Abstract
Background
Postoperative adverse events (AEs) following pulmonary resection enormously impact patient well-being, length of stay (LOS) and healthcare costs. Standardised AE data collection can be used to identify positive outliers demonstrating positive deviance (PD) who may be helpful to inform the best practice. Here, we describe our initial experience of a novel quality improvement process using PD to reduce LOS and AEs.
Methods
AE rates and LOS were collected from four centres (2014–2020) using a common dictionary. Surgeons repeatedly participated in 60 to 90 min seminars consisting of the following process: identify outcome and procedure targeted, review relevant best evidence literature, view all data anonymised by surgeon or centre (if multicentre), choose and reveal identity of best performance PD outliers, who discuss their management principles while all receive self-evaluation reports, followed by collegial discussion to generate consensus recommendations, voted by all. We assessed overall impact on AEs and LOS using aggregate data in a before/after analysis.
Results
A total of 131 surgeons (average 12/seminar) participated in 11 PD seminars (8 local and 3 multicentre), yielding 85 consensus recommendation (average 8/seminar). Median LOS following lobectomy decreased from 4.0 to 3.0 days (p=0.04) following local PD seminars and from 4.0 to 3.5 days (p=0.11) following multicentre seminars. Trends for reductions in multiple AE rates were also observed.
Conclusion
While limited by the longitudinal design, these findings provide preliminary support for this data-driven, collegial and actionable quality improvement process to help standardise and improve patient care, and merits further more rigorous investigation.
Keywords: Adverse events, epidemiology and detection; Continuous quality improvement; Quality improvement methodologies; Surgery; Postoperative Care
WHAT IS ALREADY KNOWN ON THIS TOPIC.
We have previously studied the effect of implementing positive deviance seminars in individual thoracic surgery centres, demonstrating a 34% reduction in atrial fibrillation rates, 38% reduction in prolonged air leak rates and 25% reduction in anastomotic leak rates following non-cardiac thoracic surgery.
WHAT THIS STUDY ADDS
To the best of our knowledge, this is the first study to implement positive deviance seminars as a quality improvement initiative on a national, multicentre level across thoracic surgery institutions. This study provides an encouraging first look at the impact of this initiative on the multicentre level to reduce postoperative adverse events and length of stay.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Our study presents encouraging evidence that implementing this continuous quality improvement initiative on a wider scale can help to standardise and improve practice with evidence-based formulation of practice recommendations.
Introduction
Postoperative adverse events (AEs) can have a profound detrimental impact on patient recovery after surgery. Consequences include an augmented risk of mortality,1 2 impaired postoperative recovery,3 increased length of stay (LOS),3–5 and negative patient experience.6 7 Expenses related to AE treatment strain already burdened hospital systems, raising healthcare costs by US$4000–US$44 000 per instance of a complication depending on the corrective action required.4 8 9 Though AEs are prevalent in many surgical disciplines, patients requiring thoracic surgery are at especially high risk due to the disease process, vital nature of chest anatomy and patient comorbidities. While some AEs inevitably occur, 37%–51% of all reported AEs are potentially preventable and cost the Canadian healthcare system US$397 million/year.9–11 Practice variation is known to contribute towards high rates of preventable AEs. Thus, thoracic surgeons have been leaders in creating internationally harmonised AE definitions in order to facilitate multicentre data collection.12–22
The concept of positive deviance (PD) is derived from the observation that in any community or profession, there exist individuals whose uncommon behaviours and strategies allow them to find better solutions to problems than their peers. Such individuals are considered to exhibit PD. PD seminars have previously been studied in medicine demonstrating meaningful improvements in patient care.23 24 We have previously reported a single-centre experience using PD seminars in thoracic surgery focusing on atrial fibrillation (AFIB), prolonged air leak (PAL) and anastomotic leak (AL) following non-cardiac thoracic surgery, demonstrating 34% reduction in AFIB rates, 38% reduction in PAL rates and 25% reduction in AL rates.25 26 In this study, surgeons supported the team-building and constructive nature of the seminars.25 26
Following the footsteps of international thoracic surgery associations to standardise practice and reduce AEs in thoracic surgery, the Canadian Association of Thoracic Surgeons has initiated a programme of data-informed audit and feedback (A&F) coupled to identifying best evidence (ie, literature review) and best experience (ie, PD) to inform quality improvement seminars. The culmination of this process leads to the creation of actionable consensus recommendations. This study will report the initial experience of eight local PD seminars performed with all surgeons at a single-centre and the first three multicentre PD seminars. The objective of this study was to quantify the initial experience of both single-centre and multiinstitutional quality improvement seminars on the rates of PAL, AFIB and duration of LOS following non-cardiac thoracic surgery across sites.
Methods
Outcome definitions
First, the incidence and severity of postoperative AEs were collected prospectively for patients using the Thoracic Morbidity and Mortality system (see ottawatmm.org), based on the Clavien-Dindo schema.17 18 Specifically, AFIB was defined as new onset of AFIB/flutter requiring treatment or cardioversion, but excludes recurrence if it was a condition known preoperatively. PAL was defined as an air leak originating from a tear or discontinuity of the visceral pleura lasting >5 days (ie, air leak present on postoperative day (POD) 6 or present at the time of discharge from hospital with planned follow-up on or after POD 6). The grade for the severity of each AE is included in online supplemental table 1. LOS was defined as the number of days the patients was in hospital after index surgery. Days after readmission are not included but recorded.
bmjoq-2022-001997supp001.pdf (74.3KB, pdf)
PD seminars
Local
As outlined in online supplemental figure 1, the process of a seminar at the local site starts with the shared commitment to reduce an AE/outcome for a particular procedure. Then, a review of best evidence is performed, reviewing relevant trials and recommendations (10–15 min presentation performed didactically) to situate all participants. Next, data are viewed including raw and risk adjusted data by anonymously reported by surgeons. The group selects the surgeons demonstrating PD, who are subsequently identified. The identified ‘best performers’ are asked to share the techniques/practices they believe have led to their superior outcomes. During this discussion, surgeons are emailed their personalised report to know their own results. Using literature and data as catalysts, the group is tasked with collectively, collegially creating consensus recommendations that combine best evidence and experience in order to reduce the AE in question.19 20 The process of generating consensus recommendations involves suggested recommendations, followed by group discussion. The chair of the seminar invites and/or offers suggestions for consensus recommendations, and then evokes responses from the group, including approval, disapproval or altered wording of the recommendation. When a consensus approval is reached without further edits being required, the recommendation is recorded. This process is repeated until all recommendations have been recorded and the group agrees that no new recommendations are forthcoming. Finally, all recommendations are reviewed once again and voted on independently using a live, online voting tool (MentiMeter) to anonymously record the level of agreement with each recommendation. The process for the entire PD seminar spans 60–90 min, with roughly 30–40 min being used to generate recommendations and 5 min for voting.
bmjoq-2022-001997supp002.pdf (727.3KB, pdf)
Multicentre
The process of a multicentre seminar has the same flow, but sites rather than surgeons are identified as demonstrating PD. A representative for the ‘best performers’ is asked to share both technical and institutional practices they believe improve outcomes. As with local seminars, at the end of the seminar, physicians are asked to anonymously rank their agreement with recommendations and subsequently implement the changes in their practice.
Study design
The primary outcomes are the incidence of AFIB, PAL and LOS after pulmonary resection. Data were collected from four Canadian academic thoracic surgery centres.
A retrospective uncontrolled before/after analysis was performed to evaluate AE rates and LOS preintervention and postintervention. Data were collected on a month-by-month basis for three procedures: lobectomy, segmentectomy and wedge resection. A preintervention range was determined for each site and used as a baseline for LOS and AE rates. Conversely, a postintervention range following the seminar was determined with data assumed to reflect the impact of the intervention. The total range of included data can be found in online supplemental table 2.
For local analyses, individual LOS entries falling within the preintervention and postintervention ranges (based on the corresponding seminar dates specific to each centre) were collected from each centre to form a total multicentre collection of LOS entries. These entries were analysed on a month-by-month basis to form monthly median LOS values representing data from all centres. Additionally, a singular median for the preintervention range as well as one for the postintervention range were calculated to derive a before/after metric. A similar process was followed for the AE analyses, except that monthly rates were calculated as a percentage by dividing the total incidence of the AE across the centres by the total number of procedures performed during the month. For the before/after metric, mean rates were calculated from the monthly rates.
For multicentre analyses, the same process was used. Here, however, the dates of preintervention and postintervention ranges remained consistent as all centres participated in the same multicentre seminars.
A standard preintervention period of 12 months and postintervention period of 6 months were used. We noted a marked impact of the first wave of COVID-19 on surgical volume in all centres simultaneously (March to May 2020), with a reduction in surgical volume of over 30% for these months. Due to altered case selection and decreased volume, these 3 months were removed a priori from the multicente PD seminar analyses. The preintervention and postintervention ranges for local LOS analyses remained as 12 and 6 months, respectively.
Statistical analyses
For LOS analyses, unpaired, two-sided Mann-Whitney tests were performed to compare the preintervention and postintervention medians. For AEs, unpaired, two-sided t-tests were performed to compare the preintervention and postintervention means. Statistical significance for both were set to p≤0.05. All statistical tests were performed using GraphPad Prism (GraphPad Software, San Diego, California, USA).
Patients and public involvement
Patients and public were not involved.
Results
Local seminars
The local seminars included yielded a total of 65 consensus recommendations (average 8/seminar) across the 3 topics (LOS, PAL and AFIB). A total of 50 surgeons attended (average 6/seminar), and all seminars culminated in recommendations (table 1).
Table 1.
Summary of surgeon attendance and number of recommendations resulting from PD seminars
| Topic | Date and site(s)† (dd-mm-yyyy) |
Total participant surgeons | Total no of recommendations |
| Local Seminars | |||
| LOS* | 28-01-2020—TOH | 5 | 15 |
| 13-03-2020—MUHC | 8 | 14 | |
| 04-03-2020—SJHH | 4 | 11 | |
| Mean | 5.67 | 13.3 | |
| PAL | 06-02-2015—TOH | 6 | 2 |
| 29-03-2019—MUHC | 8 | 3 | |
| 16-11-2018—UHN | 9 | 5 | |
| 19-02-2019—SJHH | 4 | 13 | |
| Mean | 6.75 | 5.75 | |
| AFIB | 06-02-2015—TOH | 6 | 2 |
| Multicentre seminars | |||
| LOS* | 17-04-2020—TOH, MUHC, SJHH | 21 | 17 |
| PAL | 05-09-2019—TOH, MUHC, UHN, SJHH | 30 | 1 |
| AFIB | 28-08-2019—TOH, MUHC, UHN, SJHH | 30 | 2 |
*Indicates that LOS seminars were used for analyses of both lobectomy as well as all pulmonary resections.
†TOH: The Ottawa Hospital; MUHC: McGill University Health Centre; UHN: University Health Network; SJHH: St. Joseph’s Healthcare Hamilton.
AFIB, atrial fibrillation; LOS, length of stay; PAL, prolonged air leak.
Table 2 provides the primary outcomes. Median LOS for lobectomy decreased from 4.0 to 3.0 days (p=0.04) while median LOS for all procedures remained at 3.0 days (figure 1). PAL rates decreased from 11.6% to 10.8% (p=0.62), and a subanalysis revealed that major PAL decreased from 2.2% to 1.9% (p=0.71) while minor PAL decreased from 9.4% to 8.9% (p=0.74) (figure 2). Finally, major AFIB rates remained at 0% preintervention and postintervention, so minor AFIB consequently accounted for the entirety of the AFIB rates, decreasing from 6.0% to 3.3% (p=0.31) (figure 2).
Table 2.
Summary of postoperative LOS and AE rates preintervention and postintervention
| Topic | Comparison | Preintervention | Postintervention | P value |
| Local seminars | ||||
| LOS: lobectomy | Median: 12 mo pre vs 6 mo post | 4.0 (IQR=2.0–7.0) | 3.0 (IQR=2.0–5.0) | 0.04* |
| LOS: all pulmonary resections | Median: 12 mo pre vs 6 mo post | 3.0 (IQR=1.0–5.0) | 3.0 (IQR=2.0–5.0) | n/a |
| PAL | Mean: 12 mo pre vs 6 mo post | 11.6 (SEM = ±0.8) | 10.8 (SEM = ±1.6) | 0.62 |
| AFIB | Mean: 12 mo pre vs 6 mo post | 6.0 (SEM = ±1.7) | 3.3 (SEM = ±1.0) | 0.31 |
| Multicentre seminars | ||||
| LOS: lobectomy | Median: 10 mo pre vs 5 mo post | 4.0 (IQR=2.0–7.0) | 3.5 (IQR=2.0–5.0) | 0.11 |
| LOS: all pulmonary resections | Median: 10 mo pre vs 5 mo post | 3.0 (IQR=1.0–5.0) | 3.0 (IQR=2.0–5.0) | n/a |
| PAL | Mean: 12 mo pre vs 6 mo post | 10.2 (SEM = ±1.1) | 9.8 (SEM = ±1.4) | 0.83 |
| AFIB | Mean: 12 mo pre vs 6 mo post | 4.1 (SEM = ±0.7) | 2.4 (SEM = ±0.5) | 0.13 |
LOS is reported as days; PAL and AFIB are reported as percentages.
*p≤0.05.
AFIB, atrial fibrillation; LOS, length of stay; mo, months; PAL, prolonged air leak.
Figure 1.

Summary of median length of stay (LOS) preintervention and postintervention for local and multicentre seminars. Surgical volume is indicated as a value at the base of each bar. Asterisk (*) represents statistical significance (p≤0.05). Error bars represent IQR.
Figure 2.
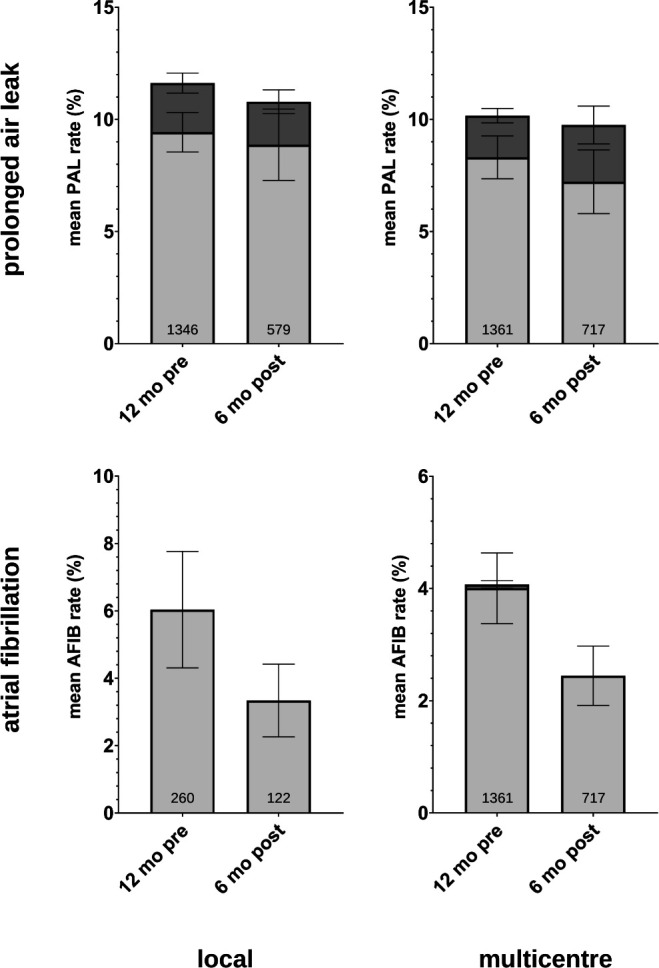
Summary of postoperative adverse event (AE) rates preintervention and postintervention for local and multicentre seminars. Surgical volume is indicated as a value at the base of each bar. Darker (top) subsections of bars represent major AE (PAL or AFIB in their respective graphs). Lighter (bottom) subsections represent minor AE. Error bars represent SE of the mean (SEM). AFIB, atrial fibrillation; PAl, prolonged air leak.
Multicentre seminars
The multicentre seminars (n=4 centres) included yielded a total of 20 consensus recommendations (average 6/seminar) across the 3 topics (LOS, PAL and AFIB). A total of 81 surgeons attended (average 27/seminar), and all seminars culminated in recommendations (table 1).
Table 2 provides the primary outcomes. Median LOS for lobectomy decreased from 4.0 to 3.5 days (p=0.11) while median LOS for all procedures remained at 3.0 days (figure 1). PAL rates decreased from 10.2% to 9.8% (p=0.83), and a subanalysis revealed that major PAL increased from 1.9% to 2.5% (p=0.38) while minor PAL decreased from 8.3% to 7.2% (p=0.53) (figure 2). Finally, AFIB rates decreased from 4.1% to 2.4% (p=0.13), major AFIB rates decreased from 0.1% to 0% (p=0.50) and minor AFIB decreased from 4.0% to 2.4% (p=0.13) (figure 2).
COVID-19 considerations
LOS data from March to May 2020 showed a mean reduction in surgical volume of 21 cases/site (32% reduction). AE data from the same months showed a mean reduction of 12.5 cases/site (40% reduction). These dates were therefore excluded to avoid this unanticipated variable. Specifically, these months were removed from the multicentre LOS analyses (online supplemental figure 2). Additionally, the postintervention periods of multicentre PAL and AFIB analyses were reduced to 6 months to ensure the end of the range lied before March 2020.
Discussion
Implementation of data-informed A&F coupled to best evidence-based and best experience-based quality improvement seminars were universally successful in generating consensus recommendations. While the true impact of these recommendations requires further study, it was encouraging to observe a reduction of 0.5 days for LOS after lobectomy following the respective multicentre seminar. After multicentre PD seminars focusing on AEs, there was a trend in reduction of AFIB and PAL. Local level results showed similar trends, including a significant reduction of 1.0 day following lobectomy, similar to a previously published single-centre experience.24
Combining best evidence (literature review) with best experience (PD) to generate actionable consensus recommendations is unique to this programme and has not, to the best of our knowledge, been applied elsewhere. Continuous data collection/review integrated into care is critical for the measurement and evaluation of practice change, and that is due to the commitment of the participants. A&F informed by this data seems to be more successful when it is collegial, constructive and actionable. Thus, the application of PD to thoracic surgery—a concept first developed in Vietnam, then global public health, and since used to improve performance across a number of healthcare settings27–32—provides an ideal method to identify positive outliers who can help guide a path for underperformers without abasement. Indeed, much of the discussion during multicentre seminars highlighted practice variation within and between institutions. The review of best evidence and best experience serve as a catalyst for discussion. The consensus recommendations generated (table 3 and online supplemental table 3) were in line with current surgical guidelines33–36 and included simple recommendations including rapid discontinuation of suction to reduce PAL, perioperative continuation of beta-blocker usage if prescribed, and pre-emptive magnesium administration to prevent AFIB. Recommendations to reduce LOS were wider-reaching and addressed preoperative, intraoperative and postoperative care.
Table 3.
Multicentre positive deviance seminar recommendations
| Multicentre positive deviance seminars | |
| Topic | Recommendations |
| Prolonged alveolar air leak |
|
| Atrial fibrillation |
|
| Length of stay |
MIS lobectomy Preoperative
Intraoperative
Postoperative
Open lobectomy Preoperative
Intraoperative
Postoperative
|
PCA, patient controlled analgesia; POD, postoperative day; VATS, Video Assisted Thoracic Surgery.
Surgeons have previously reported positively regarding the value of the PD-based approach.23 We note different surgeons/centres are identified demonstrating PD for different outcomes. Surgeons are not often provided an opportunity to discuss details regarding technique and perioperative care among their peers. The positivistic and collegial nature of discussion helps to generate consensus recommendations that may be immediately implemented. Although we look forward to formally evaluating this hypothesis, we believe the culture of collaboration and colearning that this process fosters is invaluable and can also lead to broader collaboration in clinical research.
Though surgery often aims to incorporate a culture of safety, hospital-based quality initiatives are limited in their applicability to specialised surgical disciplines that employ only a limited number of surgeons at each institution. National coordination thus provides a mechanism for centres to compare performance to national averages or benchmarks, and to share techniques across sites within a country. Ideally, these initiatives are led by national professional organisations well suited to identify areas for improvement, then evaluate and disseminate recommendations, as they best understand the unique challenges that exist within their specialty. The Society of Thoracic Surgeons and the European Society for Thoracic Surgeons have long led internationally with longstanding cardiac and thoracic surgery databases that have enabled interinstitutional benchmarking. This study introduces another data-driven methodology to improve care, with broad applicability to other disciplines. A&F using PD provides a potentially effective and efficient means to learn from data to improve quality and safety of care.
Limitations and future directions
We recognise that the limitations associated with this study preclude definitive or causal conclusions. Analyses were conducted using an uncontrolled before/after design, which cannot control for confounding secular trends. A randomised controlled trial was not feasible as all centres participate in the intervention simultaneously, and centres cannot be assigned to function purely as a control group without quality intervention, as that is their reason to perform data collection.
Additionally, the variation in local seminar dates for a given topic presents a limitation to the design of the study and can be explained by two main factors. First, because of the variation in onboarding time by centres, synchronising local seminars focusing on the same topic to occur simultaneously was made impossible. As an example, The Ottawa Hospital was the first centre to begin the programme, so its local seminars date as far back as 2015, while the first local seminars for other sites like McGill University Health Centre occurred as recently as 2019. Second, achieving 100% participation from surgeons is challenging even in single centres, and nearly impossible to coordinate simultaneously across centres to achieve synchronisation. Therefore, the impossibility of synchronised local seminars was a practical limitation of this study. Another related limitation is that overlaps exist between the date ranges of local and multicentre seminars for the same topic (see table 1). This has made it challenging to clearly distinguish between the effects of overlapping local and national seminars, and is the point of future study.
Further, there was no measurement of adoption of recommendations in this study, and not all surgeons were able to participate in all seminars. Though all physicians ranked their acceptance of the recommendations highly at the conclusion of each meeting, we were unable to meaningfully measure to what extent physicians implemented them afterwards and, by extension, the extent to which surgical practice was standardised within and across participating centres. Surgical technique is often personal, with specialists understandably proud of their technique and reluctant to adopt modifications. The measurement of surgeon adoption is the subject of a future study that aims to more rigorously evaluate and further improve the programme. We plan to perform a formal mixed-methods evaluation of the degree to which adoption of recommendations (including barriers and enablers) occurs in addition to other supporting analyses. Indeed, monthly tabulation of AE rates demonstrate considerable variation (online supplemental figures 3–10), and more centres are required for a more stable interrupted time series analysis, which would provide a more rigorous means to evaluate the effect of an intervention when randomisation is not feasible, and will be implemented as the programme continues to expand.
Third, there exists a potential limitation in the consensus recommendations that are generated during seminars. As described in the Methods section, surgeons who have demonstrated PD are identified during seminars and asked to describe the practices that they believe contribute to their strong performance relative to other surgeons. However, like all people, surgeons are subject to the fundamental attribution error, whereby environmental contributors (such as their team members and work environment) are underestimated while personal contributions may be overemphasised. Because of this, factors that may contribute in large part to a surgeon’s performance might be overlooked. This is one of the reasons for why we have ensured a review of the literature as part of the process, to seek synergies between experience and evidence. Nonetheless, this is a limitation that is challenging to overcome, given the difficulty that is inherent in measuring such a variable. We acknowledge the multifaceted nature of surgical care, as we have tried to reflect in our introduction of multicentre seminars in this study (where sites rather than surgeons are the focus for identifying PD, and a representative surgeon of each site is present during a seminar). However, ensuring the inclusion of all viewpoints such as the perspectives of all surgeons during a seminar when generating recommendations is a method for limiting the effect of the fundamental attribution error. Asking all surgeons to independently rate their level of agreement with each recommendation at the end of the session further attempts to address this important issue. In the long run, continually adjusting the process of identifying outliers and generating recommendations in a way that better reflects the surgical care environment and the players involved is a key aspect to be worked on as the programme continues to be developed and refined.
Fourth, LOS analyses were conducted in two forms: LOS following all procedures and LOS following lobectomy individually. The other two procedures studied here (segmentectomy and wedge resection) were not analysed separately for LOS. This is because lobectomy is the most common thoracic procedure and is the only individual procedure with enough volume (number of cases) to enable analysis. This presents a limitation in the power of our analysis and is one that will be overcome as the programme expands to more centres and the volume of procedures available for analysis increases.
Fifth, it has been mentioned above that days in hospital after readmission were recorded but not included in the analysis. When using LOS as a measure for quality improvement, it is recommended that readmission data be included. This is because there is often a risk of premature hospital leave following surgery, after which patients are readmitted. However, in the analyses we have conducted, the number of patients who required readmission were very low, and as such we elected not to include those patients in the LOS calculations. We do, however, acknowledge this as a potential limitation, and emphasise that our results must be interpreted as LOS after index admission only.
Finally, the reduction of elective surgeries due to COVID-19 overlapped with the planned postintervention analyses for this study. COVID-19 affected volume and resulted in changes to cases being performed, in addition to moderate changes to perioperative care and ultimately LOS/AEs. The COVID-19 months were therefore removed to minimise the impact of this unanticipated variable, and a full review of the effects of COVID-19 on Canadian thoracic surgery is subject to another investigation.
Conclusion
This initial experience of a multicentre quality improvement programme based on data-informed A&F, incorporating both best evidence and best experience (ie, PD), to generate consensus recommendations offers a collegial, actionable process with potential to reduce LOS/AEs. This method for collective quality improvement within thoracic surgery provides a framework applicable to any discipline aiming to reduce the incidence of postoperative AEs, and merits further rigorous investigation.
Footnotes
Contributors: AJES, LF, CF, GD, RM, NS, DGF and TKW envisioned and contributed to the implementation of this program and study. AJES directed and supervised the study design, data collection, analysis, interpretation and wrote the manuscript. ZA performed analyses on the collected data and wrote the manuscript. DGF contributed to the implementation of the study and wrote the manuscript. MG collected the data and wrote the manuscript. DJ supervised the analysis and reviewed the manuscript. CA managed data collection and storage, analysis of the results and reviewed the manuscript. All authors contributed to the implementation of the study and reviewed the analysis, results and manuscript. AJES, Guarantor.
Funding: Canadian Partnership Against Cancer / Partenariat Canadien Contre le Cancer. Grant number: #12155.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All data relevant to the findings of this study are contained within the text and online supplemental information. Additional lower level data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Ottawa Health Science Network Research Ethics Board (OHSN-REB)Protocol ID 20180334-01T 'Implementation of a national quality improvement and clinical trials network in thoracic surgery'. Patients were not required to give consent. From the protocol…'Given its observational nature, absence of risk and focus on quality, the QI intervention component of the study represents one of the 'limited circumstances' under which waived consent is permitted by law, on approval by a Research Ethics Board (Tri-Council Policy Statement, Section 2, Article 2.1c ii, v).'
References
- 1.Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 2005;242:326–43. discussion 341-343. 10.1097/01.sla.0000179621.33268.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andalib A, Ramana-Kumar AV, Bartlett G, et al. Influence of postoperative infectious complications on long-term survival of lung cancer patients: a population-based cohort study. J Thorac Oncol 2013;8:554–61. 10.1097/JTO.0b013e3182862e7e [DOI] [PubMed] [Google Scholar]
- 3.Irshad K, Feldman LS, Chu VF, et al. Causes of increased length of hospitalization on a general thoracic surgery service: a prospective observational study. Can J Surg 2002;45:264–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Khan NA, Quan H, Bugar JM, et al. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med 2006;21:177–80. 10.1007/s11606-006-0254-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Z, Mostofian F, Ivanovic J, et al. All grades of severity of postoperative adverse events are associated with prolonged length of stay after lung cancer resection. J Thorac Cardiovasc Surg 2018;155:798–807. 10.1016/j.jtcvs.2017.09.094 [DOI] [PubMed] [Google Scholar]
- 6.Harrison R, Walton M, Manias E, et al. The missing evidence: a systematic review of patients' experiences of adverse events in health care. Int J Qual Health Care 2015;27:424–42. 10.1093/intqhc/mzv075 [DOI] [PubMed] [Google Scholar]
- 7.Grigor EJM, Ivanovic J, Anstee C, et al. Impact of adverse events and length of stay on patient experience after lung cancer resection. Ann Thorac Surg 2017;104:382–8. 10.1016/j.athoracsur.2017.05.025 [DOI] [PubMed] [Google Scholar]
- 8.Vonlanthen R, Slankamenac K, Breitenstein S, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg 2011;254:907–13. 10.1097/SLA.0b013e31821d4a43 [DOI] [PubMed] [Google Scholar]
- 9.The economics of patient safety in acute care 2012.
- 10.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard medical practice study I. N Engl J Med 1991;324:370–6. 10.1056/NEJM199102073240604 [DOI] [PubMed] [Google Scholar]
- 11.Baker GR, Norton PG, Flintoft V, et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ 2004;170:1678–86. 10.1503/cmaj.1040498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finley CJ, Schneider L, Shakeel S. Approaches to high-risk, resource intensive cancer surgical care in Canada 2019.
- 13.Finley CJ, Jacks L, Keshavjee S, et al. The effect of regionalization on outcome in esophagectomy: a Canadian national study. Ann Thorac Surg 2011;92:485–90. 10.1016/j.athoracsur.2011.02.089 [DOI] [PubMed] [Google Scholar]
- 14.Finley CJ, Bendzsak A, Tomlinson G, et al. The effect of regionalization on outcome in pulmonary lobectomy: A Canadian national study. J Thorac Cardiovasc Surg 2010;140:757–63. 10.1016/j.jtcvs.2010.06.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller JD, Jain MK, de Gara CJ, et al. Effect of surgical experience on results of esophagectomy for esophageal carcinoma. J Surg Oncol 1997;65:20–1. [DOI] [PubMed] [Google Scholar]
- 16.Backman C, Vanderloo S, Forster AJ. Measuring and improving quality in university hospitals in Canada: the Collaborative for excellence in healthcare quality. Health Policy 2016;120:982–6. 10.1016/j.healthpol.2016.07.006 [DOI] [PubMed] [Google Scholar]
- 17.Sigler G, Anstee C, Seely AJE. Harmonization of adverse events monitoring following thoracic surgery: pursuit of a common language and methodology. JTCVS Open 2021;6:250–6. 10.1016/j.xjon.2021.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernandez FG, Falcoz PE, Kozower BD, et al. The Society of thoracic surgeons and the European Society of thoracic surgeons General thoracic surgery databases: joint standardization of variable definitions and terminology. Ann Thorac Surg 2015;99:368–76. 10.1016/j.athoracsur.2014.05.104 [DOI] [PubMed] [Google Scholar]
- 19.Jacobs JP, Shahian DM, D'Agostino RS, et al. The Society of thoracic surgeons national database 2018 annual report. Ann Thorac Surg 2018;106:1603–11. 10.1016/j.athoracsur.2018.10.001 [DOI] [PubMed] [Google Scholar]
- 20.Brunelli A, Berrisford RG, Rocco G, et al. The European thoracic database project: composite performance score to measure quality of care after major lung resection. Eur J Cardiothorac Surg 2009;35:769–74. 10.1016/j.ejcts.2009.01.037 [DOI] [PubMed] [Google Scholar]
- 21.Seely AJE, Ivanovic J, Threader J, et al. Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg 2010;90:936–42. 10.1016/j.athoracsur.2010.05.014 [DOI] [PubMed] [Google Scholar]
- 22.Ivanovic J, Al-Hussaini A, Al-Shehab D, et al. Evaluating the reliability and reproducibility of the Ottawa thoracic morbidity and mortality classification system. Ann Thorac Surg 2011;91:387–93. 10.1016/j.athoracsur.2010.10.035 [DOI] [PubMed] [Google Scholar]
- 23.Lindberg C, Downham G, Buscell P, et al. Embracing collaboration: a novel strategy for reducing bloodstream infections in outpatient hemodialysis centers. Am J Infect Control 2013;41:513–9. 10.1016/j.ajic.2012.07.015 [DOI] [PubMed] [Google Scholar]
- 24.Sreeramoju P, Dura L, Fernandez ME, et al. Using a positive deviance approach to influence the culture of patient safety related to infection prevention. Open Forum Infect Dis 2018;5:ofy231. 10.1093/ofid/ofy231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ivanovic J, Anstee C, Ramsay T, et al. Using surgeon-specific outcome reports and positive deviance for continuous quality improvement. Ann Thorac Surg 2015;100:1188–95. discussion 1194-1195. 10.1016/j.athoracsur.2015.04.012 [DOI] [PubMed] [Google Scholar]
- 26.Ivanovic J, Mostofian F, Anstee C, et al. Impact of surgeon Self-evaluation and positive deviance on postoperative adverse events after non-cardiac thoracic surgery. J Healthc Qual 2018;40:e62–70. 10.1097/JHQ.0000000000000130 [DOI] [PubMed] [Google Scholar]
- 27.Marsh DR, Schroeder DG, Dearden KA, et al. The power of positive deviance. BMJ 2004;329:1177–9. 10.1136/bmj.329.7475.1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahrari M, Houser RF, Yassin S, et al. A positive deviance-based antenatal nutrition project improves birth-weight in upper Egypt. J Health Popul Nutr 2006;24:498–507. [PMC free article] [PubMed] [Google Scholar]
- 29.Stuckey HL, Boan J, Kraschnewski JL, et al. Using positive deviance for determining successful weight-control practices. Qual Health Res 2011;21:563–79. 10.1177/1049732310386623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marra AR, Guastelli LR, de Araújo CMP, et al. Positive deviance: a new strategy for improving hand hygiene compliance. Infect Control Hosp Epidemiol 2010;31:12–20. 10.1086/649224 [DOI] [PubMed] [Google Scholar]
- 31.Arsunan AA, Syamsiar SR, Muhammad AN, et al. Identification and strengthening of positive deviance: an efforts to reduce the incidence of malaria in Selayar islands. Enfermería Clínica 2020;30:528–32. 10.1016/j.enfcli.2019.07.153 [DOI] [Google Scholar]
- 32.Howell EA, Ahmed ZN, Sofaer S, et al. Positive deviance to address health equity in quality and safety in obstetrics. Clin Obstet Gynecol 2019;62:560–71. 10.1097/GRF.0000000000000472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singhal S, Ferraris VA, Bridges CR, et al. Management of alveolar air leaks after pulmonary resection. Ann Thorac Surg 2010;89:1327–35. 10.1016/j.athoracsur.2009.09.020 [DOI] [PubMed] [Google Scholar]
- 34.Burt BM, Shrager JB. Prevention and management of postoperative air leaks. Ann Cardiothorac Surg 2014;3:21618–21218. 10.3978/j.issn.2225-319X.2014.03.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernando HC, Jaklitsch MT, Walsh GL, et al. The Society of thoracic surgeons practice guideline on the prophylaxis and management of atrial fibrillation associated with general thoracic surgery: Executive summary. Ann Thorac Surg 2011;92:1144–52. 10.1016/j.athoracsur.2011.06.104 [DOI] [PubMed] [Google Scholar]
- 36.Frendl G, Sodickson AC, Chung MK, et al. 2014 AATS guidelines for the prevention and management of perioperative atrial fibrillation and flutter for thoracic surgical procedures. J Thorac Cardiovasc Surg 2014;148:e153–93. 10.1016/j.jtcvs.2014.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2022-001997supp001.pdf (74.3KB, pdf)
bmjoq-2022-001997supp002.pdf (727.3KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All data relevant to the findings of this study are contained within the text and online supplemental information. Additional lower level data are available on reasonable request.


