 12,724 participated at baseline and entered the study between July 2020 and April 2021. The COVCO-Basel study population is comparable to the total population in the two cantons in terms of publicly available sociodemographic factors including gender and marital status (see final COVCO-Basel report available in German only: https://www.swisstph.ch/fileadmin/user_upload/CoVCoBasel_Schlussbericht_20211028.pdf).
Women are overrepresented in the age group <65 years and underrepresented in the age group 65+ years. Foreign language–speaking residents are underrepresented as questionnaires were only provided in German in the absence of funds for multilingual translations.
Between July 2020 and December 2021, participants answered to a baseline and repeated monthly online questionnaires implemented in REDCap (Research Electronic Data Capture) data collection system (https://www.project-redcap.org/). The study period was divided into two-week periods (fortnights), and we included in the analysis 6396 participants with depression score recorded for at least eight fortnights, not necessarily in a row. Participants with segments of trajectories shorter than eight fortnights would excessively influence estimation of the parameters characterizing the clusters, since we fit polynomials of increasing degree to the observed trajectories (see below).
The study protocol was approved by the regional ethics committee (Ethikkommission Nordwest-und Zentralschweiz 2020-00927) and all participants provided informed consent before enrolment to the study.
Depressive symptom score
Depressive symptoms were measured using the Depressive Anxiety Stress Scale (DASS-21.)29
Each item (depression; anxiety; stress) is scored on a 0–3 scale: ‘never = 0, sometimes = 1, often = 2, and (almost) always = 3’. The score for each domain is calculated by summing up the scores for the corresponding seven items and multiplying the total by 2. The score can be divided, to aid interpretation, into the following categories (normal = 0–9, mild = 10–13, moderate = 14–20, severe = 21–27, and extremely severe = 28+) for each domain. But the present study a priori focused on the original quantitative discrete depression score, rather than on categories, as endpoint, with a possible score range from 0 to 42.
Descriptive characteristics of trajectories
Age in years and sex were self-reported. Non-binary sex was excluded because of its small sample size. Self-reported household income was classified into three categories: below 6000, 6000–15,000, and 15,000+ CHF/month (1 CHF is equivalent to approximately 1.05 US$). Education was classified into six levels: no school degree, compulsory school, vocational training, high school diploma, technical college/University of Applied Sciences, University (including Polytechnical University). Canton of residence distinguished Basel-Stadt (urban) and Basel-Landschaft (periurban/rural). Living status was dichotomised into ‘Alone’ vs ‘Not alone’.
Participants were asked to retrospectively report past depressive symptoms according to DASS-21 scale for the month of the baseline assessment in the year before the pandemic.
For sensitivity analysis, time of study entry was defined as the period of completing the baseline questionnaire, categorised as follows: July–Sep 2020; Oct–Dec 2020; Jan–April 2021.
Statistical analysis
In the first step, we applied Group-based Trajectory Models (GBTM) methods to identify clusters of similar trajectories. The approach by Nielsen et al. (2014)30 estimates by maximum likelihood a finite mixture model where each individual belongs to a cluster with an unknown probability (to be estimated), and the response in each class is assumed to be distributed as a Zero-inflated Poisson with expected value varying polynomially with time. A Zero-inflated Poisson distribution is appropriate for the depression score, which has a discrete domain, ranging from 0 to 42, and a positively skewed distribution characterized by an excess of zeroes (see Supplementary Fig. S1). Although other approaches are present in the literature for this purpose, in particular models in the wide class of Structural Equation Models (like the Latent Growth Mixed Models – LGMM), we preferred the GBTM approach mainly for two reasons: i) GBTMs are somewhat more ‘exploratory’ than LGMMs, as they just ‘agnostically’ identify groups of similar trajectories in the population, leaving to further analyses the task to characterise such classes (see below, the description of the second step of analysis); ii) GBTMs are more flexible in the choice of the response distribution, and therefore more appropriate for our choice of assuming a Zero-inflated Poisson distribution for the depression score. For a non-technical comparison of the two approaches, see Frankfurt et al.31
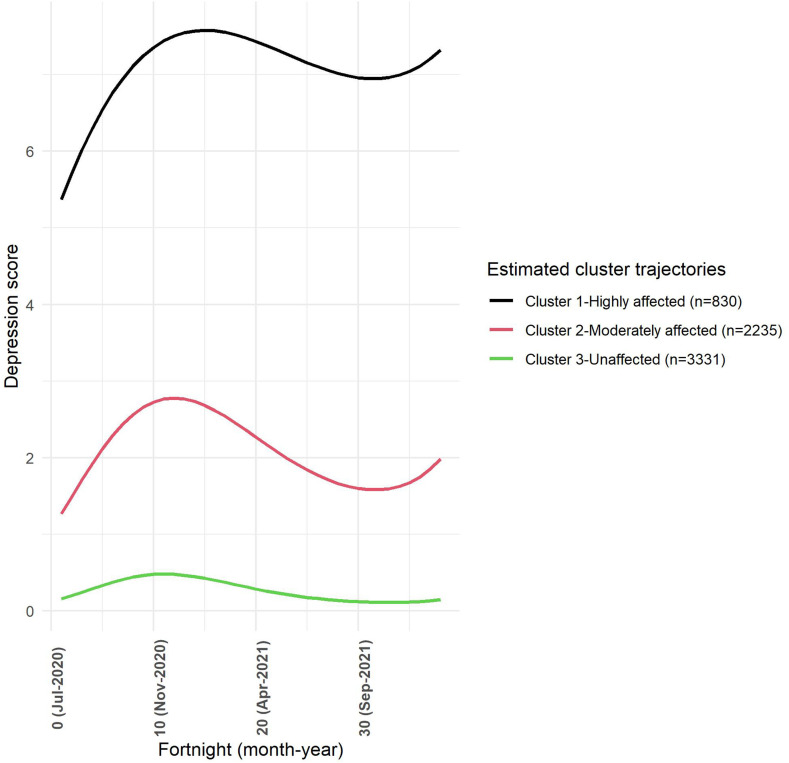
After obtaining the clusters of similar trajectories, we estimated the average trajectories for each cluster and plotted them in Fig. 1 .
Fig. 1.
Estimated trajectories of depression symptom scores for the three clusters (n = 6396, number of clusters k = 3, polynomial degree P = 3).
In the second step, we characterised the clusters both in descriptive and model-based terms. The descriptive analysis is a simple graphical representation of the distribution of selected characteristics (specifically: age, gender, income, canton, education, living status, past depression) in the clusters of similar trajectories. The modelling approach consisted in treating cluster membership as a categorical polytomous response variable, specifying a multinomial response model and testing the statistical significance of the same characteristics used in the descriptive phase, as independent predictors of the cluster membership.
All statistical analyses were conducted using R 4.0.32 The GBTM analysis used the code made available by Paul Schneider at the URL: https://raw.githubusercontent.com/bitowaqr/traj/master/raw_code.R. Multinomial logit models have been fitted using the library VGAM. The plots have been produced using the library ggplot2.
Results
Study population characteristics are summarized in Table 1 . The sample has an overrepresentation of females. Participants are well educated with 32% having a University degree. The mean prevalence of moderate to severe depressive symptoms one year before entry into the study was 8.18% (age group 18–49 years), 3.47% (age group 50–65 years) and 2.31% (age group 65+ years). Participants answering to at least eight occasions did not differ from excluded participants.
Table 1.
Baseline characteristicsa of COVCO-Basel participants, comparing participants included vs not-included in the current analysis.
| Participants included (≥8 occasions) | Participants excluded (<8 occasions) | ||
|---|---|---|---|
| N | 6396 | 6328 | |
| Age [Years] | 57.66 (14.17) | 55.4 (15.3) | |
| Sex | Female | 3561 (55.68) | 3430 (54.2) |
| Male | 2835 (44.32) | 2898 (45.8) | |
| Household income | <6000 CHF/month | 1842 (28.80) | 1830 (28.91) |
| 6000-15000 CHF/month | 3610 (56.44) | 3414 (53.95) | |
| 15,000+ CHF/month | 745 (11.65) | 804 (12.70) | |
| NA | 199 (3.11) | 280 (4.43) | |
| Canton | Basel-Stadt | 3137 (49.05) | 3160 (49.90) |
| Basel-Landschaft | 3259 (50.95) | 3168 (50.10) | |
| Education | No school degree | 4 (0.06) | 6 (0.10) |
| Compulsory school | 140 (2.19) | 175 (2.77) | |
| Vocational training | 2234 (34.93) | 2058 (32.52) | |
| High school | 383 (5.99) | 402 (6.36) | |
| Technical college/University of Applied Sciences | 1565 (24.47) | 1537 (24.28) | |
| University (including Polytechnic) | 2060 (32.21) | 2076 (32.80) | |
| NA | 10 (0.15) | 74 (1.17) | |
| Living status | Alone | 1362 (21.29) | 1316 (20.79) |
| Not alone | 4994 (78.08) | 4910 (77.60) | |
| NA | 40 (0.63) | 102 (1.61) | |
| Past depression (score 0–42) | 2.62 (5.14) | 2.66 (5.05) | |
Data presented as mean (standard deviation) or count (percentage).
Finding clusters of similar trajectories using GBTM
Based on computational stability, the degree of the polynomials used to estimate the average trajectories in the clusters has been fixed at P = 3 (i.e. cubic polynomials) and the number of clusters has been fixed at k = 3, using AIC and BIC as criteria. k = 4 clusters were slightly superior in terms of AIC and BIC, but posed problems in terms of convergence. Moreover, the four clusters obtained were not as well separated as the three clusters chosen for this paper: in particular, groups 3 and 4 differ on average only by about 1 point of depression score. This difference does not appear to be relevant in public health terms, and this led us to prefer the classification into 3 clusters over 4, notwithstanding the small gain in AIC and BIC. The ‘typical’ (average) trajectories of the three clusters of similar trajectories are graphically represented in Fig. 1. Cluster 1 (‘Highly affected’), with an estimated prevalence of 13%, starts already at a higher average level of depression score, and follows markedly the waves the COVID-19 pandemic. Mental health, in terms of depression score, of members of this cluster is strongly influenced by the pandemic and stays elevated by December 2021 compared to the baseline depression score. On the contrary, Cluster 3 (‘Unaffected’), with an estimated prevalence of 52%, starts at very low levels of depression and has a typical trajectory over time that is hardly influenced by the waves of the COVID-19 pandemic. Finally, Cluster 2 (‘Moderately affected'), with an estimated prevalence of 35%, has an intermediate pattern, similar to Cluster 1, but with attenuated effects of the waves of the COVID-19 pandemic.
Exploratory analysis
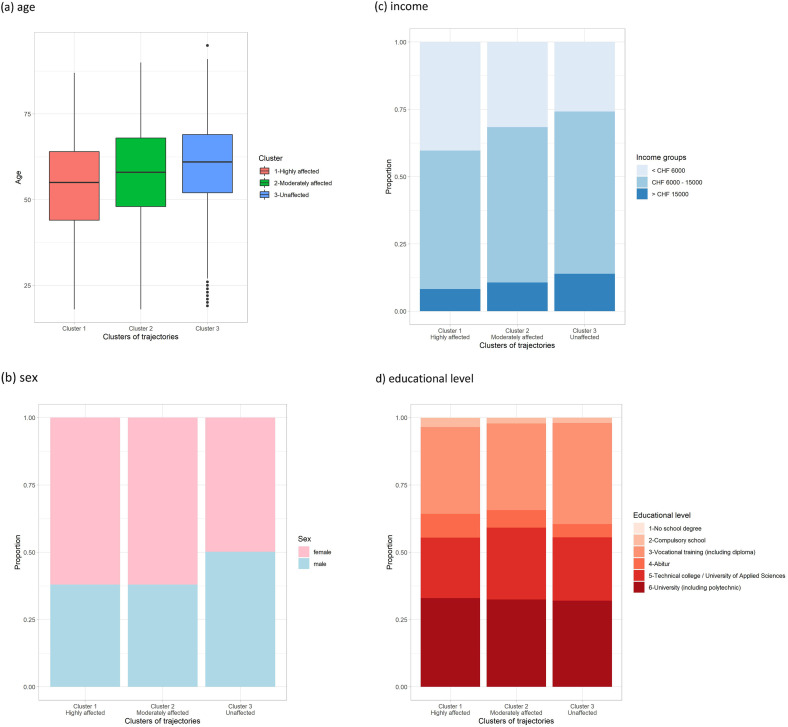
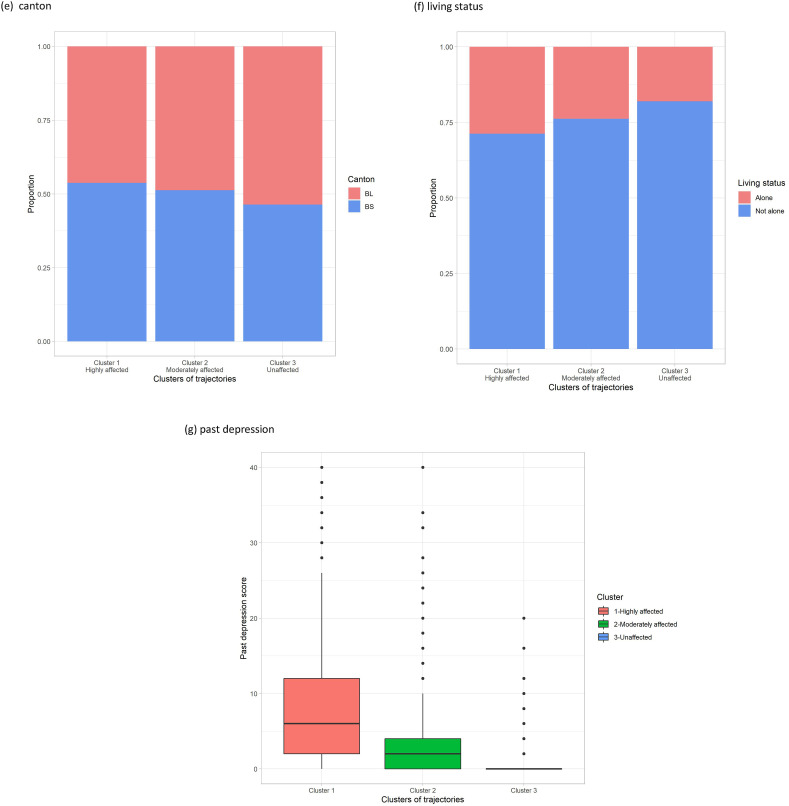
Fig. 2 graphically displays the distribution of selected characteristics in the three clusters: (a) age, (b) sex, (c) income, (d) educational level, (e) canton, (f) living status, and (g) past depression. Visual inspection of Fig. 2(a–g) suggests that age, sex, income, living status, and past depression may play a role in explaining membership in the three clusters, and therefore different trajectories in mean depression. In Cluster 1 (the ‘Highly affected’), there is a relatively larger presence, compared to the other two clusters, of participants who are younger, female, with lower average income, living alone, with higher levels of past depression. On the contrary, in Cluster 3 (the ‘Unaffected’), there is a majority of individuals with medium or older average age, high average income, not living along, with no previous symptoms of depression, while sex seems to be balanced in this Cluster. Cluster 2 has a composition intermediate between the two opposite ‘extreme’ Clusters 1 and 3. Cantonal residency (urban vs periurban/rural setting) and educational level did not seem to play a significant role in characterizing the three clusters.
Fig. 2.
Distribution of selected characteristics according to the three clusters of trajectories.
Model-based analysis
A selection procedure, starting from the full multinomial logit model with all covariates additively included and carried out using both AIC and BIC, has provided the following final model:
where: π1 = Pr{belonging to Cluster 1}, π2 = Pr{belonging to Cluster 2}, π3 = Pr{belonging to Cluster 3}; Sex2 = Male; Income2 = CHF 6000 – 15,000; Income3 = >CHF 15000; LivingStatus2 = Not alone.
The estimated regression coefficients, their standard deviations and P-value of the Wald test statistics for testing their significance are summarized in Table 2 . The most statistically significant determinants of cluster membership were age, sex, the highest category of income and the score on past depression. Living status appears to have a significant effect only on the logit of belonging to Cluster 1 vs belonging to Cluster 3. Education level and canton were not statistically significant predictors and were thus excluded from the final model.
Table 2.
Independent association of covariatesa with depression trajectories according to the multinomial logit model.
| S.Dev. | P-value | S.Dev. | P-value | ||||
|---|---|---|---|---|---|---|---|
| Intercept | −1.539 | 0.302 | 0.000 | −0.083 | 0.207 | 0.689 | |
| Age | −0.010 | 0.004 | 0.023 | −0.009 | 0.003 | 0.002 | |
| Sex | Male | −0.355 | 0.129 | 0.006 | −0.476 | 0.083 | 0.000 |
| Income | CHF 6000 – 15,000 | −0.137 | 0.135 | 0.311 | 0.022 | 0.091 | 0.813 |
| >CHF 15,000 | −0.639 | 0.240 | 0.008 | −0.338 | 0.142 | 0.018 | |
| Living status | Not alone | −0.256 | 0.150 | 0.088 | −0.120 | 0.104 | 0.246 |
| Past depression score | 1.082 | 0.048 | 0.000 | 0.791 | 0.044 | 0.000 |
Education and Canton were not maintained in the model.
In Table 3 , we report the predicted probability of cluster membership for three hypothetical individuals.
Table 3.
Predicted probability of cluster membership for three hypothetical individuals.
| Name | Age | Sex | Income | Living status | Past depres. score | Prob (Cluster1) | Prob (Cluster2) | Prob (Cluster3) |
|---|---|---|---|---|---|---|---|---|
| Petra | 25 | Female | < CHF 6000 | Alone | 11 | 0.848 | 0.152 | 0.000 |
| Ursula | 60 | Female | CHF 6000–15,000 | Not alone | 3 | 0.247 | 0.631 | 0.121 |
| Martin | 70 | Male | > CHF 15,000 | Not alone | 0 | 0.025 | 0.157 | 0.817 |
Petra is a young woman, aged 25 years, living alone, having an income in the lowest class (< CHF 6000 per month) and with a previous history of moderate depression symptoms. She has a very high probability of belonging to Cluster ‘Highly affected’. Ursula is also a woman, but older than Petra (aged 60 years), living with her family, having an income in the intermediate class (CHF 6000–15,000 per month) and with only slight symptoms of depression in the past. The most probable cluster for Ursula is Cluster ‘Moderately affected’, although the probability of falling into Cluster ‘Highly affected’ is not negligible (0.247). Martin is a man, aged 70 years, living with his family, with an income in the highest class (>CHF 15,000) and no symptoms of depression in the past. By far the most probable cluster for Martin is Cluster ‘Unaffected’.
Sensitivity analysis
Participants entered the study at different dates (from July 2020 up to April 2021) and hence at different phases of the COVID-19 pandemic. Supplement Fig. S2 displays the distribution of month of entry in the three clusters. The distribution is highly balanced. Furthermore, the distribution of the number of occasions answered did not differ by cluster (Supplementary Fig. S3).
Discussion
This is one of only few studies investigating depression trajectories in a large adult community sample over an extended period, up to the time when COVID-19 vaccination was readily available to the population. Depressive symptoms increased in a substantial percentage of this North-Western Switzerland study population, albeit at a rather low, and clinically not yet relevant, average depression score level, and mental health trajectories were similar to other regions in Europe and elsewhere.19, 20, 21, 22, 23, 24
Compared to other European countries, Switzerland imposed less stringent containment measures.33 Jobs and enterprises were protected and subsidized to avoid economic hardship. But like others, the country experienced substantial excess mortality, particularly during the second epidemic wave.34 In-hospital mortality among COVID-19 patients decreased between February 2020 and March 2021, but deteriorated when national intensive care unit occupancy reached about 70%, suggesting that even in a high-quality health care system operational pressures develop before triage becomes necessary.35 In the first pandemic year, a survey among youth mental health professionals reported a large increase in treatment demand and waiting time and a worrisome overload of mental health services.9 , 36
The study was implemented after the most extreme lockdown spanning from March 2020 to June 2020 in Switzerland. The increase in depressive symptoms in the affected trajectories coincides with the second epidemic wave resulting in restrictions between October 2020 and April 2021, and the emergence of the Omicron Sars-Cov-2 variant and associated restrictions towards the end of 2021. COVID-19 vaccine was provided to susceptible persons from December 2020 and made readily available to all population subgroups from Spring 2021 on.
Few studies identified longitudinal trajectories in an exploratory fashion. Two early longitudinal studies in the UK investigated psychological distress trajectories in community samples with a latent class approach.9 , 17 In the period between April and May 2021, general health questionnaire (GHQ-12) derived psychological distress was higher than prepandemic. Trajectories also included at the one extreme end a subgroup of people whose likelihood of distress remained continuously close to zero up to May 2021 (53.2% of study participants) and at the other extreme two-fifths of all participants who experienced a severe elevation of distress throughout the observation period.9 Another analysis of the same study population, but focusing on depressive symptoms, also found three latent trajectories similar to ours and to the psychological distress trajectories, including low (60%), moderate (29%) and severe (11%) depressive symptoms during the lockdown.18 Longer-term trajectory studies confirmed the presence of clusters of mental health trajectories with different response levels to the pandemic.19, 20, 21, 22, 23, 24 Few quasi-experimental studies benefitted from the effect of the pandemic and associated lockdowns on mental health. For example, a quasi-experimental study in Australia demonstrated that mental health was slightly worse in the region affected by a lockdown.37
The observed characteristics of persons at risk of exhibiting mental health symptoms also closely follow results from shorter- and longer-term studies abroad,19, 20, 21, 22, 23, 24 , 38 although the findings are not entirely consistent.7 But many, including longer-term studies, parallel early observations from UK exploratory trajectory approach studies, where the risk of belonging to a trajectory affected by psychological distress was greater for those who were younger, female, living without a partner, those who lost income or were living in poor neighbourhoods, and those who were reporting a previous mental illness. In addition, individuals with COVID-19–related symptoms and pre-existing at-risk health conditions for a severe COVID-19 course seemed more affected.7 , 9 , 17 Trajectories and characteristics similar to ours were also observed in a smaller Argentinian community sample with less frequent questionnaires but covering the period from April 2020 to August 2021.10 In the COVCO-Basel cohort, we observed a strong correlation between greenspace and life satisfaction that was restricted to persons with high income pointing to the complex role of the environment on psychological well-being during the pandemic.28
The population sub-groups exhibiting a continuously high level of mental distress during times of the pandemic are of concern. First, extended periods of elevated depression symptoms harbour a longer-term risk for developing mental illness.39 Second, elevated depression is often associated with changes in sleeping and eating habits, themselves posing a risk for physical and mental disorders.38 , 39 Third, depression and psychological distress are linked to altered immune system functioning and cardiovascular disease risk, both affecting infection susceptibility.40 Fourth, differences in life expectancy of up to four years according to neighbourhood SES level were previously reported in Basel, the urban centre of North-Western Switzerland, and the pandemic may widen this gap.41
The strengths of the present study are the population-based sampling, the comparatively large sample size, that symptoms of depression were assessed on a monthly basis with a validated tool until months after the broad availability of an efficient COVID-19 vaccine, and that neither date of study entry nor extent of monthly participation confounded the results. Study limitations include, first, the low participation rate in the COVCO-Basel study. Second, the lack of generalizability of the results to all residents in the greater Basel region, as foreign language–speaking residents were underrepresented in the study sample. In the absence of a multilingual non-responder questionnaire, the present study cannot be evaluated for representativeness. In particular, the prevalence of the observed trajectories cannot be estimated for the general population. It is possible that additional trajectories exist in non-participants. Third, prepandemic depression levels were assessed retrospectively. If participants with high depression levels during the pandemic were more likely to overestimate prepandemic depression, the influence of prepandemic depression symptoms may be overestimated. Fourth, as in any cohort, attrition bias is of concern.
Conclusions
The results point out that a high level of economic support and a high-quality health care system in the light of moderate containment measures as applied in Switzerland do not sufficiently protect the entire population to the same extent from adverse psychological impacts of a pandemic. Ignoring adverse effects of a long-lasting pandemic on mental well-being may have negative repercussions in the life trajectories of specific vulnerable subgroups as well as potentially on the infection control. Poor mental health and associated unhealthy behaviours may well be the most important long-term sequelae of the pandemic.
Author statements
Acknowledgements
We like to thank Thomas Vermes, Ekin Tertemiz and Emmanuel Schaffner for their contribution to the data management of the digital cohort. We thank the research staff and field workers for the coordination of data collection: Melissa Witzig, Alexia Schmitt, Tamara Wirth, Susanna Nussbaumer, Cornelia Devonas, Maria Vitale, Cynthia Vecchio-Lopez, Astrid Siegfried, Thea Wülser, Kristina Hoffmann, Julia Bähler, Luisa Waschkowski, Katrina Obas, Nadia Hedrich and Nicolas Moesli. We thank the Swiss Federal Statistical Office for providing the randomized list of participants for the main population-based portion of our study. We thank the Corona Immunitas program and SSPH+ for the collaboration. Study data were collected and managed using REDCap electronic data capture tools hosted at the Swiss Tropical and Public Health Institute.
Ethical approval
The study protocol was approved by the regional ethics committee (Ethikkommission Nordwest-und Zentralschweiz 2020-00927) and all participants provided informed consent before enrolment to the study
Funding
COVCO-Basel was funded by the Health Departments of Basel-Stadt and Basel-Landschaft and by the funding sources of the Corona Immunitas program (https://www.corona-immunitas.ch/en/).
Competing interests
The authors declare no conflict of interest. The funders had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
Author contributions
Nicole Probst-Hensch: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Project administration, Funding acquisition. Ayoung Jeong: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Dirk Keidel: Investigation, Data curation, Writing – review & editing, Project administration. Medea Imboden: Investigation, Writing – review & editing, Project administration. Gianfranco Lovison: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2023.01.010.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N., et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatr. 2020;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatr. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leung C.M.C., Ho M.K., Bharwani A.A., Cogo-Moreira H., Wang Y., Chow M.S.C., et al. Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis. Transl Psychiatry. 2022;12(1):205. doi: 10.1038/s41398-022-01946-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pfefferbaum B., North C.S. Mental health and the covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 5.Kane H., Gourret Baumgart J., El-Hage W., Deloyer J., Maes C., Lebas M.C., et al. Opportunities and challenges for professionals in psychiatry and mental health care using digital technologies during the COVID-19 pandemic: systematic review. JMIR Hum Factors. 2022;9(1) doi: 10.2196/30359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salanti G., Peter N., Tonia T., Holloway A., White I.R., Darwish L., et al. The impact of the COVID-19 pandemic and associated control measures on the mental health of the general population: a systematic review and dose-response meta-analysis. Ann Intern Med. 2022;175(11):1560–1571. doi: 10.7326/M22-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ellwardt L., Präg P. Heterogeneous mental health development during the COVID-19 pandemic in the United Kingdom. Sci Rep. 2021;11(1) doi: 10.1038/s41598-021-95490-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernández R.S., Crivelli L., Guimet N.M., Allegri R.F., Picco S., Pedreira M.E. Psychological distress and mental health trajectories during the COVID-19 pandemic in Argentina: a longitudinal study. Sci Rep. 2022;12(1):5632. doi: 10.1038/s41598-022-09663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landi G., Pakenham K.I., Crocetti E., Tossani E., Grandi S. The trajectories of anxiety and depression during the COVID-19 pandemic and the protective role of psychological flexibility: a four-wave longitudinal study. J Affect Disord. 2022;307:69–78. doi: 10.1016/j.jad.2022.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bendau A., Kunas S.L., Wyka S., Petzold M.B., Plag J., Asselmann E., et al. Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: the role of pre-existing anxiety, depressive, and other mental disorders. J Anxiety Disord. 2021;79 doi: 10.1016/j.janxdis.2021.102377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riehm K.E., Holingue C., Smail E.J., Kapteyn A., Bennett D., Thrul J., et al. Trajectories of mental distress among U.S. adults during the COVID-19 pandemic. Ann Behav Med. 2021;55(2):93–102. doi: 10.1093/abm/kaaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saunders R., Buckman J.E.J., Fonagy P., Fancourt D. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol Med. 2021:1–9. doi: 10.1017/S0033291721000957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mooldijk S.S., Dommershuijsen L.J., de Feijter M., Luik A.I. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. 2022;149:274–280. doi: 10.1016/j.jpsychires.2022.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Batterham P.J., Calear A.L., McCallum S.M., Morse A.R., Banfield M., Farrer L.M., et al. Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Med J Aust. 2021;214(10):462–468. doi: 10.5694/mja2.51043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pierce M., McManus S., Hope H., Hotopf M., Ford T., Hatch S.L., et al. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatr. 2021;8(7):610–619. doi: 10.1016/S2215-0366(21)00151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iob E., Frank P., Steptoe A., Fancourt D. Levels of severity of depressive symptoms among at-risk groups in the UK during the COVID-19 pandemic. JAMA Netw Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.26064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moulin F., Jean F., Melchior M., Patanè M., Pinucci I., Sijbrandij M., et al. Longitudinal impact of the COVID19 pandemic on mental health in a general population sample in France: evidence from the COMET Study. J Affect Disord. 2023;320:275–283. doi: 10.1016/j.jad.2022.09.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thorpe W.J.R., Gutman L.M. The trajectory of mental health problems for UK emerging adults during COVID-19. J Psychiatr Res. 2022;156:491–497. doi: 10.1016/j.jpsychires.2022.10.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayerl H., Stolz E., Freidl W. Trajectories of loneliness, depressive symptoms, and anxiety symptoms during the COVID-19 pandemic in Austria. Publ Health. 2022;212:10–13. doi: 10.1016/j.puhe.2022.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosa L., Godwin H.J., Cortese S., Brandt V. Predictors of longer-term depression trajectories during the COVID-19 pandemic: a longitudinal study in four UK cohorts. Evid Based Ment Health. 2022;25(4):e3. doi: 10.1136/ebmental-2022-300461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oka T., Kubo T., Kobayashi N., Nakai F., Miyake Y., Hamamura T., et al. Multiple time measurements of multidimensional psychiatric states from immediately before the COVID-19 pandemic to one year later: a longitudinal online survey of the Japanese population. Transl Psychiatry. 2021;11(1):573. doi: 10.1038/s41398-021-01696-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu Z.A., Shi L., Que J.Y., Zheng Y.B., Wang Q.W., Liu W.J., et al. Long-term psychological profile of general population following COVID-19 outbreak: symptom trajectories and evolution of psychopathological network. Epidemiol Psychiatr Sci. 2022;31:e69. doi: 10.1017/S2045796022000518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.OECD . OECD; 2018. Health at a glance: Europe. [Google Scholar]
- 26.Jamison D.T., Lau L.J., Wu K.B., Xiong Y. Country performance against COVID-19: rankings for 35 countries. BMJ Glob Health. 2020;5(12) doi: 10.1136/bmjgh-2020-003047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tavakkoli M., Karim A., Fischer F.B., Monzon Llamas L., Raoofi A., Zafar S., et al. From public health policy to impact for COVID-19: a multi-country case study in Switzerland, Spain, Iran and Pakistan. Int J Publ Health. 2022;67 doi: 10.3389/ijph.2022.1604969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jeong A., Galliker F., Imboden M., Keidel D., de Hoogh K., Vienneau D., et al. Residential exposure to greenspace and life satisfaction in times of COVID-19: a cross-sectional analysis of 9444 participants from a population-based study in Basel-Stadt and Basel-Landschaft. Swiss Med Wkly. 2022;152:w30204. doi: 10.4414/smw.2022.w30204. [DOI] [PubMed] [Google Scholar]
- 29.Lovibond S.H., Lovibond P.F. Psychology Foundation of Australia; 1996. Manual for the depression anxiety stress scales. [Google Scholar]
- 30.Nielsen Jdr J.S., Sun Y., Day D.M., Bevc I., Duchesne T. T. Group-based criminal trajectory analysis using cross-validation criteria. Comm Stat Theory Meth. 2014;43:4337–4356. [Google Scholar]
- 31.Frankfurt S., Frazier P., Syed M., Jung K.R. Using group-based trajectory and growth mixture modeling to identify classes of change trajectories. Counsel Psychol. 2016;44(5):622–660. [Google Scholar]
- 32.Team RC. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. 2020.
- 33.Pleninger R., Streicher S., Sturm J.E. Do COVID-19 containment measures work? Evidence from Switzerland. Swiss J Econ Stat. 2022;158(1):5. doi: 10.1186/s41937-022-00083-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Staub K., Panczak R., Matthes K.L., Floris J., Berlin C., Junker C., et al. Historically high excess mortality during the COVID-19 pandemic in Switzerland, Sweden, and Spain. Ann Intern Med. 2022;175(4):523–532. doi: 10.7326/M21-3824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anderegg N., Panczak R., Egger M., Low N., Riou J. Survival among people hospitalized with COVID-19 in Switzerland: a nationwide population-based analysis. BMC Med. 2022;20(1):164. doi: 10.1186/s12916-022-02364-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Werling A.M., Walitza S., Eliez S., Drechsler R. The impact of the COVID-19 pandemic on mental health care of children and adolescents in Switzerland: results of a survey among mental health care professionals after one year of COVID-19. Int J Environ Res Public Health. 2022;19(6) doi: 10.3390/ijerph19063252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Butterworth P., Schurer S., Trinh T.A., Vera-Toscano E., Wooden M. Effect of lockdown on mental health in Australia: evidence from a natural experiment analysing a longitudinal probability sample survey. Lancet Public Health. 2022;7(5):e427–e436. doi: 10.1016/S2468-2667(22)00082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bonati M., Campi R., Segre G. Psychological impact of the quarantine during the COVID-19 pandemic on the general European adult population: a systematic review of the evidence. Epidemiol Psychiatr Sci. 2022;31:e27. doi: 10.1017/S2045796022000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Essau C.A., de la Torre-Luque A., Lewinsohn P.M., Rohde P. Patterns, predictors, and outcome of the trajectories of depressive symptoms from adolescence to adulthood. Depress Anxiety. 2020;37(6):565–575. doi: 10.1002/da.23034. [DOI] [PubMed] [Google Scholar]
- 40.Masafi S., Saadat S.H., Tehranchi K., Olya R., Heidari M., Malihialzackerini S., et al. Effect of stress, depression and type D personality on immune system in the incidence of coronary artery disease. Open Access Maced J Med Sci. 2018;6(8):1533–1544. doi: 10.3889/oamjms.2018.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moser A., Panczak R., Zwahlen M., Clough-Gorr K.M., Spoerri A., Stuck A.E., et al. What does your neighbourhood say about you? A study of life expectancy in 1.3 million Swiss neighbourhoods. J Epidemiol Community Health. 2014;68(12):1125–1132. doi: 10.1136/jech-2014-204352. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.