Figure 9.
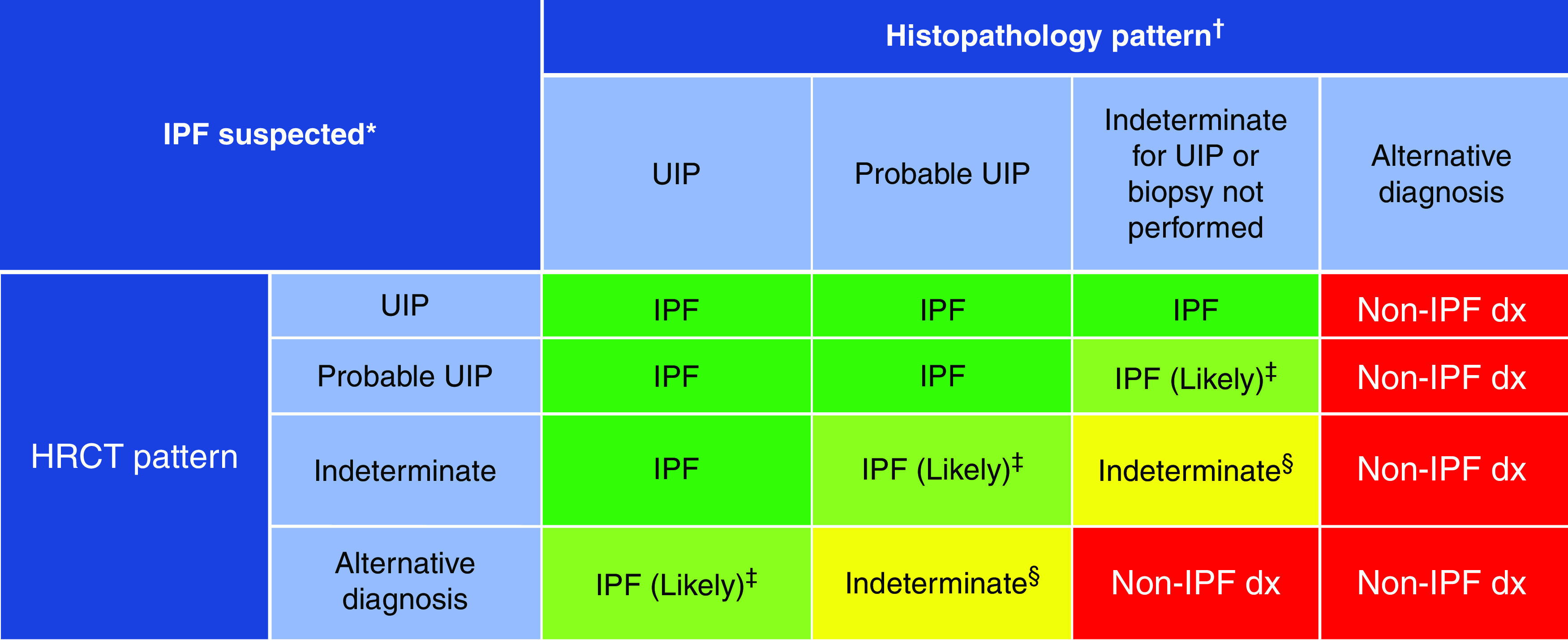
Idiopathic pulmonary fibrosis (IPF) diagnosis on the basis of high-resolution computed tomography (HRCT) and biopsy patterns, developed using consensus by discussion. *“Clinically suspected of having IPF” is defined as unexplained patterns of bilateral pulmonary fibrosis on chest radiography or chest computed tomography, bibasilar inspiratory crackles, and age > 60 years. Middle-aged adults (>40 and <60 yr old) can rarely present with otherwise similar clinical features, especially in patients with features suggesting familial pulmonary fibrosis. †Diagnostic confidence may need to be downgraded if histopathological assessment is based on transbronchial lung cryobiopsy given the smaller biopsy size and greater potential for sampling error compared with surgical lung biopsy. ‡IPF is the likely diagnosis when any of the following features are present: 1) moderate to severe traction bronchiectasis and/or bronchiolectasis (defined as mild traction bronchiectasis and/or bronchiolectasis in four or more lobes, including the lingula as a lobe, or moderate to severe traction bronchiectasis in two or more lobes) in a man >50 years old or in a woman >60 yr old, 2) extensive (>30%) reticulation on HRCT and age > 70 yr, 3) increased neutrophils and/or absence of lymphocytosis in BAL fluid, and 4) multidisciplinary discussion produces a confident diagnosis of IPF. §Indeterminate for IPF 1) without an adequate biopsy remains indeterminate and 2) with an adequate biopsy may be reclassified to a more specific diagnosis after multidisciplinary discussion and/or additional consultation. Adapted from Reference 2. dx = diagnosis; UIP = usual interstitial pneumonia.
