Figure 2. The immune response to ischemic stroke in the aged brain.
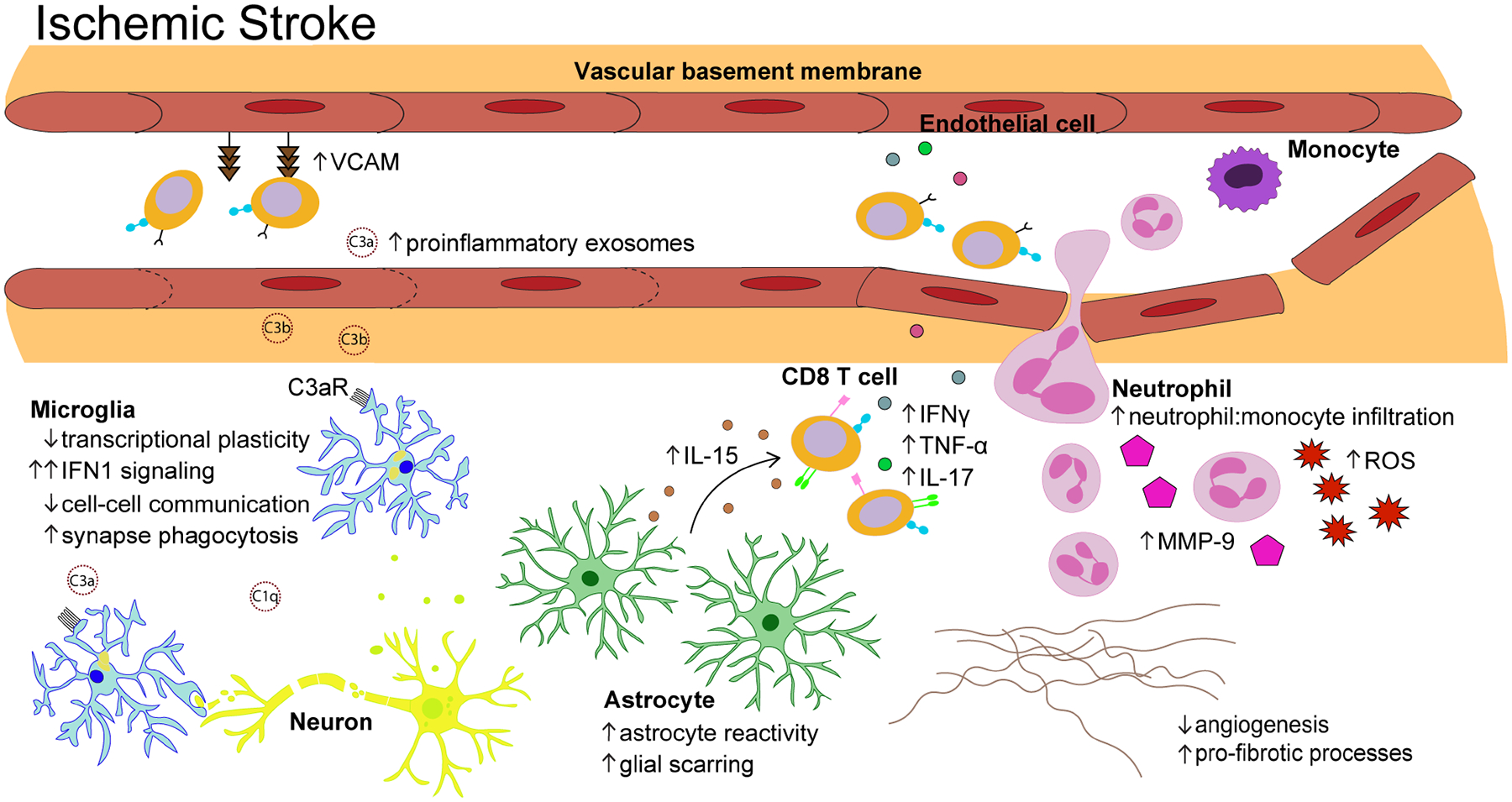
Following ischemic stroke, aged microglia (light blue) demonstrate a blunted transcriptional response dominated by genes associated with IFN1 signaling. The complement components that infiltrate the brain from serum exosomes bind to C3a receptors on aged microglia and trigger excessive synapse phagocytosis. Astrocyte reactivity (green) is exacerbated after ischemic stroke, leading to accelerated glial scar formation. Ischemic injury triggers aged astrocytes to significantly upregulate IL-15 which promotes further accumulation of CD8+ T cells (orange) that recruit other peripheral immune cells through secretion of proinflammatory cytokines. The ratio of neutrophils (pink) to monocytes (purple) is significantly increased in the aged brain after ischemic stroke and infiltrating neutrophils are highly metabolically active, secreting large amounts of matrix metalloproteinase (MMP)-9 and reactive oxygen species (ROS). Genes related to angiogenesis and extracellular matrix (ECM) remodeling (e.g. Col3a1, Col6a1, Pdgfrb, Lox, Angptl4, Ecm, Mmp12, Eln) are significantly downregulated in the aged brain relative to that observed in young animals, indicative of reduced vascular remodeling.
