Abstract
Context
The number of pediatric anterior cruciate ligament reconstructions (ACLRs) occurring yearly increased almost 6-fold from 2004–2014. We find it interesting that limited recent data exist on rates of ACL injury and reconstruction in children and adolescents, especially in the context of COVID-19.
Objective
Given the effect of the COVID-19 pandemic on youth sports seasons and the postponement of many elective surgeries, we sought to examine the changes in rates of ACLR during this period.
Design
Retrospective cohort study.
Setting
This study used the Pediatric Health Information System (PHIS) database to identify eligible patients at PHIS-participating hospitals nationwide from January 2016–June 2021, with March 1, 2020, considered the start of the COVID-19 pandemic.
Patients or Other Participants
Using Current Procedural Terminology codes, patients 18 years old and younger who underwent ACLR surgery were identified.
Main Outcome Measure(s)
Patient demographics and overall rates of surgery prepandemic and intrapandemic were compared. Data were analyzed using bivariate, mixed-model, and time series analyses.
Results
A total of 24 843 ACLRs were identified during this time period. In total, 1853 fewer surgeries than expected were performed after March 2020 given prepandemic trends. Intrapandemic demographics revealed an increase in the proportion of patients who identified as White and with private insurance and a decrease in the proportion who identified as Black and with public insurance. Also, the proportion of ACLRs by region shifted, with more surgeries performed in the Midwest and fewer in the Northeast. In the model adjusted for hospital-level variability, only race and insurance status remained significant.
Conclusions
Based on prepandemic trends, fewer patients than projected underwent ACLR once the pandemic began, likely due to a combination of decreased rates of injury and delayed surgery.
Keywords: anterior cruciate ligament injury, pandemic effects, pediatric sports medicine
Key Points
Pediatric patients undergoing anterior cruciate ligament reconstructions increased from 2016–2020.
Fewer than expected reconstructions were performed during the COVID-19 pandemic, with a shift in the patient demographics.
Anterior cruciate ligament (ACL) ruptures are relatively common athletic injuries among pediatric and adolescent patients. Previous researchers1 have suggested that rates of ACL reconstruction (ACLR) are increasing among this population. The number of pediatric and adolescent ACLRs increased almost 6-fold from 2004–2014.1 This increase occurred across sex and age groups and was more rapid than the overall increase of orthopaedic surgeries in this population.1
Since the onset of the pandemic in March 2020, the number of sports injuries has decreased significantly.2–5 The proportion of injuries attributed to sports fell during COVID-19, largely due to modified or canceled sport seasons.6 Regarding ACL injuries specifically, a Google Trends analysis showed that from March 2020–May 2020, the terms ACL reconstruction, ACL repair, and anterior cruciate ligament reconstruction were searched less often than before the start of the pandemic, demonstrating changing interest in this surgery among the general population.7
Aside from its effect on athletic injuries, COVID-19 also resulted in postponed or canceled elective surgeries in many locations.8,9 This may have presented problems for patients who experienced an ACL rupture but were unable to undergo surgery in a timely fashion. Whereas surgery should be delayed until the effusion reduces and range of motion of the knee returns, delaying ACLR further is associated with a higher rate of chondral injuries and increased severity of these lesions.10,11
Given the aforementioned changes brought about by COVID-19, we suspected that the rates of ACLR have decreased substantially since the pandemic began in the United States, around March 2020, with a rise in incidence when many athletes returned to play. To date, no formal studies have examined how ACLR rates in the pediatric and adolescent patient population have been affected by the COVID-19 pandemic. In this study, we aimed to answer the following questions: (1) What was the general trend of ACLR among pediatric patients in the United States from January 2016–June 2021? (2) How did the COVID-19 pandemic affect this trend? (3) What demographic differences were observed between the patient population undergoing ACLR before and during the COVID-19 pandemic?
METHODS
Data Source
Data for this study were obtained from the Pediatric Health Information System (PHIS), an administrative database that contains inpatient, emergency department, ambulatory surgery, and observation encounter-level data from more than 50 not-for-profit tertiary care pediatric hospitals in the United States. These hospitals are affiliated with the Children's Hospital Association (Lenexa, Kansas). Data quality and reliability were ensured through a joint effort between the Children's Hospital Association and participating hospitals. For the purposes of external benchmarking, participating hospitals provided discharge and encounter data, including demographics, diagnoses, and procedures. Nearly all of these hospitals also submitted resource utilization data (eg, pharmaceuticals, imaging, and laboratory) to PHIS. Data were deidentified at the time of submission and subjected to a number of reliability and validity checks before being included in the database. For this study, data from 48 hospitals were included.
Population and Selection Criteria
This retrospective cohort study used data from the PHIS database from January 1, 2016–June 30, 2021, to identify patients aged 18 years old or younger who had undergone ACLR at PHIS-participating hospitals. Patients were identified using Current Procedural Terminology (CPT) codes (https://www.cms.gov/Medicare/Fraud-and-Abuse/PhysicianSelfReferral). Isolated ACLR was captured by CPT 29888 (arthroscopically aided anterior cruciate ligament repair/augmentation or reconstruction) and CPT 27407 (repair, revision, and/or reconstruction procedures on the femur [thigh region] and knee joint). Combined ACL and collateral ligament reconstruction codes were included using CPT 27409, 27427, 27428, and 27429. Combined ACLR and tibial spine fracture codes were included using CPT 29850 and 29851. The search methods were based on those of Tepolt et al.1 We imposed no further exclusion criteria for this study, and no patients were excluded from the identified cohort.
Variables
Patients were classified as having their surgeries prepandemic, defined as January 2016–February 2020, or intrapandemic, March 2020–June 2021. March 2020 was chosen as the start of the intrapandemic period because it reflects the month the World Health Organization declared SARS-CoV-2, the virus that causes COVID-19, a pandemic.12 Given that the pandemic was ongoing throughout March 2020–June 2021, we used the term intrapandemic to describe this period. Demographic variables collected were sex, median household income, age at surgery, race (White, Pacific Islander or Native Hawaiian, Black, Asian, American Indian or Alaskan Native), insurance provider (private, public, uninsured, other), urban or suburban versus rural (determined using the patient's zip code and US census tracts), and region (Midwest, Northeast, South, West).
Statistical Analysis
Data were analyzed with bivariate analysis, mixed-effects logistic regression using variables significant in the bivariate analysis, and time series analysis. Descriptive analysis was used to characterize the patient population by demographic factors and hospital region. Bivariate analysis (t tests and χ2 tests, as indicated) and mixed-model analysis adjusted by hospital-level variability compared prepandemic and intrapandemic trends. The PHIS database is an aggregate of data from 48 hospitals; therefore, hospital-level variability was included as a covariate in this model to control for differences attributable to hospital-level factors rather than patient-level variables. We used random-effects modeling to determine the change in ACLRs due to COVID-19 while controlling for month of the year. An interrupted time series analysis was performed with prepandemic and intrapandemic linear trend estimates. The prepandemic ACLR trend was used to estimate the difference between the expected number of surgeries based on prepandemic trends and the number performed in the intrapandemic period. A P value < .05 was considered significant. The prepandemic and intrapandemic research was completed using Stata (version 17.0; Stata Corp).
RESULTS
We identified 24 843 patients from 48 hospitals who had undergone ACLR from January 2016–June 2021. Their mean age was 14.89 years (95% CI = 10.39, 19.37 years), and 12 757 (51.35%) of the patients were female. Most patients had private insurance (n = 13 636, 54.89%) and identified as White (n = 15 140, 60.94%). Of the surgeries, 5517 (22.21%) were completed in the Midwest, 5045 (20.31%) in the Northeast, 8157 (32.83%) in the South, and 6124 (24.65%) in the West.
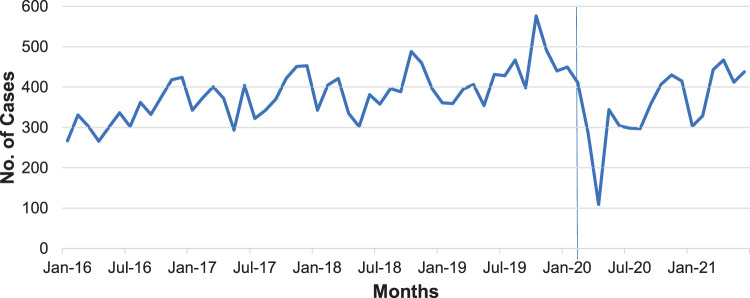
During the prepandemic period, a general trend of increased ACLRs was noted, with a significant drop in March 2020. After this initial drop, the number of ACLRs began to increase again beginning in May 2020. Before the COVID-19 pandemic, ACLRs were trending up by about 3 surgeries per month (95% CI = 1.79, 3.64; P < .01). In March 2020, 203 (41.5%) fewer ACLRs were performed than would have been expected based on this prepandemic trend (95% CI = −283.17, −122.95; P < .01). After this initial drop, the number of ACLRs increased by 13 surgeries per month (95% CI = 6.31, 20.94; P < .01). In total, 1853 fewer surgeries were performed during the intrapandemic time period than expected given prepandemic trends (Figure). After controlling for the month of surgery, the number of ACLRs overall decreased 30% from the prepandemic to the intrapandemic time periods, likely attributable to COVID-19 (incidence rate ratio = 0.700, 95% CI = 0.607, 0.808; P < .01).
Figure.
Incidence of anterior cruciate ligament reconstructions in US pediatric hospitals, January 2016–June 2021. The vertical line at March 2020 represents the start of the intrapandemic period, the month the World Health Organization declared SARS-CoV-2 a pandemic.
In the bivariate analysis, age, race, payor, urban region, and urban home zip code were different between those undergoing ACLR in the prepandemic versus the intrapandemic period (Table 1). Since COVID-19, the proportion of patients who underwent ACLR who identified as White increased (59.4% to 66.2%, P < .01) and the proportion of patients who identified as Black decreased (18.5% to 16.6%, P < .01), with no changes in the proportion of patients identifying as Pacific Islander or Native Hawaiian, Asian, or American Indian or Alaskan Native. The proportion of patients with private insurance increased (53.9% to 58.3%, P < .01), and the proportion with public insurance decreased (37.8% to 34.1%, P < .01). We found that intrapandemic, the proportion of ACLRs performed in the Midwest increased (21.8% to 23.7%, P < .01) and the proportion performed in the Northeast decreased (20.7% to 18.9%, P < .01), as did those with an urban home zip code (87.7% to 85.3%, P < .01) versus prepandemic. After controlling for hospital-level variability using a mixed-model analysis, the only variables that were still significant were identifying as White (odds ratio = 1.26, 95% CI = 1.16, 1.37; P < .01) and insurance status (Table 2).
Table 1.
Patient Characteristics and Outcomes for Pediatric Patients Who Underwent Anterior Cruciate Ligament Reconstruction in US Pediatric Hospitals, January 2016–June 2021
| Characteristic |
Cases, No. (%)a |
P Value |
|
| Prepandemic (January 2016–February 2020) |
Intrapandemic (March 2020–June 2021) |
||
| Total | 19 202 (77.3) | 5641 (22.7) | |
| Sex | .05 | ||
| Male | 9406 (49.0) | 2680 (47.5) | |
| Female | 9796 (51.0) | 2961 (52.5) | |
| Income, $b | 49 462.70 ± 20 593.40 | 49 630.40 ± 20 448.60 | .59 |
| Age, mean ± SD, y | 14.9 ± 2.2 | 14.8 ± 2.3 | <.01c |
| Racec | |||
| White | 11 405 (59.39) | 3735 (66.21) | <.01c |
| Pacific Islander or Native Hawaiian | 95 (0.49) | 20 (0.35) | .17 |
| Black | 3559 (18.53) | 938 (16.63) | .01c |
| Asian | 478 (2.49) | 160 (2.84) | .15 |
| American Indian or Alaskan Native | 62 (0.32) | 25 (0.44) | .18 |
| Payor | <.01c | ||
| Private | 10 345 (53.9) | 3291 (58.3) | |
| Public | 7261 (37.8) | 1925 (34.1) | |
| Uninsured | 166 (0.9) | 69 (1.2) | |
| Other | 1237 (6.4) | 348 (6.2) | |
| Unknown | 193 (1.0) | 8 (0.1) | |
| Urban | 16 833 (87.7) | 4813 (85.3) | <.01c |
| Region | <.01c | ||
| Midwest | 4181 (21.8) | 1336 (23.7) | |
| Northeast | 3977 (20.7) | 1068 (18.9) | |
| South | 6330 (33.0) | 1827 (32.4) | |
| West | 4714 (24.6) | 1410 (25.0) | |
Unless otherwise indicated.
Percentages may add up to >100% because some participants identified with >1 race.
P value < .05 indicates significant difference.
Table 2.
Factors Associated With Anterior Cruciate Ligament Reconstruction Among Pediatric Patients, January 2016–June 2021: A Mixed-Model Analysis Adjusted for Hospital-Level Variability
| Characteristic |
Odds Ratio |
95% CI |
P Value |
| Age | 0.989 | 0.975, 1.002 | .11 |
| Race | |||
| White | 1.260 | 1.16, 1.37 | <.01b |
| Black | 1.034 | 0.929, 1.151 | .54 |
| Payor | |||
| Privatea | — | — | |
| Public | 0.921 | 0.857, 0.989 | .02b |
| Uninsured | 1.250 | 0.926, 1.686 | .14 |
| Other | 0.950 | 0.782, 1.054 | .21 |
| Urban | 0.951 | 0.860, 1.052 | .33 |
| Region | |||
| Midwesta | — | — | |
| Northeast | 0.547 | 0.257, 1.160 | .12 |
| South | 1.043 | 0.605, 1.791 | .88 |
| West | 0.774 | 0.421, 1.439 | .42 |
Reference group.
P < .05 indicates significant difference.
DISCUSSION
To our knowledge, this cohort study is among the first to characterize trends in ACLRs among pediatric patients in recent years and during the COVID-19 pandemic. During a 5.5-year period of data, we identified 24 843 ACLRs from 48 pediatric hospitals in the United States. We found an overall increase in the number of ACLRs performed in this population from January 2016–June 2021, with a significant drop in March 2020 and April 2020, followed by a subsequent increase.
From January 2016–February 2020 (prepandemic), ACLRs were clearly trending up, suggesting that previous trends of increasing rates of ACLRs continued.1 However, we are unable to ascertain the reasons behind these increases based on our data. Limited information exists about recent trends of ACL injury; therefore, it is difficult to determine whether these changes were due to an increased rate of injury or of reconstruction alone.
In March 2020, the number of ACLRs decreased from what would have been expected based on the prepandemic trend. Two simple explanations include decreased ACL injuries due to halted participation in sports or delayed ACLR surgery due to personal or hospital precautions. Notably, after April 2020, the rate increased more quickly than that seen in prepandemic months. Similar trends were evident in other surgeries—orthopaedic and overall—with an initial drop and subsequent increase.13,14 Data for analysis were available through June 2021, but as the pandemic continues, we expect the rate of ACLRs to stabilize to prepandemic levels or increase slightly due to pandemic-related deconditioning.
Whereas no data have been published to date on changes in the rates of ACL injury, one can presume that when sports seasons were canceled in March 2020, injuries sharply decreased. We believe injuries still occurred because COVID-19 precautions varied regionally, and some athletes continued to practice and play informally. Per Gupta et al,15 the rates of ACL injury were lower in practice versus competition; therefore, the decrease in scheduled competitions alone may have led to fewer injuries. Some studies16–18 have suggested that the rate of injuries increases at the beginning of a sport season. The deconditioning that can occur during an off-season may contribute to a high rate of preseason injuries.19 The same effect may have been seen as athletes returned to sports after COVID-19 restrictions were lifted; for example, 2 early reports20,21 of National Football League players indicated that an abrupt return to sport may have contributed to an increased rate of on-field injuries. Under quarantine regulations, we presume that many patients were deconditioned when they returned to play. Children and adolescents in particular may have been at increased risk of injury from COVID-19 restrictions due to the combination of deconditioning and changes in body habitus that occurred during their off-season.22 Although most sports had resumed in some capacity by the end of the study period, teams should put increased emphasis on preseason conditioning with both strength and flexibility training.22 Changes in body habitus due to growth spurts alone are known to affect proprioception, and researchers23,24 suggested that proprioceptive exercises may reduce the risk of sport-related injury. This is certainly important to keep in mind when coupled with likely deconditioning during the pandemic.
The decrease in surgeries seen, particularly in March 2020, may reflect canceled surgeries due to hospital precautions and to patients' fear of seeking medical care, rather than true changes in rates of ACL injury. The 2 dips we saw in the intrapandemic period occurred during July 2020 and January 2021, the 2 months in the intrapandemic study period that corresponded with a peak in US COVID-19 cases.25 Although this may have been due to normal variation, it is also possible that during these case peaks, surgeries were delayed or canceled to alleviate hospital burden. The decline in surgeries was not unique to ALCR; investigators26 showed a decrease in all elective orthopaedic surgeries during the COVID-19 pandemic due to hospital delays and elective surgery cancellations. According to Chang et al,26 those with a lower American Society of Anesthesiologists Physical Status score (a subjective measure of a patient's overall health)—such as most pediatric patients undergoing ACLR—were more likely to want surgery at the earliest available time than those with higher American Society of Anesthesiologists scores. In addition, patients planning for soft tissue knee surgeries, such as ACLR, were more likely to want surgery at the earliest opportunity than those planning for some other orthopaedic procedures, explaining the spike in ACLRs in May 2020.26
Understanding the extent to which the decrease in surgical volume was due to fewer injuries versus delayed surgery is important because ACLR delays were associated with worse outcomes.10,11 It is customary to schedule ACLR within 3 months of injury due to the potential negative effects associated with delaying surgery, such as increased chondral lesions and elevated risks of meniscal injuries and irreparable meniscal tears,10,11 yet such scheduling became more difficult as many elective surgeries were delayed or canceled because of the COVID-19 pandemic.8,9 As providers counsel patients about the preferred surgical timing for ACLR, both during the COVID-19 pandemic and beyond, they must consider the negative effects of delayed ACLR. Future authors should quantify the rate of ACL rupture during the COVID-19 pandemic and the effects of delayed surgery during this period.
The demographics of the prepandemic patient population differed from those of the intrapandemic population. We found that after March 2020, the proportions of patients with private insurance and those who identified as White increased and the proportions of patients with public insurance and those who identified as Black decreased. Insurance status and identifying as White were significant even after we adjusted for hospital-level variability. The exact reason(s) for these differences are not clear, but similar trends with insurance were seen in another study27 quantifying the effect of the COVID-19 pandemic on elective surgeries from March 2020–August 2020. Lin et al27 observed that factors associated with decreased likelihood of a requested procedure being scheduled included being uninsured or self-pay. One plausible reason is that patients with private insurance may have had fewer barriers to surgery. Given that we demonstrated no difference in income between the patient populations prepandemic and intrapandemic, the difference in insurance status does not appear to be attributable to socioeconomic status alone. With a high rate of job loss or job turnover during the pandemic, many of the effects of insurance seen here could have been due to an overall change in insurance patterns in the US population.
In addition to insurance status, the proportion of surgeries performed in the Midwest increased, and those performed in the Northeast and among patients from urban areas decreased. This may in part have been the result of hospital-level variability, given that the region and living in an urban area were not significant after we adjusted for these variables. In addition, these findings may reflect differences in injury rates due to the variability of sports restrictions. For example, sports restrictions more universally affected school teams than private club and travel teams. Both of the latter have higher associated costs and thus may be composed of athletes from higher socioeconomic backgrounds. It is also possible that the numbers of these teams differ across the United States, which may explain the regional differences. Future researchers should quantify trends of ACL injury during this period to determine whether the demographic differences affected the rate of injury as well. This will allow us to better understand whether the changes in rates of ACLR during the COVID-19 pandemic were due to a change in rate of injury or disparities in care.
This study had the limitations inherent in all database and retrospective studies, which would apply to both the prepandemic and intrapandemic data. The average age of the patients undergoing ACLR was about 15 years. Whereas a large portion of the patients were adolescents, we likely did not fully capture all adolescent ACLRs because some skeletally mature adolescents undergo surgery in adult surgical facilities. A previous study28 showed that rates of ACL injury during childhood and adolescence peaked at age 16 years for girls and age 17 years for boys. Therefore, the true average age of pediatric patients undergoing ACLRs may be slightly older. Our study population may not have included a larger portion of ACLRs done among skeletally mature patients than among patients who were not yet skeletally mature. Adolescent girls have a higher rate of ACL injury than adolescent boys, but the reverse has been reported for individuals under 12 years old.29 No overall difference in adolescent boys and girls was evident in our study or in an earlier study1 of ACLRs from the same database during 2004–2014. This, too, may have been affected by the age distribution of our cohort, given that high school–aged females, who are often skeletally mature, had the highest rate of ACL injuries among children and adolescents 18 years old and younger.30
The PHIS database only analyzes data from large pediatric tertiary care referral hospitals; thus, our conclusions may not extend to hospitals treating different patient populations. Changes in trends may also be affected by differences in the proportion of ACLRs performed at pediatric tertiary care referral hospitals versus community and nonspecialty hospitals. Of note, these results only reflect ACLR trends, which may not translate to ACL injury trends in that they may reflect changes in treatment preferences or other unmeasured factors. The use of an administrative database provided a large sample size but inhibited our ability to establish causality for changes in trends.
Overall, we identified an increasing trend of pediatric patients who underwent ACLR from 2016–2021 but fewer than expected during the COVID-19 pandemic. Notably, the pandemic has had disparate effects on patients, depending on their race and insurance status. Whereas plausible explanations have been suggested, the true underlying causes could not be confirmed by the methods of our trends analysis study. These effects should be examined further in future studies to determine possible underlying causes and long-term trends.
REFERENCES
- 1.Tepolt FA, Feldman L, Kocher MS. Trends in pediatric ACL reconstruction from the PHIS database. J Pediatr Orthop . 2018;38(9):e490–e494. doi: 10.1097/BPO.0000000000001222. [DOI] [PubMed] [Google Scholar]
- 2.Sanford EL, Zagory J, Blackwell JM, Szmuk P, Ryan M, Ambardekar A. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J Pediatr Surg . 2021;56(5):918–922. doi: 10.1016/j.jpedsurg.2021.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baxter I, Hancock G, Clark M, et al. Paediatric orthopaedics in lockdown: a study on the effect of the SARS-Cov-2 pandemic on acute paediatric orthopaedics and trauma. Bone Jt Open . 2020;1(7):424–430. doi: 10.1302/2633-1462.17.BJO-2020-0086.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raitio A, Ahonen M, Jääskelä M, et al. Reduced number of pediatric orthopedic trauma requiring operative treatment during COVID-19 restrictions: a nationwide cohort study. Scand J Surg . 2021;110(2):254–257. doi: 10.1177/1457496920968014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bram JT, Johnson MA, Magee LC, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop . 2020;40(8):373–379. doi: 10.1097/BPO.0000000000001600. [DOI] [PubMed] [Google Scholar]
- 6.Chaudhari PP, Anderson M, Ourshalimian S, et al. Epidemiology of pediatric trauma during the coronavirus disease-2019 pandemic. J Pediatr Surg . 2022;57(2):284–290. doi: 10.1016/j.jpedsurg.2021.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tijerina JD, Cohen SA, Parham MJ, et al. Public interest in elective orthopedic surgery following recommendations during COVID-19: a Google Trends analysis. Cureus . 2020;12(12):e12123. doi: 10.7759/cureus.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Comfort SM, Murata Y, Pierpoint LA, Philippon MJ. Management of outpatient elective surgery for arthroplasty and sports medicine during the COVID-19 pandemic: a scoping review. Orthop J Sports Med . 2021;9(11):23259671211053335. doi: 10.1177/23259671211053335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pickens RC, Kao AM, Williams MA, Herman AC, Kneisl JS. Pediatric surgical reentry strategy following the COVID19 pandemic a tiered and balanced approach Am Surg Published online May 19. 2021. [DOI] [PMC free article] [PubMed]
- 10.Prodromidis AD, Drosatou C, Thivaios GC, Zreik N, Charalambous CP. Timing of anterior cruciate ligament reconstruction and relationship with meniscal tears: a systematic review and meta-analysis. Am J Sports Med . 2021;49(9):2551–2562. doi: 10.1177/0363546520964486. [DOI] [PubMed] [Google Scholar]
- 11.Prodromidis AD, Drosatou C, Mourikis A, Sutton PM, Charalambous CP. Relationship between timing of anterior cruciate ligament reconstruction and chondral injuries a systematic review and metaanalysis Am J Sports Med Published online September 15. 2021. [DOI] [PubMed]
- 12.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. World Health Organization Accessed April 21 2022. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 .
- 13.Salenger R, Etchill EW, Ad N, et al. The surge after the surge: cardiac surgery post-COVID-19. Ann Thorac Surg . 2020;110(6):2020–2025. doi: 10.1016/j.athoracsur.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uimonen M, Kuitunen I, Paloneva J, Launonen AP, Ponkilainen V, Mattila VM. The impact of the COVID-19 pandemic on waiting times for elective surgery patients: a multicenter study. PLoS One . 2021;16(7):e0253875. doi: 10.1371/journal.pone.0253875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta AS, Pierpoint LA, Comstock RD, Saper MG. Sex-based differences in anterior cruciate ligament injuries among United States high school soccer players: an epidemiological study. Orthop J Sports Med . 2020;8(5):2325967120919178. doi: 10.1177/2325967120919178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slater LV, Wasserman EB, Hart JM. Trends in recurrent anterior cruciate ligament injuries differ from new anterior cruciate ligament injuries in college and high school sports: 2009–2010 through 2016–2017. Orthop J Sports Med . 2019;7(11):2325967119883867. doi: 10.1177/2325967119883867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mouton C, Gokeler A, Urhausen A, Nührenbörger C, Seil R. High incidence of anterior cruciate ligament injuries within the first 2 months of the season in amateur team ball sports. Sports Health . 2021;14(2):183–187. doi: 10.1177/19417381211014140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palmieri-Smith RM, Mack CD, Brophy RH, et al. Epidemiology of anterior cruciate ligament tears in the National Football League. Am J Sports Med . 2021;49(7):1786–1793. doi: 10.1177/03635465211010146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heidt RS, II, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med . 2000;28(5):659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 20.Baker HP, Pirkle S, Cahill M, Reddy M, Portney D, Athiviraham A. The injury rate in National Football League players increased following cancellation of preseason games because of COVID-19. Arthrosc Sports Med Rehabil . 2021;3(4):e1147–e1154. doi: 10.1016/j.asmr.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patetta M, Mayo B, Martini OZ, Sullivan B, Onsen L, Hutchinson M. Preseason elimination impact on anterior cruciate ligament injury in the National Football League. World J Orthop . 2021;12(11):833–841. doi: 10.5312/wjo.v12.i11.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang C, Vander Voort W, Haus BM, Carter CW. COVID-19 and youth sports: what are the risks of getting back on the field too quickly? Pediatr Ann . 2021;50(11):e465–e469. doi: 10.3928/19382359-20211019-01. [DOI] [PubMed] [Google Scholar]
- 23.Martel M, Finos L, Koun E, Farnè A, Roy AC. The long developmental trajectory of body representation plasticity following tool use. Sci Rep . 2021;11(1):559. doi: 10.1038/s41598-020-79476-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riva D, Bianchi R, Rocca F, Mamo C. Proprioceptive training and injury prevention in a professional men's basketball team: a six-year prospective study. J Strength Cond Res . 2016;30(2):461–475. doi: 10.1519/JSC.0000000000001097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coronavirus in the US latest map and case count. New York Times . March 3. Accessed April 21 2022. 2020. https://www.nytimes.com/interactive/2021/us/covid-cases.html .
- 26.Chang J, Wignadasan W, Kontoghiorghe C, et al. Restarting elective orthopaedic services during the COVID-19 pandemic: do patients want to have surgery? Bone Jt Open . 2020;1(6):267–271. doi: 10.1302/2046-3758.16.BJO-2020-0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin JA, Braun HJ, Schwab ME, Pierce L, Sosa JA, Wick EC. Pandemic recovery persistent disparities in access to elective surgical procedures Ann Surg Published online March 3. 2021. [DOI] [PMC free article] [PubMed]
- 28.Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics . 2017;139(3):e20161877. doi: 10.1542/peds.2016-1877. [DOI] [PubMed] [Google Scholar]
- 29.Bloom DA, Wolfert AJ, Michalowitz A, Jazrawi LM, Carter CW. ACL injuries aren't just for girls: the role of age in predicting pediatric ACL injury. Sports Health . 2020;12(6):559–563. doi: 10.1177/1941738120935429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med . 2016;44(6):1502–1507. doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]