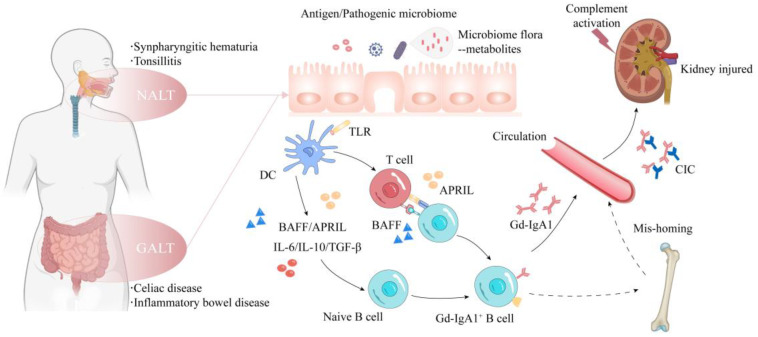
Figure 1.
The pathophysiology of IgAN. IgAN usually presents with episodic gross hematuria and a concurrent upper respiratory tract infection or gastrointestinal disorder. Individuals with genetic susceptibility to IgAN develop aberrant mucosal immune responses to persistent antigenic stimulus, pathogenic microbiota and microbial metabolites. Antigen-presenting cells thereby activate and facilitate B-cells undergoing class switch and then differentiate into IgA+ ASCs in T-cell-dependent or T-cell-independent manners. Some mistrafficking ASCs take up residence in systemic sites, such as the bone marrow, NALT and GALT, leading to an increased circulating level of Gd-IgA1 and thus resulting in immune complex formation. The Gd-IgA1-containing immune complexes deposit in glomerular mesangium. Subsequently, complement activation (the alternative, lectin and terminal pathway) and intraglomerular inflammation together synergistically lead to kidney injuries, such as mesangial hypercellularity and fibrosis. ASC, antibody-secreting cell; CIC, circulating immune complex; DC, dendritic cell; NALT, nasal-associated lymphoid tissue; GALT, gut-associated lymphoid tissue; IgAN, IgA nephropathy.