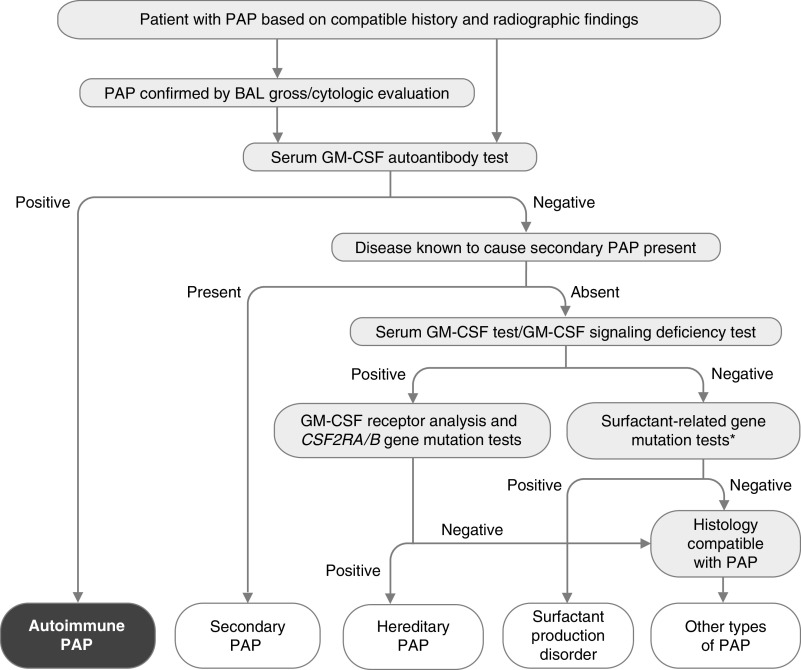
Figure 5.
Algorithm for diagnosis of pulmonary alveolar proteinosis (PAP). PAP is suspected on the basis of history and radiographic findings and can be confirmed by the gross and microscopic appearance of BAL fluid. A serum GM-CSF (granulocyte/macrophage colony–stimulating factor) autoantibody test is performed and is highly sensitive and specific for diagnosis of autoimmune PAP. Secondary PAP is diagnosed in individuals with a negative test result who have a condition known to cause PAP. Those with negative test results and no known PAP-causing disease should undergo blood GM-CSF signaling testing and serum GM-CSF testing to identify hereditary PAP caused by CSF2RA or CSF2RB gene mutations, followed by appropriate confirmatory genetic testing. Patients with normal concentrations of serum GM-CSF (e.g., low/undetectable) and normal GM-CSF signaling test results (e.g., detectable) should undergo genetic testing used to identify surfactant production disorders (also known as congenital PAP), including mutational analysis of SFTPC, SFTPB, ABCA3, and NKX2.1 (*). A transbronchial or surgical lung biopsy may be needed if all test results are negative, and further genetic testing may be needed to identify other ultrarare PAP-causing diseases (i.e., methionine-transfer RNA mutations [235], lysinuric protein intolerance [236], or lymphoid cell deficiency–related PAP [237]) Adapted from Reference 4.