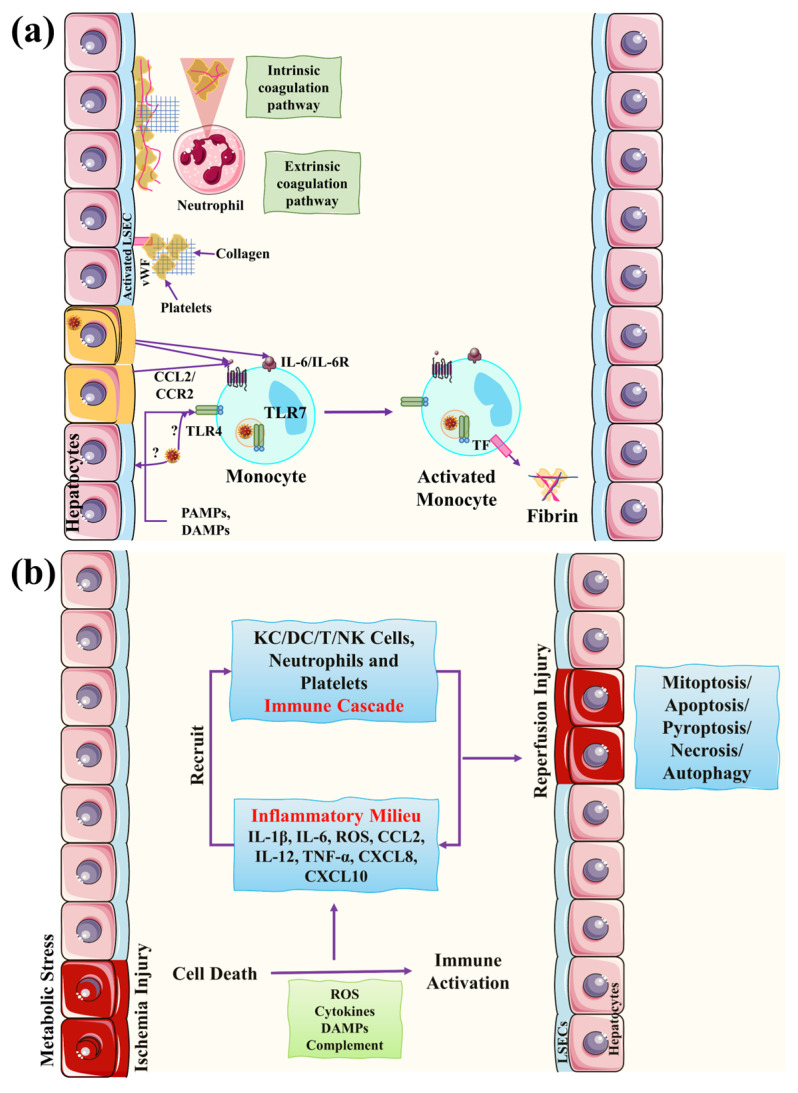
Figure 4.
COVID-19-associated liver damage mechanisms of impaired coagulation and hepatic ischemia/hypoxia reperfusion injury. (a) In those with severe COVID-19 and hepatic impairment, coagulation problems have been associated with negative results. Monocytes are drawn to endothelial cells in response to proinflammatory stimuli and create tissue factors (TFs), which activate an extrinsic coagulation pathway, resulting in fibrin deposition and blood clotting. Neutrophils are attracted to infection sites early and create neutrophil extracellular traps (NETs), which start a chain reaction of inflammatory responses and activate the contact coagulation pathway, binding and activating platelets to enhance blood clotting. (b) Hepatic ischemia/hypoxia reperfusion damage occurs in two stages: ischemia-induced cell injury and reperfusion-induced inflammatory response. Ischemic injury, which is a localized process of cellular metabolic anomalies, initiates hepatocyte cell death. Reperfusion damage, which occurs following ischemia injury, is produced by metabolic anomalies and a strong inflammatory, immunological response that includes both direct and indirect cytotoxic pathways. This figure is reproduced from Li et al. [26] after permission from Springer Nature (license no. 5445930573563).