Abstract
Pulmonary fibrosis (PF) is a serious and often fatal illness that occurs in various clinical settings and represents a significant unmet medical need. Increasing evidence indicates that neutrophil extracellular traps (NETs) contribute significantly to the progression of PF. Therefore, understanding the pathways by which NETs contribute to the disease is crucial for developing effective treatments. This review focuses on the formation of NETs and the common mechanisms of NETs in PF.
Keywords: Pulmonary fibrosis, Neutrophil extracellular traps, Interstitial lung disease
Highlights
1. This review focuses on NETs formation and the role of NETs in PF and presents research progress.
2. We describe specific mechanisms by which NETs induce PF in fibroblasts while revealing the transduction mechanisms that remain to be investigated.
3. We explore the possible consequences of NETs action on lung epithelial cells, including NETs-induced lung epithelial damage and NETs-driven epithelial mesenchymal transition.
4. We introduce recent key findings about the role of NETs-mediated chronic inflammation in PF and the effect of autophagy-driven production of NETs in fibrosis.
Introduction
Neutrophil extracellular traps (NETs), a meshwork structure that captures bacteria, fungi and viruses, were discovered by Volker Brinkmann in 2004 [1]. DNA, histones, and antimicrobial proteins are found in NETs, which are produced by activated neutrophils, and high concentrations of NETs around pathogens are considered antibacterial. NETs play an important role in host defense mechanisms and in non-infectious diseases, such as autoimmune diseases, vasculitis, psoriasis and other pathological processes, including coagulation, thrombosis [2, 3], diabetes mellitus [4], atherosclerosis [5, 6], cystic fibrosis [7] and malignant tumors [8, 9]. Furthermore, elevated levels of NETs have been detected in tissues of patients with PF, and they are associated with disease progression [10]. Evidence indicates that NETs components such as DNA, myeloperoxidase (MPO), neutrophil elastase (NE) and histones release cytokines that lead to inflammation, epithelial-mesenchymal transformation (EMT) or epithelial damage, all of which promote the progression of lung fibrosis. In this review, we discuss the formation of NETs, their role in PF and current advances in studying NETs in PF.
Role and formation of NETs
As the body’s primary defense cells, neutrophils enhance the immune response by phagocytosis, degranulation and release of reactive oxygen species (ROS) [11–13]. NETs are extracellular structures composed of chromatin and granule proteins that bind and kill microorganisms. NETosis is the process of cell death following neutrophil activation, which differs from apoptosis and necrosis in morphological and molecular features. This novel form of cell death involves the formation of NETs and then continuing to play an important role in the immune response [1, 14].
Research has demonstrated that activated NADPH oxidase may produce ROS, and the main pathways that activate NADPH oxidase include PKC-Raf, MERK/ERK and PI3K/Akt [15–17]. In response to the generated ROS, MPO is stimulated, and elastase is activated and migrates from asplenophilic granules to the nucleus by the synergistic action of ROS and MPO [18, 19]. As NETs form, NE digests nucleosomal histones and promotes extensive chromatin deglycosylation, late binding of MPO to chromatin stimulates NE to depolymerize chromatin, and granulins bind to depolymerized chromatin released by neutrophils [20]. Notably, a portion of the formed NETs is mediated by mitochondrial ROS without NADPH oxidase activity [21, 22]. Peptidylarginine deiminase type 4 (PAD4) is involved in developing NETs because PAD4-Knock out (KO) mice were found to eliminate NETs and induce histone guanylation, and this increase in histone guanylation was associated with chromatin deprotonation during NETs formation [23]. By converting histone arginine to citrulline, PAD4 reduces the strong positive charge of histones, thus weakening histone DNA binding. This weakened interaction causes nucleosome unpacking and chromatin depolymerization [24]. Interestingly, according to a recent study, the formation of NETs is independent of ROS and may result from the multitude of molecules released by Staphylococcus aureus during neutrophil cleavage [25].
Interstitial lung disease
Interstitial lung disease (ILD), also called diffuse parenchymal lung disease, is a group of disease with diffuse lung parenchymal, alveolar inflammation and interstitial fibrosis as basic pathological changes [26]. ILD is etiologically complex and is associated with more than 200 diseases, which can be categorized according to known etiology (such as environmental exposure, drug toxicity and connective tissue disease) or unknown etiology (such as idiopathic pulmonary fibrosis (IPF)) [27]. IPF, the most common and aggressive form of ILD, is characterized by the imaging and pathologic features of conventional interstitial pneumonia without an established etiology or correlation with PF-related diseases [28]. According to current estimates, IPF prevalence ranges from 0.57 to 4.51 per 10,000 people in Asia-Pacific countries, 0.33 to 2.51 in Europe, and 2.40 to 2.98 in North America [29]. ILD is also a common pulmonary complication in patients with connective tissue diseases (CTDs). Various CTDs, such as rheumatoid arthritis, systemic sclerosis (SSc), polymyositis and dermatomyositis, Sjögren’s syndrome (SS), systemic lupus erythematosus (SLE) and Mixed Connective Tissue Disease ILD (MCTD), are associated with ILD [30–33]. There has been a high but divergent reported incidence of ILD among patients with SSc, ranging from 40 to 91% [34, 35]. According to several studies, the prevalence of pulmonary involvement in SS varies widely from 9 to 26% [36, 37]. Based on HRCT and PFT findings, ILD is reported in 47 to 90% of patients with MCTD, whereas ILD is reported in 1 to 15% of patients with SLE [38]. Although PF remains a rare disease, statistics show that the mortality rate is steadily increasing (from 18.81 per 100,000 people in 2000 to 20.66 per 100,000 people in 2017) [39, 40]. A rising mortality rate indicates that PF remains a pressing challenge and that a deeper understanding of its pathogenesis is necessary. In addition to having an innate immune response, NETs may direct the progression and occurrence of fibrosis, making them a new target for anti-fibrotic therapies.
NETs induce pulmonary fibrosis through fibroblasts
Fibroblasts that form the lung connective tissue are derived mainly from embryonic mesenchymal cells. Lung fibroblasts, as the main constituent cells of lung connective tissue, are postulated to perform the following functions under physiological conditions: maintain the normal shape of lung tissue, provide the scaffold to facilitate effective gas exchange of lung tissue, and synthesize and secrete a variety of proteins, collagen fibers and other extracellular matrix components after lung tissue damage has been rapidly repaired [41–43].Under pathological conditions, inflammation of the alveolar epithelial cells and sustained damage cause the recruitment of large numbers of immune cells, which then produce and release pro-inflammatory and pro-fibrotic factors [44, 45]. As a result of the combined action of various cytokines, lung fibroblasts are abnormally activated. Activated lung fibroblasts are the key effector cells of PF. They can, for example, contribute directly to the occurrence and development of PF through abnormal proliferation, phenotypic transformation, and secretion of extracellular matrix (ECM) components [46–48]. Moreover, lung fibroblasts can indirectly promote fibrosis by secreting inflammatory factors such as Interleukin-1(IL-1), IL-6, and tumor necrosis factor-alpha (TNF-α) [49].
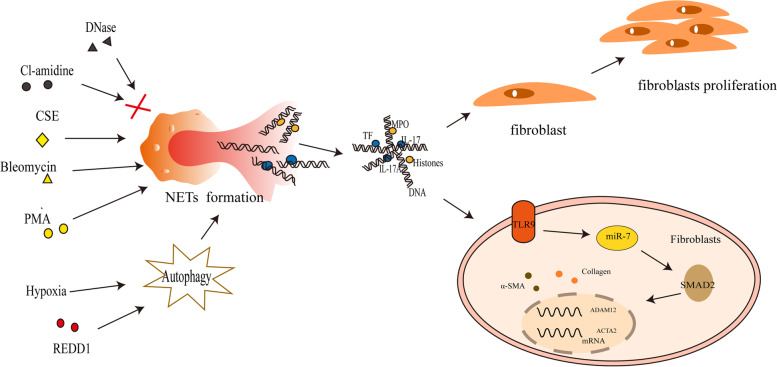
NETs play a crucial role in the activation of lung fibroblasts and their differentiation into myofibroblasts. Effects of NETs components MPO and histones on the proliferation and differentiation of lung fibroblast were confirmed by MPO inhibitor or histones inhibitor with the down-regulation of alpha-smooth muscle actin(α-SMA) and collagen production. Whereas pre-treated with recombinant human MPO (rhMPO) and rhhistones3 promoted the expression of α-SMA, the collagen production and the proliferation of lung fibroblasts. And the DNA components of NETs was confirmed by Toll-like receptor 9(TLR9)-miR-7-drosophila mothers against decapentaplegic 2(Smad2) signaling pathway to promote lung fibroblast proliferation and their differentiation into myofibroblasts [50]. In vitro activation and differentiation of human lung fibroblasts into myofibroblasts by NETs released from neutrophils treated with phorbol 12-myristate 13-acetate (PMA) resulted in elevated mRNA levels for a disintegrin and metalloprotease 12 (ADAM12), actin alpha 2 (ACTA2) and protein levels for the mesenchymal marker α-SMA and collagen production. However, the activity of NETs on lung fibroblasts after digestion with DNase was eliminated [51], indicating that DNA components in NETs likely influence the differentiation of fibroblasts positively. Despite not directly stimulating fibrotic responses on fibroblasts in vitro, the fibrosis-inducing drugs, cigarette smoke extract (CSE), magnesium silicate and bleomycin indirectly induce fibroblast activation through NETs release [51]. Furthermore, these investigators found that the expression of IL-17 in NETs components did not affect the differentiation of lung fibroblasts into myofibroblasts, but IL-17 acted in concert with DNA/histones in NET-dependent fibroblast activation. The derived components of NETs produced under different conditions vary, and although they do not directly determine the activated differentiation of fibroblasts, they can indirectly participate in their fibrogenesis process [51]. Studies showed that active SLE expresses tissue factor (TF)-bearing and IL-17A-bearing NETs, which activate and differentiate human skin fibroblasts. In elucidating the components of NETs responsible for activation and differentiation of human skin fibroblasts, TF and IL-17A were found, in particular, to decorate active SLE NETs. Researchers assessed the expression of ACAT2 and found that TF or IL-17A neutralization of NETs did not mediate human skin fibroblasts activation/differentiation. Collectively, these results demonstrate that active SLE NETs contribute to the activation/differentiation of human skin fibroblasts, whereas TF and IL-17A present in SLE NETs enhance the fibrotic activity of differentiated human skin fibroblasts [52]. Together, these findings indicate the presence of NET-derived components, suggesting their involvement in fibrotic aspects. Although some authors have demonstrated the effects of different components of NETs on lung fibroblast proliferation and differentiation, the mechanisms by which some components of NETs exert these effects remain unclear.
PAD4 also promotes the release of NETs through histone guanylation [24]. Inducing PF in PAD4-KO mice with bleomycin suppressed the expression of fibrosis-associated mediators significantly, including collagen type I α 1 chain, elastin, fibronectin 1, connective tissue growth factor and fibroblast growth factor 2 [53]. The PAD4 deficiency prevented a decrease in alveolar epithelial and pulmonary vascular endothelial cell numbers and increased ACTA2-positive mesenchymal cells and S100A4-positive fibroblasts in the lung. Pretreatment of neutrophils with Cl-amidine, a PAD4 inhibitor that inhibits NETs release by blocking guanylation of histone H3 and subsequent incubation with cigarette smoke extract inhibited the differentiation and activation of fibroblasts [53]. The findings suggest that the PAD4 inhibitor is a therapeutic target for PF because it reduces bleomycin-induced NETs and fibrosis formation. This promising research area will require further investigation into how anti-NETs interrupt PF and represents a potential treatment (Fig. 1).
Fig. 1.
NETs induce pulmonary fibrosis through fibroblasts. PMA, Bleomycin, CSE could promote the release of NETs from neutrophils. Under hypoxia conditions, REDD1 promotes NETs release by enhancing autophagy, while Cl-amidine (a PAD4 inhibitor) and DNase prevent NETs production and action process. It has been suggested that MPO and Histones contribute to the proliferation and differentiation of fibroblasts, whereas DNA promotes myofibroblast differentiation by connecting with the pathway TLR9-miR-7-SMAD2. There is evidence that IL-17, IL17A, and TF promote fibrotic activity in differentiated fibroblasts, but not their differentiation. NETs: neutrophil extracellular traps; PMA: phorbol 12-myristate 13-acetate; CSE: cigarette smoke extract; PAD4: peptidylarginine deiminase type 4; MPO: myeloperoxidase
NETs drive lung epithelial injury and pulmonary fibrosis
Repetitive injury and alterations of the alveolar epithelium (including alveolar epithelial cell proliferation and hyperplasia) [54], abnormal alveolar epithelial cell activation that leads to impaired epithelial-mesenchymal crosstalk [55] and senescence of pulmonary epithelial cells [56] have been described and linked with the development of PF. Currently, PF is postulated to be caused by repeated damage to alveolar epithelial cells, which can cause abnormal interactions between epithelial cells and fibroblasts [57, 58]. Cell death of alveolar epithelial may occur during the early stages of PF [59, 60], in which alveolar epithelial cell type II (ATII) damage is significant, and there have been reports that in the lungs of patients with IPF, 70–80% of the ATII stained positive for apoptotic markers [61, 62].
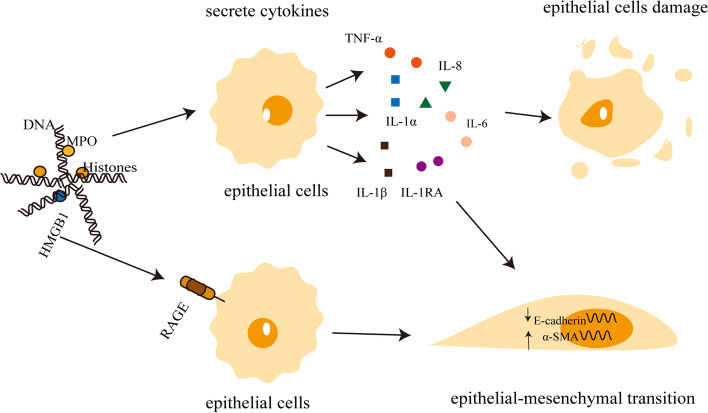
NETs play various roles in lung epithelial injury and fibrosis. For example, protein components of NETs, particularly histones, caused epithelial and endothelial cell death in a mouse model of acute lung injury induced by lipopolysaccharide [63]. In vitro, extracellular histones are cytotoxic to endothelial cells, while in vivo, histone administration leads to neutrophil margins, vacuolar endothelial cells, intra-alveolar hemorrhage, and macro- and microvascular thrombosis [64]. Other pathways besides NETs-DNA may also damage lung epithelial cells, such as NETs mediating inflammasome activation and IL-1β secretion from monocytes and causing airway epithelial cell injury, and NETs modify and regulate lung injury by activating ferroptosis in alveolar epithelial [65–67]. Additionally, NETs are associated with the development of lung fibrosis after COVID-19, because NETs induce the downregulation of the epithelial marker E-cadherin and the upregulation of the mesenchymal marker α-SMA in pulmonary epithelial cells [68–71]. Exposure to butyl benzyl phthalate (BBP), a widely used plasticizer, has been linked to asthma and impaired lung functions [72, 73]. As a consequence of promoting glucose uptake and ROS burst in neutrophils, BBP promotes EMT through the formation of NETs [74]. The regulation of NETs on lung epithelial cells is primarily determined by epithelial cell injury and mesenchymal transition, and there remains much to be learned about the role of NETs in driving pulmonary epithelial injury and PF.
NETs-mediated inflammation and pulmonary fibrosis
PF is commonly associated with chronic inflammation. A complex network of cytokines, chemokines and inflammatory mediums are released during the process of PF, driving fibroblast recruitment, proliferation and overproduction of ECM. Key cytokines and chemokines that induce a pro-fibrotic environment include TNF-α, transforming growth factor-β (TGF-β), monocyte chemotactic protein 1 (MCP1)/CCL2, macrophage inhibitory protein 1α (MIP1α)/ CCL3 and T-2-chemokines such as CCL17, CCL18 and CCL22 [75, 76]. TGF-β is an important mediator of pro-fibrosis and induces fibroblast differentiation into myofibroblasts. TGF-β also promotes ECM production by promoting ECM gene transcription (including collagen, fibronectin and proteoglycan) and preventing collagen degradation by inhibiting matrix metalloproteinase, fibrinogen activator and elastase activities [58, 77, 78]. NE is a main protein component of NETs and an inhibitor of NE has been demonstrated to attenuate PF in a murine model by inhibiting TGF-β1 and inflammatory cell recruitment to the lungs [79]. The mechanism by which NETs rely on TGF-β as a signaling pathway has not been investigated in detail; however, NETs have been shown to activate TGF-β in other diseases. For example, NETs induce proliferation, invasion, migration, and EMT of gastric cancer cells by activating the TGF-β-p-Smad2/3 signaling pathway [80]. NETs are associated with the upregulation of the TGF-β signaling pathway and associated genes, including TGF-β1, Smad3 and collagen type III α 1 chain in chronic thromboembolic pulmonary hypertension monocytes. Further studies have indicated that NETs-dependent monocyte differentiation causes a predominantly fibroblast phenotype with increased TGF-β-dependent signal transduction [2]. TGF-β may act as a downstream molecule of NETs to promote the progression of PF. Moreover, NETs may promote the release of TGF-β, an important agent for tissue remodeling after acute lung injury during late phases [81]. According to existing studies, NETs probably activate the TGF-β signaling pathway in lung fibroblasts to promote PF progression. Confirmation of this activation process requires further research efforts.
NETs also stimulate the alveolar and bronchial epithelial cells to secrete pro-inflammatory factors such as IL-8 and IL-6, not by inducing DNA or histones in the cells, but by releasing the high mobility group box 1 (HMGB1) protein. HMGB1 induces the secretion of IL-8 and IL-6 via the receptor of advanced glycation end-product (RAGE) [82]. Studies have shown that the mRNA of RAGE is highly expressed in alveolar epithelial cells and the nuclear protein HMGB-1 was also identified in NETs [83]. HMGB-1 was also shown to induce the release of pro-inflammatory cytokines when released into the extracellular environment [84–86]. IL-17A acts as a pro-inflammatory factor that promotes PF by depending on NETs [51, 87]. Furthermore, NETs also promote the release of cytokines such as IL-1, TNF-α, IL-1RA and IL-1α [51, 88, 89]. The essential role of NETs-produced inflammatory factors is clearly important in PF progression. Interestingly, Chirivi and his colleagues described the inhibition of NETs with the therapeutic anti-citrullinated protein antibody (tACPA) for the first time in mice models. By using tACPA, it may be possible to reduce neutrophil-driven inflammation and decrease lung fibrosis [90]. According to the evidence presented above, NETs cause chronic lung inflammation by producing a series of inflammatory factors that, in turn, stimulate fibrotic pathways downstream in cells (such as lung epithelial cells, fibroblasts and immune cells) to accelerate the progression of PF (Fig. 2).
Fig. 2.
NETs drive lung epithelial injury and pulmonary fibrosis. MPO, DNA and histones in Nets can cause damage to alveolar epithelial cells, which release a large number of pro-inflammatory and pro-fibrotic factors (including IL-6, IL-8, IL-1α, IL-1β and TNF-α) and initiate subsequent inflammatory immune repair. Excessive repair of alveolar epithelial cells after injury is an important mechanism of pulmonary fibrosis. HMGB1 in NETs could act on the RAGE receptors in lung epithelial cells, which in turn leads to the downregulation of the epithelial cell marker E-cadherin and the upregulation of the myofibroblast cell marker α-SMA. NETs: neutrophil extracellular traps; MPO: myeloperoxidase; HMGB1: high mobility group box 1; RAGE: the receptor of advanced glycation end-product; α-SMA: alpha-smooth muscle actin
Autophagy-driven NETs and pulmonary fibrosis
Autophagy is a self-degradative process responsible for balancing energy sources during critical developmental stages and in response to nutrient stress [91]. Rather than eliminating materials, autophagy serves as a dynamic recycling system that creates new building blocks and energy to maintain the integrity of cells and homeostasis. Abnormalities in the autophagic process may cause the development of diseases [92]. Autophagy is involved in the NETosis process, and different types of vesicles with a double phospholipid bilayer are found in PMA-stimulated neutrophils and monitoring the localization of the autophagy marker microtubule-associated protein 1 light chain 3 suggests that PMA induces autophagy in a superoxide-independent manner. Additionally, the pharmacological inhibition of autophagy did not affect the activity of PMA-induced NADPH oxidase [93]. A significant reduction in the release of NETs was observed after treating neutrophils with the autophagy inhibitors bafilomycin A1 and chloroquine [51, 94]. Typically, autophagy is a protective mechanism for an organism, with enhanced autophagy reducing the progression of PF [95–99]. In contrast excess of autophagy stimulates the activation of fibroblasts and causes tissue fibrosis. For example, the coactivator peroxisome proliferator-activated receptor gamma coactivator-1α is upregulated in SSc patients and mouse animal models to promote autophagy for TGF-β-induced fibroblasts activation [100]. TGF-β also activates autophagy through epigenetic mechanisms to amplify its pro-fibrotic effects [101]. The hypoxia-response and stress-response protein (REDD1)/ autophagy/ NETs axis is involved in kidney injury and dermatofibrosis in patients with SLE. Studies showed that endothelin-1 and hypoxia-inducible factor-1α inhibition, prior to stimulation of neutrophils with an active serum, ameliorated the activation/differentiation of human skin fibroblasts to myofibroblasts, indicating the importance of NETs in the activation/differentiation of fibroblasts [52]. Additionally, the REDD1/autophagy pathway has been reported to induce NETs and increase IL-1β secretion [102]. Although the regulatory mechanism of PF by autophagy/NETs has not been fully resolved, we were able to detect a possible role for autophagy/NETs in PF regulation.
Conclusion
NETs are associated with the early and advanced stages of PF. Evidence suggests that NETs may regulate the fibrosis process by causing pro-inflammatory effects, injuring pulmonary epithelium and endothelium, promoting pulmonary EMT, activating lung fibroblasts, or inducing autophagy. Further research is required to fully understand how NETs interact with cells and downstream signaling pathways during lung fibrosis. Current research on NETs and PF is based primarily on basic experiments, and potential clinical transformation still requires further exploration. Signaling pathways and molecular targets related to NETs have been partially identified, so inhibiting NETs to delay disease progression or onset should still be possible.
Acknowledgements
Not applicable.
Abbreviations
- PF
Pulmonary fibrosis
- NETs
Neutrophil extracellular traps
- MPO
Myeloperoxidase
- NE
Neutrophil elastase
- EMT
Epithelial-mesenchymal transformation
- ROS
Reactive oxygen species
- PAD4
Peptidylarginine deiminase type 4
- ILD
Interstitial lung disease
- IPF
Idiopathic pulmonary fibrosis
- CTDs
Connective tissue diseases
- SSc
Systemic sclerosis
- SS
Sjögren’s syndrome
- SLE
Systemic lupus erythematosus
- MCTD
Mixed Connective Tissue Disease ILD
- ECM
Extracellular matrix
- IL-1
Interleukin-1
- TNF-α
Tumor necrosis factor alpha
- rhMPO
Recombinant human MPO
- TLR9
Toll-like receptor9
- PMA
Phorbol 12-myristate 13-acetate
- ADAM12
A disintegrin and metalloprotease 12
- ACTA2
Actin alpha 2
- TF
Tissue factor
- α-SMA
Alpha-smooth muscle actin
- CSE
Cigarette smoke extract
- ATII
Alveolar epithelial cell type II
- Smad2
Drosophila mothers against decapentaplegic2
- BBP
Butyl benzyl phthalate
- TGF-β
Transforming growth factor-β
- MCP1/CCL2
Monocyte chemotactic protein 1
- MIP1α/ CCL3
Macrophage inhibitory protein 1α
- HMGB1
High mobility group box 1
- tACPA
Therapeutic anti-citrullinated protein antibody
- REDD1
The hypoxia-response and stress-response
- RAGE
The receptor of advanced glycation end-product
Authors’ contributions
Suyan Yan,Meiqi Li and Baocheng Liu wrote different sections of the manuscript. Zhenzhen Ma and Qingrui Yang prepared, revised, and wrote the manuscript. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication. The author(s) read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (Youth fund project, Grant NO.82201994) and the Natural Science Foundation of Shandong Province (General Program, Grant No.ZR2022MH016 and Youth fund project, Grant No. ZR2021QH043).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Suyan Yan, Email: ysyzm1025@163.com.
Meiqi Li, Email: l_meiq@163.com.
Baocheng Liu, Email: 1342721850@qq.com.
Zhenzhen Ma, Email: mazhenzhendz@163.com.
Qingrui Yang, Email: qryang720@163.com.
References
- 1.Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303(5663):1532–1535. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- 2.Sharma S, Hofbauer TM, Ondracek AS, Chausheva S, Alimohammadi A, Artner T, et al. Neutrophil extracellular traps promote fibrous vascular occlusions in chronic thrombosis. Blood. 2021;137(8):1104–1116. doi: 10.1182/blood.2020005861. [DOI] [PubMed] [Google Scholar]
- 3.Zhang H, Zhou Y, Qu M, Yu Y, Chen Z, Zhu S, et al. Tissue factor-enriched neutrophil extracellular traps promote immunothrombosis and disease progression in sepsis-induced lung injury. Front Cell Infect Microbiol. 2021;11:677902. doi: 10.3389/fcimb.2021.677902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta A, Singh K, Fatima S, Ambreen S, Zimmermann S, Younis R, et al. Neutrophil extracellular traps promote NLRP3 inflammasome activation and glomerular endothelial dysfunction in diabetic kidney disease. Nutrients. 2022;14(14):2965. doi: 10.3390/nu14142965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Josefs T, Barrett TJ, Brown EJ, Quezada A, Wu X, Voisin M, et al. Neutrophil extracellular traps promote macrophage inflammation and impair atherosclerosis resolution in diabetic mice. JCI Insight. 2020;5(7):e134796. doi: 10.1172/jci.insight.134796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warnatsch A, Ioannou M, Wang Q, Papayannopoulos V. Neutrophil extracellular traps license macrophages for cytokine production in atherosclerosis. Science. 2015;349(6245):316–320. doi: 10.1126/science.aaa8064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kummarapurugu AB, Zheng S, Ma J, Ghosh S, Hawkridge A, Voynow JA. Neutrophil elastase triggers the release of macrophage extracellular traps: relevance to cystic fibrosis. Am J Respir Cell Mol Biol. 2022;66(1):76–85. doi: 10.1165/rcmb.2020-0410OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xiao Y, Cong M, Li J, He D, Wu Q, Tian P, et al. Cathepsin C promotes breast cancer lung metastasis by modulating neutrophil infiltration and neutrophil extracellular trap formation. Cancer Cell. 2021;39(3):423–437.e7. doi: 10.1016/j.ccell.2020.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Yang L, Liu Q, Zhang X, Liu X, Zhou B, Chen J, et al. DNA of neutrophil extracellular traps promotes cancer metastasis via CCDC25. Nature. 2020;583(7814):133–138. doi: 10.1038/s41586-020-2394-6. [DOI] [PubMed] [Google Scholar]
- 10.Negreros M, Flores-Suárez LF. A proposed role of neutrophil extracellular traps and their interplay with fibroblasts in ANCA-associated vasculitis lung fibrosis. Autoimmun Rev. 2021;20(4):102781. doi: 10.1016/j.autrev.2021.102781. [DOI] [PubMed] [Google Scholar]
- 11.Mortaz E, Alipoor SD, Adcock IM, Mumby S, Koenderman L. Update on neutrophil function in severe inflammation. Front Immunol. 2018;9:2171. doi: 10.3389/fimmu.2018.02171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amulic B, Cazalet C, Hayes GL, Metzler KD, Zychlinsky A. Neutrophil function: from mechanisms to disease. Annu Rev Immunol. 2012;30:459–489. doi: 10.1146/annurev-immunol-020711-074942. [DOI] [PubMed] [Google Scholar]
- 13.Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol. 2011;11(8):519–531. doi: 10.1038/nri3024. [DOI] [PubMed] [Google Scholar]
- 14.Fuchs TA, Abed U, Goosmann C, Hurwitz R, Schulze I, Wahn V, et al. Novel cell death program leads to neutrophil extracellular traps. J Cell Biol. 2007;176(2):231–241. doi: 10.1083/jcb.200606027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El Benna J, Han J, Park JW, Schmid E, Ulevitch RJ, Babior BM. Activation of p38 in stimulated human neutrophils: phosphorylation of the oxidase component p47phox by p38 and ERK but not by JNK. Arch Biochem Biophys. 1996;334(2):395–400. doi: 10.1006/abbi.1996.0470. [DOI] [PubMed] [Google Scholar]
- 16.Dewas C, Fay M, Gougerot-Pocidalo MA, El-Benna J. The mitogen-activated protein kinase extracellular signal-regulated kinase 1/2 pathway is involved in formyl-methionyl-leucyl-phenylalanine-induced p47phox phosphorylation in human neutrophils. J Immunol. 2000;165(9):5238–5244. doi: 10.4049/jimmunol.165.9.5238. [DOI] [PubMed] [Google Scholar]
- 17.Hoyal CR, Gutierrez A, Young BM, Catz SD, Lin J-H, Tsichlis PN, et al. Modulation of p47PHOX activity by site-specific phosphorylation: Akt-dependent activation of the NADPH oxidase. Proc Natl Acad Sci U S A. 2003;100(9):5130–5135. doi: 10.1073/pnas.1031526100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ermert D, Urban CF, Laube B, Goosmann C, Zychlinsky A, Brinkmann V. Mouse neutrophil extracellular traps in microbial infections. J Innate Immun. 2009;1(3):181–193. doi: 10.1159/000205281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Metzler KD, Goosmann C, Lubojemska A, Zychlinsky A, Papayannopoulos V. A myeloperoxidase-containing complex regulates neutrophil elastase release and actin dynamics during NETosis. Cell Rep. 2014;8(3):883–896. doi: 10.1016/j.celrep.2014.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papayannopoulos V, Metzler KD, Hakkim A, Zychlinsky A. Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J Cell Biol. 2010;191(3):677–691. doi: 10.1083/jcb.201006052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Douda DN, Khan MA, Grasemann H, Palaniyar N. SK3 channel and mitochondrial ROS mediate NADPH oxidase-independent NETosis induced by calcium influx. Proc Natl Acad Sci U S A. 2015;112(9):2817–2822. doi: 10.1073/pnas.1414055112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lood C, Blanco LP, Purmalek MM, Carmona-Rivera C, De Ravin SS, Smith CK, et al. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat Med. 2016;22(2):146–153. doi: 10.1038/nm.4027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neeli I, Khan SN, Radic M. Histone deimination as a response to inflammatory stimuli in neutrophils. J Immunol. 2008;180(3):1895–1902. doi: 10.4049/jimmunol.180.3.1895. [DOI] [PubMed] [Google Scholar]
- 24.Li P, Li M, Lindberg MR, Kennett MJ, Xiong N, Wang Y. PAD4 is essential for antibacterial innate immunity mediated by neutrophil extracellular traps. J Exp Med. 2010;207(9):1853–1862. doi: 10.1084/jem.20100239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pilsczek FH, Salina D, Poon KKH, Fahey C, Yipp BG, Sibley CD, et al. A novel mechanism of rapid nuclear neutrophil extracellular trap formation in response to Staphylococcus aureus. J Immunol. 2010;185(12):7413–7425. doi: 10.4049/jimmunol.1000675. [DOI] [PubMed] [Google Scholar]
- 26.Montesi SB, Fisher JH, Martinez FJ, Selman M, Pardo A, Johannson KA. Update in interstitial lung disease 2019. Am J Respir Crit Care Med. 2020;202(4):500–507. doi: 10.1164/rccm.202002-0360UP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Podolanczuk AJ, Wong AW, Saito S, Lasky JA, Ryerson CJ, Eickelberg O. Update in interstitial lung disease 2020. Am J Respir Crit Care Med. 2021;203(11):1343–1352. doi: 10.1164/rccm.202103-0559UP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wijsenbeek M, Cottin V. Spectrum of fibrotic lung diseases. N Engl J Med. 2020;383(10):958–968. doi: 10.1056/NEJMra2005230. [DOI] [PubMed] [Google Scholar]
- 29.Maher TM, Bendstrup E, Dron L, Langley J, Smith G, Khalid JM, et al. Global incidence and prevalence of idiopathic pulmonary fibrosis. Respir Res. 2021;22(1):197. doi: 10.1186/s12931-021-01791-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cottin V. Idiopathic interstitial pneumonias with connective tissue diseases features: a review. Respirology. 2016;21(2):245–258. doi: 10.1111/resp.12588. [DOI] [PubMed] [Google Scholar]
- 31.Olson AL, Brown KK, Fischer A. Connective tissue disease-associated lung disease. Immunol Allergy Clin North Am. 2012;32(4):513–536. doi: 10.1016/j.iac.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Mathai SC, Danoff SK. Management of interstitial lung disease associated with connective tissue disease. BMJ. 2016;352:h6819. doi: 10.1136/bmj.h6819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fischer A, Antoniou KM, Brown KK, Cadranel J, Corte TJ, du Bois RM, et al. An official European Respiratory Society/American Thoracic Society research statement: interstitial pneumonia with autoimmune features. Eur Respir J. 2015;46(4):976–987. doi: 10.1183/13993003.00150-2015. [DOI] [PubMed] [Google Scholar]
- 34.Sánchez-Cano D, Ortego-Centeno N, Callejas JL, Fonollosa Plá V, Ríos-Fernández R, Tolosa- Vilella C, et al. Interstitial lung disease in systemic sclerosis: data from the spanish scleroderma study group. Rheumatol Int. 2018;38(3):363–374. doi: 10.1007/s00296-017-3916-x. [DOI] [PubMed] [Google Scholar]
- 35.Tashkin DP, Elashoff R, Clements PJ, Goldin J, Roth MD, Furst DE, et al. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med. 2006;354(25):2655–2666. doi: 10.1056/NEJMoa055120. [DOI] [PubMed] [Google Scholar]
- 36.Ito I, Nagai S, Kitaichi M, Nicholson AG, Johkoh T, Noma S, et al. Pulmonary manifestations of primary Sjogren's syndrome: a clinical, radiologic, and pathologic study. Am J Respir Crit Care Med. 2005;171(6):632–638. doi: 10.1164/rccm.200403-417OC. [DOI] [PubMed] [Google Scholar]
- 37.Parambil JG, Myers JL, Lindell RM, Matteson EL, Ryu JH. Interstitial lung disease in primary Sjögren syndrome. Chest. 2006;130(5):1489–1495. doi: 10.1378/chest.130.5.1489. [DOI] [PubMed] [Google Scholar]
- 38.Gao Y, Moua T. Treatment of the connective tissue disease-related interstitial lung diseases: a narrative review. Mayo Clin Proc. 2020;95(3):554–573. doi: 10.1016/j.mayocp.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 39.Dove EP, Olson AL, Glassberg MK. Trends in idiopathic pulmonary fibrosis-related mortality in the United States: 2000-2017. Am J Respir Crit Care Med. 2019;200(7):929–931. doi: 10.1164/rccm.201905-0958LE. [DOI] [PubMed] [Google Scholar]
- 40.Navaratnam V, Hubbard RB. The mortality burden of idiopathic pulmonary fibrosis in the United Kingdom. Am J Respir Crit Care Med. 2019;200(2):256–258. doi: 10.1164/rccm.201902-0467LE. [DOI] [PubMed] [Google Scholar]
- 41.Li R, Li X, Hagood J, Zhu M-S, Sun X. Myofibroblast contraction is essential for generating and regenerating the gas-exchange surface. J Clin Invest. 2020;130(6):2859–2871. doi: 10.1172/JCI132189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Young L, Adamson IY. Epithelial-fibroblast interactions in bleomycin-induced lung injury and repair. Environ Health Perspect. 1993;101(1):56–61. doi: 10.1289/ehp.9310156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bitterman PB. Pathogenesis of fibrosis in acute lung injury. Am J Med. 1992;92(6A):39S–43S. doi: 10.1016/0002-9343(92)90606-C. [DOI] [PubMed] [Google Scholar]
- 44.Klingberg F, Hinz B, White ES. The myofibroblast matrix: implications for tissue repair and fibrosis. J Pathol. 2013;229(2):298–309. doi: 10.1002/path.4104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Papiris SA, Tomos IP, Karakatsani A, Spathis A, Korbila I, Analitis A, et al. High levels of IL-6 and IL-8 characterize early-on idiopathic pulmonary fibrosis acute exacerbations. Cytokine. 2018;102:168–172. doi: 10.1016/j.cyto.2017.08.019. [DOI] [PubMed] [Google Scholar]
- 46.Zhao H, Li C, Li L, Liu J, Gao Y, Mu K, et al. Baicalin alleviates bleomycin-induced pulmonary fibrosis and fibroblast proliferation in rats via the PI3K/AKT signaling pathway. Mol Med Rep. 2020;21(6):2321–2334. doi: 10.3892/mmr.2020.11046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu S-S, Liu C, Lv X-X, Cui B, Yan J, Li Y-X, et al. The chemokine CCL1 triggers an AMFR-SPRY1 pathway that promotes differentiation of lung fibroblasts into myofibroblasts and drives pulmonary fibrosis. Immunity. 2021;54(9):2042–2056.e8. doi: 10.1016/j.immuni.2021.06.008. [DOI] [PubMed] [Google Scholar]
- 48.Hu X, Xu Q, Wan H, Hu Y, Xing S, Yang H, et al. PI3K-Akt-mTOR/PFKFB3 pathway mediated lung fibroblast aerobic glycolysis and collagen synthesis in lipopolysaccharide-induced pulmonary fibrosis. Lab Invest. 2020;100(6):801–811. doi: 10.1038/s41374-020-0404-9. [DOI] [PubMed] [Google Scholar]
- 49.Zhang J, Wang D, Wang L, Wang S, Roden AC, Zhao H, et al. Profibrotic effect of IL-17A and elevated IL-17RA in idiopathic pulmonary fibrosis and rheumatoid arthritis-associated lung disease support a direct role for IL-17A/IL-17RA in human fibrotic interstitial lung disease. Am J Physiol Lung Cell Mol Physiol. 2019;316(3):L487–L497. doi: 10.1152/ajplung.00301.2018. [DOI] [PubMed] [Google Scholar]
- 50.Zhang S, Jia X, Zhang Q, Zhang L, Yang J, Hu C, et al. Neutrophil extracellular traps activate lung fibroblast to induce polymyositis-related interstitial lung diseases via TLR9-miR-7-Smad2 pathway. J Cell Mol Med. 2020;24(2):1658–1669. doi: 10.1111/jcmm.14858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chrysanthopoulou A, Mitroulis I, Apostolidou E, Arelaki S, Mikroulis D, Konstantinidis T, et al. Neutrophil extracellular traps promote differentiation and function of fibroblasts. J Pathol. 2014;233(3):294–307. doi: 10.1002/path.4359. [DOI] [PubMed] [Google Scholar]
- 52.Frangou E, Chrysanthopoulou A, Mitsios A, Kambas K, Arelaki S, Angelidou I, Arampatzioglou A, Gakiopoulou H, Bertsias GK, Verginis P, et al. REDD1/autophagy pathway promotes thromboinflammation and fibrosis in human systemic lupus erythematosus (SLE) through NETs decorated with tissue factor (TF) and interleukin-17A (IL-17A) Ann Rheum Dis. 2019;78(2):238–248. doi: 10.1136/annrheumdis-2018-213181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Suzuki M, Ikari J, Anazawa R, Tanaka N, Katsumata Y, Shimada A, et al. PAD4 deficiency improves bleomycin-induced neutrophil extracellular traps and fibrosis in mouse lung. Am J Respir Cell Mol Biol. 2020;63(6):806–818. doi: 10.1165/rcmb.2019-0433OC. [DOI] [PubMed] [Google Scholar]
- 54.Königshoff M, Bonniaud P. Live and let die: targeting alveolar epithelial cell proliferation in pulmonary fibrosis. Am J Respir Crit Care Med. 2014;190(12):1339–1341. doi: 10.1164/rccm.201411-2030ED. [DOI] [PubMed] [Google Scholar]
- 55.Zhang C, Zhu X, Hua Y, Zhao Q, Wang K, Zhen L, et al. YY1 mediates TGF-β1-induced EMT and pro-fibrogenesis in alveolar epithelial cells. Respir Res. 2019;20(1):249. doi: 10.1186/s12931-019-1223-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lehmann M, Hu Q, Hu Y, Hafner K, Costa R, van den Berg A, et al. Chronic WNT/β-catenin signaling induces cellular senescence in lung epithelial cells. Cell Signal. 2020;70:109588. doi: 10.1016/j.cellsig.2020.109588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Selman M, Pardo A. Idiopathic pulmonary fibrosis: an epithelial/fibroblastic cross-talk disorder. Respir Res. 2002;3(1):3. doi: 10.1186/rr175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wuyts WA, Agostini C, Antoniou KM, Bouros D, Chambers RC, Cottin V, et al. The pathogenesis of pulmonary fibrosis: a moving target. Eur Respir J. 2013;41(5):1207–1218. doi: 10.1183/09031936.00073012. [DOI] [PubMed] [Google Scholar]
- 59.Corrin B, Dewar A, Rodriguez-Roisin R, Turner-Warwick M. Fine structural changes in cryptogenic fibrosing alveolitis and asbestosis. J Pathol. 1985;147(2):107–119. doi: 10.1002/path.1711470206. [DOI] [PubMed] [Google Scholar]
- 60.Myers JL, Katzenstein AL. Epithelial necrosis and alveolar collapse in the pathogenesis of usual interstitial pneumonia. Chest. 1988;94(6):1309–1311. doi: 10.1378/chest.94.6.1309. [DOI] [PubMed] [Google Scholar]
- 61.Korfei M, Ruppert C, Mahavadi P, Henneke I, Markart P, Koch M, et al. Epithelial endoplasmic reticulum stress and apoptosis in sporadic idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2008;178(8):838–846. doi: 10.1164/rccm.200802-313OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barbas-Filho JV, Ferreira MA, Sesso A, Kairalla RA, Carvalho CR, Capelozzi VL. Evidence of type II pneumocyte apoptosis in the pathogenesis of idiopathic pulmonary fibrosis (IFP)/usual interstitial pneumonia (UIP) J Clin Pathol. 2001;54(2):132–138. doi: 10.1136/jcp.54.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saffarzadeh M, Juenemann C, Queisser MA, Lochnit G, Barreto G, Galuska SP, et al. Neutrophil extracellular traps directly induce epithelial and endothelial cell death: a predominant role of histones. PLoS One. 2012;7(2):e32366. doi: 10.1371/journal.pone.0032366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xu J, Zhang X, Pelayo R, Monestier M, Ammollo CT, Semeraro F, et al. Extracellular histones are major mediators of death in sepsis. Nat Med. 2009;15(11):1318–1321. doi: 10.1038/nm.2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Narasaraju T, Yang E, Samy RP, Ng HH, Poh WP, Liew A-A, et al. Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. Am J Pathol. 2011;179(1):199–210. doi: 10.1016/j.ajpath.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lachowicz-Scroggins ME, Dunican EM, Charbit AR, Raymond W, Looney MR, Peters MC, et al. Extracellular DNA, neutrophil extracellular traps, and inflammasome activation in severe asthma. Am J Respir Crit Care Med. 2019;199(9):1076–1085. doi: 10.1164/rccm.201810-1869OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang H, Liu J, Zhou Y, Qu M, Wang Y, Guo K, et al. Neutrophil extracellular traps mediate mA modification and regulates sepsis-associated acute lung injury by activating ferroptosis in alveolar epithelial cells. Int J Biol Sci. 2022;18(8):3337–3357. doi: 10.7150/ijbs.69141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pandolfi L, Bozzini S, Frangipane V, Percivalle E, De Luigi A, Violatto MB, et al. Neutrophil extracellular traps induce the epithelial-mesenchymal transition: implications in post-COVID-19 fibrosis. Front Immunol. 2021;12:663303. doi: 10.3389/fimmu.2021.663303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Martins-Cardoso K, Almeida VH, Bagri KM, Rossi MID, Mermelstein CS, König S, et al. Neutrophil extracellular traps (NETs) promote pro-metastatic phenotype in human breast cancer cells through epithelial-mesenchymal transition. Cancers (Basel) 2020;12(6):1542. doi: 10.3390/cancers12061542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhu T, Zou X, Yang C, Li L, Wang B, Li R, et al. Neutrophil extracellular traps promote gastric cancer metastasis by inducing epithelial-mesenchymal transition. Int J Mol Med. 2021;48(1):127. doi: 10.3892/ijmm.2021.4960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stehr AM, Wang G, Demmler R, Stemmler MP, Krug J, Tripal P, et al. Neutrophil extracellular traps drive epithelial-mesenchymal transition of human colon cancer. J Pathol. 2022;256(4):455–467. doi: 10.1002/path.5860. [DOI] [PubMed] [Google Scholar]
- 72.Jahreis S, Trump S, Bauer M, Bauer T, Thürmann L, Feltens R, et al. Maternal phthalate exposure promotes allergic airway inflammation over 2 generations through epigenetic modifications. J Allergy Clin Immunol. 2018;141(2):741–753. doi: 10.1016/j.jaci.2017.03.017. [DOI] [PubMed] [Google Scholar]
- 73.Fernandez IE, Eickelberg O. New cellular and molecular mechanisms of lung injury and fibrosis in idiopathic pulmonary fibrosis. Lancet. 2012;380(9842):680–688. doi: 10.1016/S0140-6736(12)61144-1. [DOI] [PubMed] [Google Scholar]
- 74.Wang W, Liu Z, Zhang Y, Wang L, Meng D, Li X, et al. Benzyl butyl phthalate (BBP) induces lung injury and fibrosis through neutrophil extracellular traps. Environ Pollut. 2022;309:119743. doi: 10.1016/j.envpol.2022.119743. [DOI] [PubMed] [Google Scholar]
- 75.Agostini C, Gurrieri C. Chemokine/cytokine cocktail in idiopathic pulmonary fibrosis. Proc Am Thorac Soc. 2006;3(4):357–363. doi: 10.1513/pats.200601-010TK. [DOI] [PubMed] [Google Scholar]
- 76.Miyazaki Y, Araki K, Vesin C, Garcia I, Kapanci Y, Whitsett JA, et al. Expression of a tumor necrosis factor-alpha transgene in murine lung causes lymphocytic and fibrosing alveolitis. A mouse model of progressive pulmonary fibrosis. J Clin Invest. 1995;96(1):250–259. doi: 10.1172/JCI118029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Khalil N, Xu YD, O'Connor R, Duronio V. Proliferation of pulmonary interstitial fibroblasts is mediated by transforming growth factor-beta1-induced release of extracellular fibroblast growth factor-2 and phosphorylation of p38 MAPK and JNK. J Biol Chem. 2005;280(52):43000–43009. doi: 10.1074/jbc.M510441200. [DOI] [PubMed] [Google Scholar]
- 78.Ruiz V, Ordóñez RM, Berumen J, Ramírez R, Uhal B, Becerril C, et al. Unbalanced collagenases/TIMP-1 expression and epithelial apoptosis in experimental lung fibrosis. Am J Physiol Lung Cell Mol Physiol. 2003;285(5):L1026–L1036. doi: 10.1152/ajplung.00183.2003. [DOI] [PubMed] [Google Scholar]
- 79.Gregory AD, Kliment CR, Metz HE, Kim K-H, Kargl J, Agostini BA, et al. Neutrophil elastase promotes myofibroblast differentiation in lung fibrosis. J Leukoc Biol. 2015;98(2):143–152. doi: 10.1189/jlb.3HI1014-493R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xia X, Zhang Z, Zhu C, Ni B, Wang S, Yang S, et al. Neutrophil extracellular traps promote metastasis in gastric cancer patients with postoperative abdominal infectious complications. Nat Commun. 2022;13(1):1017. doi: 10.1038/s41467-022-28492-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bosmann M, Ward PA. Protein-based therapies for acute lung injury: targeting neutrophil extracellular traps. Expert Opin Ther Targets. 2014;18(6):703–714. doi: 10.1517/14728222.2014.902938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sabbione F, Keitelman IA, Iula L, Ferrero M, Giordano MN, Baldi P, et al. Neutrophil extracellular traps stimulate proinflammatory responses in human airway epithelial cells. J Innate Immun. 2017;9(4):387–402. doi: 10.1159/000460293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Urbonaviciute V, Voll RE. High-mobility group box 1 represents a potential marker of disease activity and novel therapeutic target in systemic lupus erythematosus. J Intern Med. 2011;270(4):309–318. doi: 10.1111/j.1365-2796.2011.02432.x. [DOI] [PubMed] [Google Scholar]
- 84.Andersson U, Tracey KJ. HMGB1 is a therapeutic target for sterile inflammation and infection. Annu Rev Immunol. 2011;29:139–162. doi: 10.1146/annurev-immunol-030409-101323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.He M, Kubo H, Ishizawa K, Hegab AE, Yamamoto Y, Yamamoto H, et al. The role of the receptor for advanced glycation end-products in lung fibrosis. Am J Physiol Lung Cell Mol Physiol. 2007;293(6):L1427–L1436. doi: 10.1152/ajplung.00075.2007. [DOI] [PubMed] [Google Scholar]
- 86.Katsuoka F, Kawakami Y, Arai T, Imuta H, Fujiwara M, Kanma H, et al. Type II alveolar epithelial cells in lung express receptor for advanced glycation end products (RAGE) gene. Biochem Biophys Res Commun. 1997;238(2):512–516. doi: 10.1006/bbrc.1997.7263. [DOI] [PubMed] [Google Scholar]
- 87.Miossec P, Kolls JK. Targeting IL-17 and TH17 cells in chronic inflammation. Nat Rev Drug Discov. 2012;11(10):763–776. doi: 10.1038/nrd3794. [DOI] [PubMed] [Google Scholar]
- 88.Hudock KM, Collins MS, Imbrogno M, Snowball J, Kramer EL, Brewington JJ, et al. Neutrophil extracellular traps activate IL-8 and IL-1 expression in human bronchial epithelia. Am J Physiol Lung Cell Mol Physiol. 2020;319(1):L137–L147. doi: 10.1152/ajplung.00144.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Miranda FJB, Rocha BC, Pereira MCA, Pereira LMN, de Souza EHM, Marino AP, et al. Toxoplasma gondii-induced neutrophil extracellular traps amplify the innate and adaptive response. mBio. 2021;12(5):e0130721. doi: 10.1128/mBio.01307-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chirivi RGS, van Rosmalen JWG, van der Linden M, Euler M, Schmets G, Bogatkevich G, et al. Therapeutic ACPA inhibits NET formation: a potential therapy for neutrophil-mediated inflammatory diseases. Cell Mol Immunol. 2021;18(6):1528–1544. doi: 10.1038/s41423-020-0381-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mizushima N, Komatsu M. Autophagy: renovation of cells and tissues. Cell. 2011;147(4):728–741. doi: 10.1016/j.cell.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 92.Levine B, Kroemer G. Biological functions of autophagy genes: a disease perspective. Cell. 2019;176(1–2):11–42. doi: 10.1016/j.cell.2018.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Remijsen Q, Vanden Berghe T, Wirawan E, Asselbergh B, Parthoens E, De Rycke R, et al. Neutrophil extracellular trap cell death requires both autophagy and superoxide generation. Cell Res. 2011;21(2):290–304. doi: 10.1038/cr.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Boone BA, Murthy P, Miller-Ocuin J, Doerfler WR, Ellis JT, Liang X, et al. Chloroquine reduces hypercoagulability in pancreatic cancer through inhibition of neutrophil extracellular traps. BMC Cancer. 2018;18(1):678. doi: 10.1186/s12885-018-4584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gui Y-S, Wang L, Tian X, Li X, Ma A, Zhou W, et al. mTOR Overactivation and compromised autophagy in the pathogenesis of pulmonary fibrosis. PLoS One. 2015;10(9):e0138625. doi: 10.1371/journal.pone.0138625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Abdel Fattah E, Bhattacharya A, Herron A, Safdar Z, Eissa NT. Critical role for IL-18 in spontaneous lung inflammation caused by autophagy deficiency. J Immunol. 2015;194(11):5407–5416. doi: 10.4049/jimmunol.1402277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nho RS, Hergert P. IPF fibroblasts are desensitized to type I collagen matrix-induced cell death by suppressing low autophagy via aberrant Akt/mTOR kinases. PLoS One. 2014;9(4):e94616. doi: 10.1371/journal.pone.0094616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jessop F, Hamilton RF, Rhoderick JF, Shaw PK, Holian A. Autophagy deficiency in macrophages enhances NLRP3 inflammasome activity and chronic lung disease following silica exposure. Toxicol Appl Pharmacol. 2016;309:101–110. doi: 10.1016/j.taap.2016.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Liu M-W, Su M-X, Tang D-Y, Hao L, Xun X-H, Huang Y-Q. Ligustrazin increases lung cell autophagy and ameliorates paraquat-induced pulmonary fibrosis by inhibiting PI3K/Akt/mTOR and hedgehog signalling via increasing miR-193a expression. BMC Pulm Med. 2019;19(1):35. doi: 10.1186/s12890-019-0799-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang Y, Shen L, Zhu H, Dreissigacker K, Distler D, Zhou X, et al. PGC-1α regulates autophagy to promote fibroblast activation and tissue fibrosis. Ann Rheum Dis. 2020;79(9):1227–1233. doi: 10.1136/annrheumdis-2020-216963. [DOI] [PubMed] [Google Scholar]
- 101.Zehender A, Li Y-N, Lin N-Y, Stefanica A, Nüchel J, Chen C-W, et al. TGFβ promotes fibrosis by MYST1-dependent epigenetic regulation of autophagy. Nat Commun. 2021;12(1):4404. doi: 10.1038/s41467-021-24601-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Angelidou I, Chrysanthopoulou A, Mitsios A, Arelaki S, Arampatzioglou A, Kambas K, et al. REDD1/autophagy pathway is associated with neutrophil-driven IL-1β inflammatory response in active ulcerative colitis. J Immunol. 2018;200(12):3950–3961. doi: 10.4049/jimmunol.1701643. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.