Abstract
Primary yolk sac tumors are extragonadal germ cell tumors commonly seen in children and young adults. They are more common in men. Germ cells tumor on histopathological characteristics is classified as seminoma and non-seminomatous (NSGC). The rarest form of NSGC is an extragonadal yolk sac tumor of mediastinum. Clinical presentations are not specific and may imitate other chronic disease such as other malignancies or tuberculosis such as chest discomfort, vena cava superior syndrome, fever, weight loss, and chronic cough. Immunohistochemistry showed a positive result in Alpha-fetoprotein and pan-cytokeratin. Due to its rarity, brain metastases' clinical signs and symptoms, anatomical sites, and characteristics are less well documented. However, the metastatic brain process gave similar histological findings to the primary site. Additional radiological and laboratory tests can be carried out to identify other metastatic processes. Standardized treatment of primary mediastinal sac tumors with brain metastasis has not yet been established. Combining chemotherapy, surgery and radiation treatment could improve overall outcomes and prognosis. We present a scarce case of primary mediastinal yolk sac tumor with metastatic brain process in a 32-year-old male with a short survival period.
Keywords: Brain metastases, Extragonadal tumor, Non-seminomatous germ cell tumor, Yolk sac tumor
Introduction
Yolk Sac Tumor (YST) is an extragonadal non-seminomatous germ cell tumor (NSGCT) [1]. There was an incidence of 500 cases of NSGCT each year in the United States [2]. International Germ Cell Cancer Collaborative Group notes that the brain metastatic process accounts for 1.3% before chemotherapy [3]. It has a bimodal age distribution, with children being the most prevalent and 20-30-year-olds being the second most prevalent age group and predominantly male [4]. Brain metastatic process from primary mediastinal yolk sac tumor was scarce with poor prognosis. Our study presents a case of a young adult male with brain metastases developed from primary mediastinal yolk sac tumors with 9-month survival after platinum-based chemotherapy.
Case report
A 32-year-old man was referred from the primary healthcare hospital with progressive pulmonary tuberculosis on oral anti-tuberculosis medication 3 months before admission and superior vena cava syndrome. Tuberculosis in the previous clinic was diagnosed with clinical symptoms of chronic cough and weight loss, with chest x-ray showing pleural effusion and AFB negative. After 3 months of OAT, the patient did not improve but getting severe. Hence, He was referred to the higher health care system.
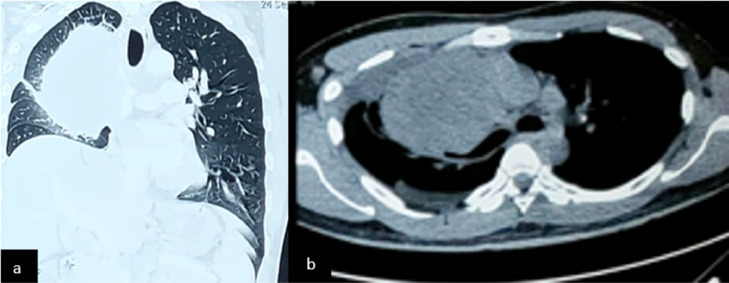
He presented with chronic cough, dyspnea, upper extremity swelling, distended neck vein, and 8 kg weight loss. After a general examination and imaging with a thorax CT scan, we found a solid mass on the middle anterior mediastinum (Fig. 1). Mediastinal mass biopsy result in mediastinal yolk sac tumor. Immunohistochemistry results were positive in PanCK and AFP. The blood test showed an increase in AFP. The patient received platinum-based chemotherapy with PEB (cisplatin, etoposide, and bleomycin) for 3 cycles and bleomycin for 6 cycles for 6 months. During the treatment, the patient clinical sign and symptoms improved.
Fig. 1.
The thorax CT scan obtained on the first admission showed a solid mass in the middle anterior mediastinum with the size of 7.65 × 8.28 × 11.3 cm.
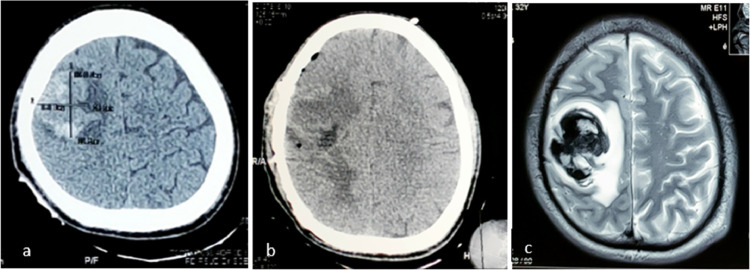
In the 7-month treatment, the patient got a chronic progressive headache, burning sensation and progressive left body weakness but did not get medical attention. The following week, the patient got loss of consciousness following the third attack of the left focal to bilateral tonic-clonic seizure attack and was admitted to the emergency room. His vital sign was stable A Glasgow Coma Scale (GCS) of 15 was obtained on examination after diazepam and phenytoin injections. Neurological deficits were supranuclear lingual and facial palsy, left body weakness, and left body paresthesia. An emergency non-contrast computed tomography (NCCT) scan revealed 27 ccs of intracerebral bleeding in the left parietal cortex (Fig. 2). We consulted the neurosurgery and internal medicine department. The intratumoral hemorrhage was decided to be evacuated and biopsied. After surgery, there was no progression in the neurological symptom.
Fig. 2.
Brain CT scan before (a) and after (b) intracerebral hemorrhage evacuation from the 7 months after initial treatment. Intracerebral hemorrhage volume was ±27 cc with midline shift <0.5 cm; after surgery, there was a hypodense area which indicates peritumoral edema. (c) Brain MRI with contrast before evacuation showed intratumoral hemorrhage.
Brain magnetic resonance imaging (MRI) with contrast and spectroscopy revealed a solid mass with peritumoral hemorrhage in the left parietal lobe destruction of the right frontal-occipital tract. Spectroscopy showed an increase in the choline/creatinine ratio in intra and peritumoral lesions. Other screenings such as contrast CT thorax, testicular and abdominal USG showed negative for tumor existence. Laboratory values showed slight hypoalbuminemia 2.9 g/dL and hypokalemia 2.9 mmol/L. There was a normal β-hCG level. Alpha-fetoprotein (AFP) was elevated and significantly reduced after brain surgery.
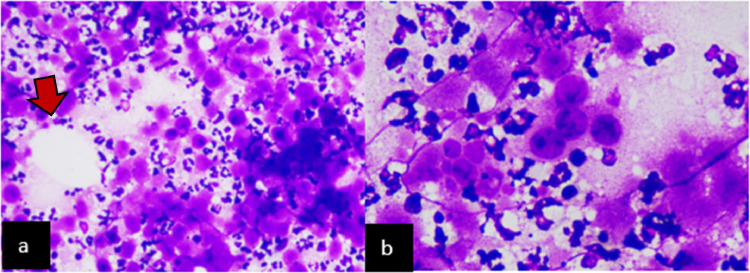
The brain biopsy was consistent with a NSGCT of the yolk sac type (Fig. 3). Immunohistochemistry in both specimens showed positive expression of AFP, pan-cytokeratin (PanCK) and negative expression of CD30. This result was consistent with a mediastinal yolk sac tumor. The patient was given levetiracetam as an antiepileptic medication. Dexamethasone was given 15 mg per day and tapered off weekly. Upon discharge, his GCS was 15 without any further neurological deficit progression. The patient died after 9 months after the first time he was diagnosed with the primary mediastinal tumor.
Fig. 3.
Histological specimen from the brain tissue (a) H&E stain 200x insert and (b) H&E stain 400x insert. Both specimens showed the proliferation of anaplastic cells with prominent nuclei, hyperchromatic, which is characteristic of the metastatic cell. These cells form epithelial glands, with intervening vessels forming schiller Duval bodies (shown in red arrow). Further, we performed immunohistochemistry, and the result was positive for PanCK and AFP, consistent with an endodermal sinus tumor.
Discussion
Endodermal sinus or yolk sac tumor (YST) is a rare malignant extragonadal NSGC tumor [5]. The World Health Organization (WHO) has divided germ cell tumors into 2 groups. The first group is seminomatous, and the second is a NSGCT [6]. The NSGCT consist of the embryonic tumor, yolk sac tumor (YST), teratoma, and mixed germ cell tumor [7]. Seminomatous germ cell tumor is more prevalent compared to NSGCT. Germ cell tumors are classified according to their location as either extragonadal or gonadal [8]. Extragonadal NSGCT is very rare, with a 2%-5% prevalence among germ cell tumors [9]. It occurs due to the failure of germ cell tumor migration from the urogenital to the genital ridge. It eventually ends up in the retroperitoneal region and anterior mediastinum [8], [9], [10]. The primary metastatic process of the mediastinal NSGC tumor is the lung, bone, and brain. The prevalence of metastatic brain process was low after Cisplatin-based treatment was introduced [11]. The likelihood of brain metastasis increases if there is a relapse in cisplatin-based treatment presence of lung metastases [12].
Primary mediastinal GCT prevail in only <0.5% case of all thoracic outlet tumors [5].
According to a systematic review, only 10 studies of mediastinal germ cell tumors have been reported up to August 2020, with 90% of them being malignant yolk sac tumors. This showed the rarity of primary mediastinal germ cell tumors [10]. Males are more affected than their female counterparts with poor prognoses [13]. Pure yolk sac tumor majority found 40% of children, and mixed-type YST was found in young adults [14]. The retrospective study by Skuari et al. showed a median age of 28.5 years old [4,10,15].
Presentation of primary mediastinal yolk sac tumors that are not specific can mimic other chronic diseases or thoracic outlet compression syndrome [16]. Chronic signs of primary mediastinal YST is weight loss (11%), coughing, and fever (13%). In the area where TBC is endemic, primary mediastinal YST could be misdiagnosed as TBC [17]. Other signs of thoracic outlet compression, such as chest pain, dyspnea, and superior vena cava syndrome, were also present in this case, with a prevalence 23%, 25%, and 10%, respectively [17]. Brain metastatic process characteristic from primary mediastinal NSGCT is less well documented. However, some have reported metastatic processes to the cerebellum, cerebral hemisphere angiomatosis, and intratumoral hemorrhage [11,14,18]. In a retrospective study of 523 patients, one-third of patients with relapsed germ cell tumors and half of the patients with primary germ cell tumors presented with brain metastases were asymptomatic [12]. Metastatic brain processes' clinical signs vary according to their size and location in the brain.
The gold standard for diagnosing primary mediastinal yolk sac tumors is histopathological and immunohistochemistry examination. This could differentiate YST from other NSGCT. The immunohistochemistry profile in YST revealed positive in pan-cytokeratin and Alpha-fetoprotein. Seminoma will give negative results [19].
Surgery, chemotherapy, or combined are available as options for treatment to improve survival rates. Platinum-based chemotherapy is the first-line option. It usually starts with 4 cycles of VIP or BEP. However, research preferred VIP (cisplatin, etoposide, and ifosfamide) compared to BEP (cisplatin, etoposide, and bleomycin) chemotherapy regimens [20]. An observational study involving 221 patients with mediastinal yolk sac tumors with platinum-based chemotherapy showed that 13% got acute respiratory distress with BEP treatment compared to VIP treatment [21]. It is suggested that BEP induce respiratory failure after surgery. However, surgery in a mediastinal yolk sac tumor with a combination of pre- and post-chemotherapy has to be performed. Surgery is suggested to be done after several chemotherapies [8]. The metastatic brain process of YST could be treated with radiotherapy and chemotherapy [22]. Surgical removal is recommended in cases of a single lesion tumor with intratumoral hemorrhage and a tumor diameter >2 cm [11].
Prognosis of Mediastinal yolk sac from the international germ cell cancer collaborative group showed progression-free survival for YST in 5 years, only 35%. It would be below 50% if there were metastatic processes outside the mediastinum [3,23]. Patients with metastatic brain process got 24 months mean survival [22]. This unfavorable prognosis has been attributed to several factors, including the ability for complete surgical resection, advanced stages of the disease, early metastasis, AFP levels, multiple metastatic processes of the brain with a diameter >2 cm, and rapid growth of the tumor [20,22].
Conclusion
Though extremely rare, brain metastases in primary mediastinal YST have a poor prognosis. Signs and symptoms are not specific, so physicians should be more aware and reevaluate patient diagnosis [5]. As opposed to a single treatment, multimodal treatment, including pre-chemotherapy, surgery, and post-surgical chemotherapy, gives better outcomes. Craniotomy resection with a combination of radiation therapy can be done in case of cerebral metastatic process [24]. The current management of NSGCT with cerebral metastasis is not optimized due to the scarcity of cases. Adapting therapy with a multi-disciplinary approach is the best choice for understanding and treating the disease [16].
Provenance and peer review
Not commissioned, externally peer-reviewed.
Patient consent
Written informed consent for the publication of this case report was obtained from a relative of the patient.
Acknowledgments
The authors would like to thank all lecturers, family, and friends who have been teaching and supporting us.
Footnotes
Funding: The authors declared that no grants were involved in supporting this work.
Competing Interests: There is no declaration of interest.
References
- 1.Williamson SR, Delahunt B, Magi-Galluzzi C, Algaba F, Egevad L, Ulbright TM, et al. The World Health Organization 2016 classification of testicular germ cell tumours: a review and update from the International Society of Urological Pathology Testis Consultation Panel. Histopathology. 2017;70:335–346. doi: 10.1111/his.13102. [DOI] [PubMed] [Google Scholar]
- 2.Abdul Rahman R, Mohamad Sukri N, Md Nazir N, Ahmad Radzi MA, Zulkifly AH, Che Ahmad A, et al. The potential of 3-dimensional construct engineered from poly(lactic-co-glycolic acid)/fibrin hybrid scaffold seeded with bone marrow mesenchymal stem cells for in vitro cartilage tissue engineering. Tissue Cell. 2015;47:420–430. doi: 10.1016/j.tice.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Mead GM. International germ cell consensus classification: a prognostic factor- based staging system for metastatic germ cell cancers. J Clin Oncol. 1997;15:594–603. doi: 10.1200/JCO.1997.15.2.594. [DOI] [PubMed] [Google Scholar]
- 4.Papaioannou A, Porpodis K, Spyratos D, Zarogoulidis K. Yolk sac tumour in the anterior mediastinum. Pneumon. 2013;26:361–365. [Google Scholar]
- 5.Zarif K, Benbrahim Z, Acharfi N, Khacha A, Maaroufi M, Amaadour L, et al. A primary mediastinal germ cell tumor of yolk sac type: case report. Pan Afr Med J. 2021;38:300–304. doi: 10.11604/pamj.2021.38.330.23730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haloua M, Bouardi NEl, Hbibi M, Alami BE, Lamrani YA, Maaroufi M, et al. Intracranial bifocal germinoma. Radiol Case Rep. 2022;17:3015–3018. doi: 10.1016/j.radcr.2022.05.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anindhita T, Andriani R, Malueka RG, editors . Tumor Otak Sekunder (Metastasis). buku ajar neuroonkologi. 1st ed. Jakarta: Perdossi; 2019. p. 199–209.
- 8.Nakhla SG, Sundararajan S. A rare case of primary anterior mediastinal yolk sac tumor in an elderly adult male. Case Rep Oncol Med. 2016;2016:1–4. doi: 10.1155/2016/8961486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atmaca AF, Altınova S, Canda AE, Ozcan MF, Alıcı S, Memıs L, et al. Retroperitoneal extragonadal nonseminomatous germ cell tumor with synchronous orbital metastasis. Adv Urol. 2009;2009:1–3. doi: 10.1155/2009/419059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu X, Li D, Xia J, Wang P, Cai J. Mediastinal mixed germ cell tumor: a case report and literature review. Open Med. 2021;16:892–898. doi: 10.1515/med-2021-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Forquer JA, Harkenrider M, Fakiris AJ, Timmerman RD, Cavaliere R, Henderson MA, et al. Brain metastasis from non-seminomatous germ cell tumor of the testis. Expert Rev Anticancer Ther. 2007;7:1567–1580. doi: 10.1586/14737140.7.11.1567. [DOI] [PubMed] [Google Scholar]
- 12.Feldman DR, Lorch A, Kramar A, Albany C, Einhorn LH, Giannatempo P, et al. Brain metastases in patients with germ cell tumors: prognostic factors and treatment options—an analysis from the Global Germ Cell Cancer Group. J Clin Oncol. 2016;34:345–351. doi: 10.1200/JCO.2015.62.7000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raoufi M, Herrick L, Benali A, Achaachi L, El Ftouh M, Bellarbi S, et al. Mediastinal mature teratoma revealed by empyema. Case Rep Pulmonol. 2016;2016:1–4. doi: 10.1155/2016/7869476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kan P, Gottfried ON, Blumenthal DT, Liu JK, Salzman KL, Townsend J, et al. Primary spinal yolk sac tumor with brain metastasis: case report and review of the literature. J Neurooncol. 2006;78:249–253. doi: 10.1007/s11060-005-9022-z. [DOI] [PubMed] [Google Scholar]
- 15.Sakurai H, Asamura H, Suzuki K, Watanabe S -i., Tsuchiya R. Management of primary malignant germ cell tumor of the mediastinum. Jpn J Clin Oncol. 2004;34:386–392. doi: 10.1093/jjco/hyh062. [DOI] [PubMed] [Google Scholar]
- 16.Noor M, Leal BL, Patel D. A rare case of primary mediastinal endodermal sinus tumor presenting with hemoptysis. Cureus. 2020;12:10–13. doi: 10.7759/cureus.9517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu J, Tian B, Zeng Q, Chen C, Zhou C, Li H, et al. Mediastinal teratoma presenting with hemoptysis and pleuritis misdiagnosed as tuberculosis (empyema) BMC Pediatr. 2018;18:1–6. doi: 10.1186/s12887-018-1357-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Monroy-Sosa A, Reyes-Soto G, Cacho-Díaz B, Granados-García M, Estrada AH, Cano-Valdez AM, et al. Brain angiometastasis from a non-seminomatous germ cell tumor: a case report. Int J Surg Case Rep. 2018;42:44–49. doi: 10.1016/j.ijscr.2017.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu F, Wang L, Zhai X. Primary mediastinal yolk sac tumor : a case report and literature review. Int J Clin Exp Pathol. 2020;13:2772–2777. [PMC free article] [PubMed] [Google Scholar]
- 20.Liu B, Lin G, Liu J, Liu H, Shang X, Li J. Primary mediastinal yolk sac tumor treated with platinum-based chemotherapy and extended resection: report of seven cases. Thorac Cancer. 2018;9:491–494. doi: 10.1111/1759-7714.12591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmoll HJ, Souchon R, Krege S, Albers P, Beyer J, Kollmannsberger C, et al. European consensus on diagnosis and treatment of germ cell cancer: a report of the European Germ Cell Cancer Consensus Group (EGCCCG) Ann Oncol. 2004;15:1377–1399. doi: 10.1093/annonc/mdh301. [DOI] [PubMed] [Google Scholar]
- 22.Salvati M, Piccirilli M, Raco A, Santoro A, Frati R, Lenzi J, et al. Brain metastasis from non-seminomatous germ cell tumors of the testis. Neurosurg Rev. 2006;29:130–137. doi: 10.1007/s10143-005-0004-6. [DOI] [PubMed] [Google Scholar]
- 23.Zain SM, Mirchia K, Galbraith K, Galgano MA, Lee M, Richardson TE, et al. Mediastinal metastases from a primary immature teratoma of the CNS. Radiol Case Rep. 2022;17:3339–3344. doi: 10.1016/j.radcr.2022.06.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nia AM, Allison RZ, Sweeney M, Briner RP. Late testicular yolk sac tumor with cerebellar metastasis and a rapid recurrence after a gross total resection: a case report. Cureus. 2021;13:1–5. doi: 10.7759/cureus.17143. [DOI] [PMC free article] [PubMed] [Google Scholar]