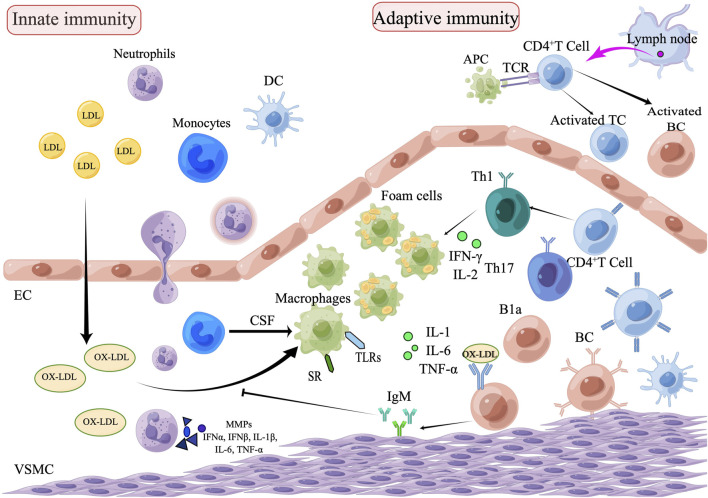
FIGURE 1.
The role of innate and adaptive immunity in the development of atherosclerosis. The process of atherosclerosis is brought on by the buildup of heat shock proteins and modified ox-LDL in the intima of the arterial wall, which is exacerbated by the invasion of innate immune cells such as monocytes, eosinophils, and neutrophils. Monocytes are transformed into macrophages, which remove ox-LDL by binding to scavenger receptors and are further transformed into foam cells. Subsequently, adaptive immune cells, including Th1and Th17, enter the plaque lesion and produce inflammatory cytokines (IL-1, IL-6, and TNF-α) which exacerbate the pathophysiology of atherosclerosis. APCs arrive via lymphatic vessels to present homologous peptides on MHC molecules to naive T cells, which attract adaptive T cell and B cell responses. B1a cells can be stimulated by IL-5 to produce oxygen LDL-specific natural IgM antibodies, which block oxygen LDL absorption and production of foam cells, thus achieving an anti-atherosclerotic effect. Natural IgM has also been demonstrated to facilitate the clearance of apoptotic cells (EC, endothelial cells; VSMC, vascular smooth muscle cell; DC, dendritic cell; TC, T lymphocytes; BC, B lymphocytes; SR, scavenger receptor; B1a, B1a lymphocytes; CSF, colony stimulating factors; APCs, Antigen-presenting cells).