Abstract
The COVID‐19 pandemic and its accompanying infection control measures introduced sudden and significant disruptions to the lives of children and adolescents around the world. Given the potential for negative impacts on the mental health of youths as a result of these changes, we conducted a systematic review and meta‐analysis to examine the prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances in children and adolescents during the pandemic. We searched major literature databases for relevant cross‐sectional or longitudinal studies that included primary and secondary school students or children and adolescents ≤18 years of age. Prevalence values were extracted, logit‐transformed, and pooled. Based on 191 included studies with 1,389,447 children and adolescents, we found the pooled prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances to be 31%, 31%, and 42%, respectively. Age, grade levels, education levels, gender, geographical regions, and electronics use were correlated with the prevalence of mental health symptoms. The prevalence of mental health symptoms also increased with time, although signs of recovery and stabilization were also observed. Overall, the results from this review demonstrate the need for increased mental health research, monitoring, and intervention for children and adolescents during the current and future pandemics.
Keywords: adolescent, anxiety, children, COVID‐19, depression, sleep disturbances
The COVID‐19 pandemic and its accompanying infection control measures introduced significant disruptions to the lives of children and adolescents. We conducted a systematic review and meta‐analysis to examine the prevalence of mental health issues in youths and found the pooled prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances to be 31%, 31%, and 42%, respectively. These results call for increased mental health research for children and adolescents.

INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic has greatly impacted the lives of people around the world, both physically and mentally. As countries and governments strived to mitigate the impact of the virus on vulnerable populations and overstretched healthcare systems using limited resources, the psychological wellbeing of their populations was often overlooked. 1 Before comprehensive vaccination programs were introduced, measures, such as widespread lockdowns, closure of businesses and public institutions, and the termination of social gatherings, were used as primary infection control strategies. 2 These restrictions caused significant psychological aggravations as they led to familial separation, reduced personal freedoms and socialization, and increased risks of financial instability due to unemployment and disruptions to global supply chains. 3 The continuously evolving nature of the pandemic also serves as a constant stressor, as previous studies have shown that large‐scale, unpredictable, traumatic events can intrinsically leave affected individuals in a state of shock and insecurity. 4 These aforementioned factors, compounded by alarmist reporting from influential news sources and social media, 5 , 6 have shaped the pandemic into an unprecedented threat to the global mental health landscape.
Indeed, systematic reviews conducted during the early periods of the COVID‐19 pandemic have shown worrying mental health trends involving multiple populations. Among the general global population, the estimated prevalence of major depressive disorders and anxiety disorders increased by over 20% during 2020. 7 Additionally, elevated levels of mental health disorders were commonly reported by studies conducted among vulnerable populations, such as COVID‐19 patients, 8 college students, 9 and healthcare workers. 10 Despite the implementation of COVID‐19 vaccines and new antiviral therapies, resistant viral variants, such as Omicron and Omicron sublineages, 11 continue to affect the daily lives of individuals, especially those residing in low‐ and middle‐income countries (LMICs) that have limited access to vaccines. 12 Recent COVID‐19 resurgences in densely populated countries, such as China, have also led to renewed lockdown measures in an attempt to curb viral transmission. 13 , 14 It is evident that the psychological impact of the virus will persist as the world enters the third year of the pandemic; thus, continued mental health research and monitoring are warranted to evaluate the need for implementing mental health services and preventive strategies for pandemic‐related psychological disorders.
Children and adolescents, who often benefit from routine and structured activities, 15 have been particularly vulnerable to the psychological effects of the pandemic and its associated infection control measures. 16 In the fall semester of 2020, numerous countries, including Canada, the United States, Australia, and China, elected to only partially reopen schools in select low‐risk regions or through the implementation of virtual learning technologies. According to worldwide data from the United Nations Educational, Scientific and Cultural Organization (UNESCO), over 600 million children and adolescents have been impacted by these schooling changes. 17 Previous investigations have shown that youths who are out‐of‐school or engaging in virtual learning are less physically active, have increased screen time, and have irregular sleeping patterns. 18 , 19 , 20 These factors have been shown in prepandemic studies to be major drivers of mental health disorders in children and adolescents, 21 , 22 , 23 and these problems were expected to worsen due to forced home confinement and decreased interaction with other youths during the pandemic. 24 , 25 Barring impacts from school closures, children and adolescents are also directly affected by the pandemic in ways similar to their adult counterparts. 26 , 27 For example, fear concerning the wellbeing of friends and family or externalization of finance‐related problems from parents and guardians 28 can take a persistent toll on youths’ mental health status. 25 Children who have parents or relatives infected with SARS‐CoV‐2 or working as frontline healthcare workers may also be particularly susceptible to mental health problems due to constant grief and worry. 25 , 29
Without early detection and timely intervention, pandemic‐related mental health issues can substantially disrupt children and adolescents’ performance in school, as well as their behaviors and self‐discipline at home and within their communities. 30 , 31 Undetected and untreated disorders may also lead to self‐harm via increased risks of suicidal ideation, which became the second leading cause of mortality among adolescents aged 10–19 in the United States based on prepandemic data from 2019. 32 Additionally, youths struggling with emotional problems may adopt unhealthy coping strategies, such as substance abuse. 33 , 34 In the long‐term, adults who have experienced mental health problems during childhood or adolescence may be at risk of developing substance dependence, having reduced earning potentials, or having difficulty forming long‐lasting social relationships. 35
Although there has been substantial research interest in the physical manifestations of COVID‐19 in children and adolescents, more extensive research on the psychological impact of the pandemic in this population is required. A previous review published in August 2021 suggested that the prevalence of depressive and anxiety symptoms in children and adolescents was 25% and 21%, respectively. 36 However, its findings were limited by low sample sizes, significant publication bias, and a lack of in‐depth analysis of effects from covariates, such as grade levels, electronics use, or physical activity. Additionally, while the study found significant positive temporal trends with mental health symptoms, the majority of included studies were conducted in the early stages of the pandemic. Therefore, we conducted this systematic review and meta‐analysis to provide an updated and more comprehensive assessment of the prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances in children and adolescents. Additionally, we assessed the impact of different covariates and moderators on the mental health status of this population.
METHODS
We conducted this systematic review and meta‐analysis in accordance with the Preferred Reporting Items for Systematic Review and Meta‐Analysis (PRISMA) 2020 guidelines 37 (see Table S1 for the PRISMA checklist) and followed recommendations from the Cochrane Handbook for Systematic Reviews of Interventions. 38 This systematic review was prospectively registered on PROSPERO 39 (CRD42020195965).
Literature search
We systematically searched the following databases from January 1st, 2020 to October 10th, 2022 for relevant publications: (1) EBSCOhost CINAHL; (2) Ovid EMBASE; (3) Ovid MEDLINE; (4) Ovid PsycINFO; (5) PubMed Clinical Queries (with COVID‐19 General Filter); (6) Web of Science Core Collection; and (7) China National Knowledge Infrastructure (CNKI). The search strategies used are appended in Tables S2–S8. Additionally, we hand‐searched the reference sections of reviews identified during the database search for relevant publications.
Eligibility criteria
Publications were included in the meta‐analysis if they met the following criteria: (1) primary cross‐sectional or longitudinal studies conducted after January 2020 (or reported data from time points after January 2020); (2) included children and adolescents ≤18 years of age or students enrolled in primary or secondary educational institutions; and (3) reported the prevalence of depressive symptoms, anxiety symptoms, and/or sleep disturbances, as assessed using self‐reported instruments or clinical interviews. Studies specifically targeting children with special needs or pre‐existing mental health disorders were excluded. No limitations on the publication's language or country of origin were placed.
Study selection
Following deduplication using Endnote 20, we screened titles and abstracts retrieved from the database searches independently and in‐duplicate using Rayyan 40 against the aforementioned eligibility criteria. Study entries deemed relevant by two reviewers were subsequently entered into an in‐duplicate full‐text screening process. Disagreements during both stages were resolved via arbitration with a senior author.
Data extraction
Data extraction was completed independently and in‐duplicate using a standardized data extraction form designed a priori. The following data items were included in the data extraction form: (1) study methods and metadata (i.e., author's last name, year of publication, country of study origin, cross‐sectional/longitudinal study design, duration of data collection, and response rate); (2) participant characteristics (i.e., sample size, gender distributions, mean/median age with variance, and inclusion criteria, such as grade level or education level); and (3) outcome‐related data (i.e., assessment scales and thresholds for depressive symptoms, anxiety symptoms, and sleep disturbances, in addition to overall prevalence values, and prevalence values stratified by prespecified subgroups). Disagreements were resolved via arbitration with a senior author. When we encountered longitudinal studies that reported outcome values at multiple time points, we included only the prevalence at the earliest time point after January 2020 in the meta‐analyses. Data from the remaining time points were included for completing the meta‐regression analyses by the date of data collection.
For studies with missing information, we made attempts to contact the principal investigators to obtain relevant unpublished data.
Risk of bias assessment
We assessed the risk of bias for each included study using a validated tool developed by Hoy et al. 41 The tool assesses methodological quality across 10 items addressing a prevalence study's external and internal validity. Each criterion was given a score of 0 if it was unaddressed/unclear or a score of 1 if it was met. The overall risk of bias was rated as either low (score >8), moderate (score 6−8), or high (score ≤5) based on threshold values established in previous systematic reviews. 42 , 43
Statistical analysis
We performed random‐effects prevalence meta‐analysis using the meta 5.2‐0 library in R. 44 Prevalence values were logit‐transformed and pooled using a generalized linear mixed‐effects model 45 with Hartung–Knapp adjustment. 46 , 47 In addition to synthesizing the total prevalence values, we also pooled the prevalence of the assessed mental health conditions by different severities (mild, moderate, or severe as defined by individual study criteria).
The presence of heterogeneity was assessed using Cochran's Q test with a significance level of p Q < 0.10 following recommendations from the Cochrane Handbook. 38 We further quantified heterogeneity using I 2 statistics. An I 2 value ≥75% was considered to be indicative of serious heterogeneity as recommended by the Cochrane Handbook. 38 Lastly, we assessed the presence of small study effects as an indication of publication bias using funnel plots and Egger's regression tests. 48
Meta‐regressions and subgroup analyses
To assess the impact of covariates and moderators on the pooled prevalences and heterogeneity, we conducted subgroup analyses based on the following prespecified subgroups: (1) gender; (2) education level (elementary/primary school vs. junior secondary/middle school vs. senior secondary/high school); (3) geographical region as defined by the World Health Organization regional classification; and (4) screening tools and threshold values used for assessment of mental health symptoms. Additionally, we performed subgroup analyses based on potential risk factors for mental health issues in youths identified in previous studies: (1) levels of physical activity (defined as per individual study criteria); 49 (2) level of electronics/Internet use (defined as per individual study criteria); 50 , 51 (3) infection in relatives; 25 , 29 , 52 (4) parents/guardians as healthcare workers; 25 , 29 , 52 and (5) financial difficulties. 53
In addition to the subgroup analyses, we performed meta‐regressions to assess correlations between the pooled prevalence and individual study‐level covariates. We prospectively chose mean age, grade level, and date of data collection (expressed as the number of months since January 1st, 2020 to the last day of the study duration) as our covariates of interest. Only one covariate was fit into each meta‐regression model.
Based on reviewer feedback, a post hoc nonlinear regression was completed for the date of data collection with a restricted cubic spline (RCS) model using the metafor 3.8‐1 and rms 6.3‐0 libraries in R. 54 The model consists of multiple connected, continuous cubic polynomials separated by knots. Five knots were used for nonlinear regressions in this review following recommendations from previous studies, 55 positioned at the 5th, 25th, 50th, 75th, and 95th percentiles of date distribution. The Akaike Information Criterion (AIC) was used to compare the model fit between the nonlinear and linear meta‐regression models for the date of data collection. A lower AIC indicates a better relative model fit.
Sensitivity analyses
To assess the impact of study biases on the pooled prevalences, we conducted the following post hoc sensitivity analyses: (1) including only studies using validated screening tools; (2) including only studies using self‐rated screening tools; and (3) excluding studies with a high risk of bias.
RESULTS
After deduplication, we assessed 24,926 abstracts for eligibility (see Figure 1). After the screening process, 191 studies were included in the systematic review 50 , 51 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 , 193 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 , 211 , 212 , 213 , 214 , 215 , 216 , 217 , 218 , 219 , 220 , 221 , 222 , 223 , 224 , 225 , 226 , 227 , 228 , 229 , 230 , 231 , 232 , 233 , 234 , 235 , 236 , 237 , 238 , 239 , 240 , 241 , 242 , 243 , 244 with a total of 1,389,447 children and adolescents. The mean age of the included participants ranged from 4.1 to 18.9 years old. Additional information regarding the included studies and participants is tabulated in Table S9.
FIGURE 1.
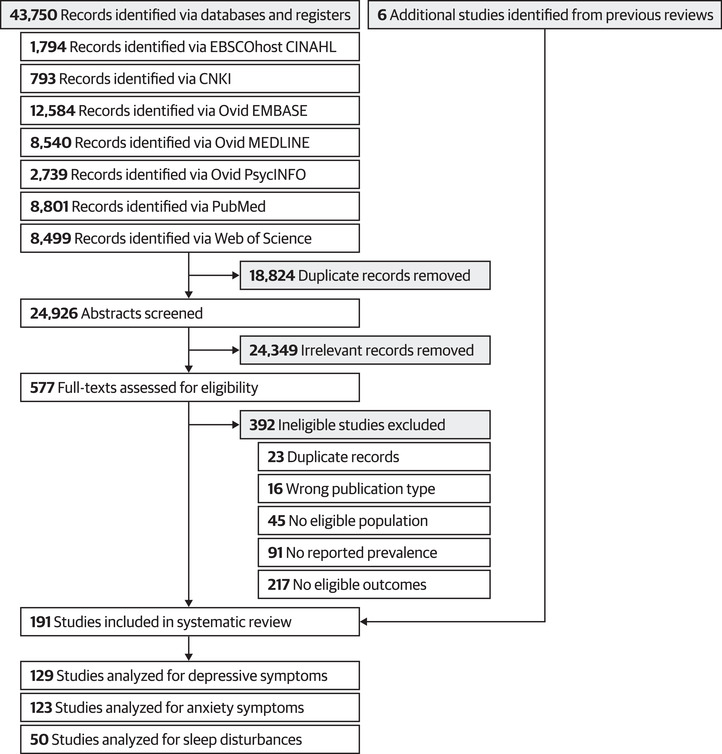
PRISMA flowchart for the identification and selection of relevant studies.
A majority of the included studies used cross‐sectional survey designs with convenience snowball sampling conducted online or in local schools. Overall, 135 studies (70.7%) were conducted in 2020, 26 studies (13.6%) were conducted in 2021, and one study (0.5%) was conducted in 2022. Four studies (2.1%) were conducted using longitudinal designs over multiple years. The remaining 25 studies (13.1%) did not explicitly report the duration of data collection.
Thirty‐one studies (16.2%) assessed youths from Region of the Americas, nine studies (4.7%) assessed youths from the Eastern Mediterranean Region, 44 studies (23.0%) assessed youths from the European Region, 10 studies (5.2%) assessed youths from the South‐East Asia Region, and 95 studies (49.7%) assessed youths from the Western Pacific Region. Two studies (1.0%) included participants from multiple geographical regions. No studies reported data originating from the African Region.
Risk of bias
Using the risk of bias tool developed by Hoy et al., 41 35 studies (18.3%) were rated as having a low risk of bias, 138 studies (72.3%) were rated as having a moderate risk of bias, and 18 studies (9.4%) were rated as having a high risk of bias. A majority of included studies were rated as having a moderate or high risk of bias due to deficiencies in items relating to external validity, such as the use of snowball/convenience sampling, the inclusion of mainly local youths (who may not be an accurate representation of the national or regional youth population), and low or unreported response rates. The risk of bias ratings are summarized in Figure 2 and tabulated in Table S10.
FIGURE 2.
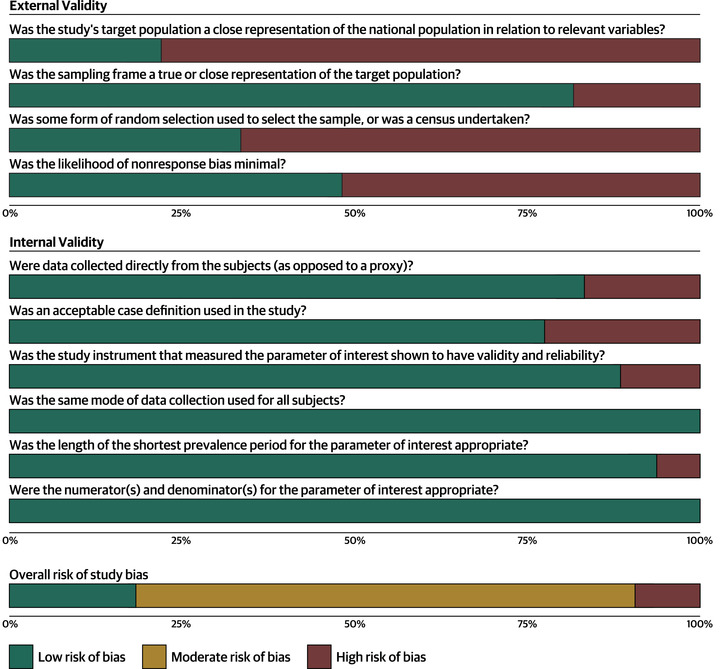
Summary diagram showing an overview of the risk of bias ratings of the included studies.
Prevalence of depressive symptoms
The pooled prevalence of depressive symptoms from 129 studies (n = 524,417) was 31% (95% CI 27−35%; see Figure 3 and Figure S1) with serious and significant heterogeneity (I 2 = 100%, p Q < 0.01). The prevalence of mild, moderate, and severe depressive symptoms was 19% (95% CI 15−24%), 13% (95% CI 10−16%), and 6% (95% CI 4−9%), respectively.
FIGURE 3.
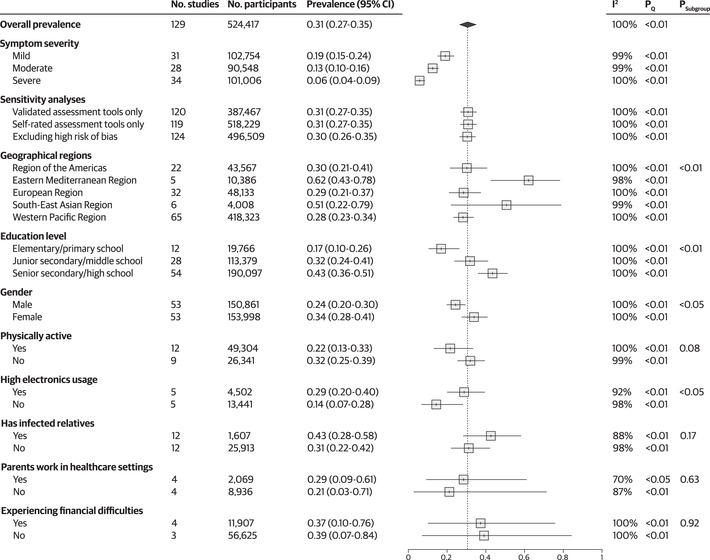
Forest plot showing the pooled prevalence of depressive symptoms and results of sensitivity analyses and subgroup analyses. Psubgroup indicates the result of the test for subgroup differences. Abbreviation: CI, confidence interval.
There were significant subgroup differences by screening tools and threshold values (p < 0.01; see Figure S2). The most commonly reported screening tool was Patient Health Questionnaire‐9 with a positive screening threshold of ≥5 (used by 22 studies with n = 155,587), which yielded a prevalence of 44% (95% CI 36−52%). This value is substantially greater than the overall prevalence estimate.
None of the sensitivity analyses led to any notable changes to the pooled prevalence (see Figure 3), and there were no significant small study effects as an indication of publication bias (p = 0.95; see Figure S3).
Prevalence of anxiety symptoms
The pooled prevalence of anxiety symptoms from 123 studies (n = 1,241,604) was 31% (95% CI 27−35%; see Figure 4 and Figure S4) with serious and significant heterogeneity (I 2 = 100%, p Q < 0.01). The prevalence of mild, moderate, and severe anxiety symptoms was 19% (95% CI 15−24%), 12% (95% CI 8−17%), and 5% (95% CI 3−7%), respectively.
FIGURE 4.
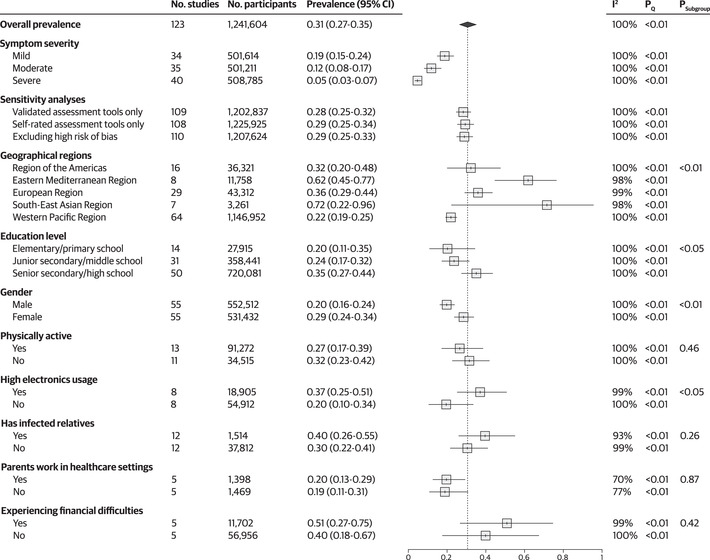
Forest plot showing the pooled prevalence of anxiety symptoms and results of sensitivity analyses and subgroup analyses. Psubgroup indicates the result of the test for subgroup differences. Abbreviation: CI, confidence interval.
There were significant subgroup differences by screening tools and threshold values (p < 0.01; see Figure S5). The most commonly reported screening tool was Generalized Anxiety Disorder‐7 with a positive screening threshold of ≥5 (used by 27 studies with n = 604,491), yielding a prevalence of 35% (95% CI 29−41%) which is 4% greater compared to the overall prevalence estimate.
Sensitivity analysis yielded minor changes in the prevalence estimates. Excluding studies using nonvalidated tools reduced the prevalence by 3%, while excluding parental‐rated scales and studies with high risks of bias reduced the prevalence by 2% (see Figure 4). There were no significant indications of publication bias (p = 0.95; see Figure S6).
Prevalence of sleep disturbances
The pooled prevalence of sleep disturbances from 50 studies (n = 104,219) was 42% (95% CI 33−52%; see Figure 5 and Figure S7) with serious and significant heterogeneity (I 2 = 100%, p Q < 0.01). We did not conduct analyses stratified by symptom severity due to a paucity of data. Excluding studies using nonvalidated tools and studies with a high risk of bias increased the prevalence by 4% and 3%, respectively, while excluding studies using parental‐rated tools reduced the prevalence by 5% (see Figure 5). There were no significant indications of publication bias (p = 0.83; see Figure S8).
FIGURE 5.
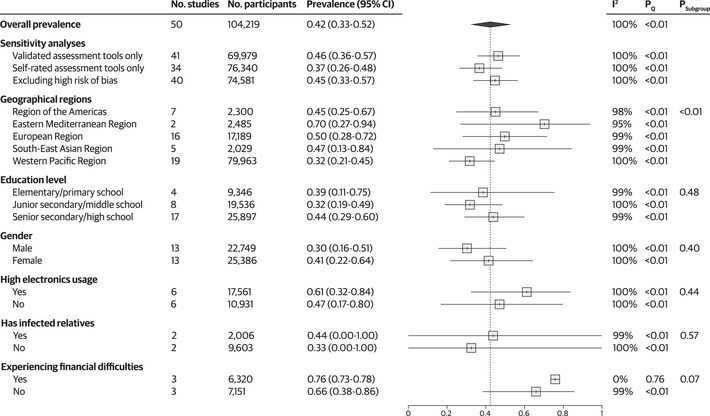
Forest plot showing the pooled prevalence of sleep disturbances and results of sensitivity analyses and subgroup analyses. Psubgroup indicates the result of the test for subgroup differences. Abbreviation: CI, confidence interval.
There were significant subgroup differences by screening tools and threshold values (p < 0.01; see Figure S9). The most commonly reported screening tool was the Pittsburgh Sleep Quality Index (PSQI) with a positive screening threshold of >5, which was used by 13 studies with a collective sample size of 28,483 youths. The pooled prevalence based on assessments using the criteria of PSQI > 5 was 48% (95% CI 30−66%), which is 6% greater compared to the overall pooled estimate.
Subgroup analyses by geographical region
There were significant subgroup interactions by geographical regions for all assessed outcomes. Specifically, the prevalence of depressive and anxiety symptoms was substantially higher for youths from the Eastern Mediterranean and European Regions compared to other regions. Additionally, the prevalence of sleep disturbances was also higher for youths from the Eastern Mediterranean Region compared to other regions. In contrast, youths from the Western Pacific Region reported a substantially lower prevalence of sleep disturbances and anxiety symptoms compared to other regions (see Figures 3, 4, 5 and Figures S10–S12).
Subgroup analyses by education level
We found significant subgroup interactions by education level for the prevalence of depressive (see Figure S13) and anxiety (see Figure S14) symptoms but not for the prevalence of sleep disturbances. Students in high school reported a higher prevalence of depressive and anxiety symptoms compared to middle and elementary school students. Additionally, students in middle school also reported higher prevalences of depressive symptoms compared to elementary school students (see Figures 3, 4, 5).
Subgroup analyses by gender
There were significant subgroup interactions by gender for the prevalence of depressive (see Figure S15) and anxiety (see Figure S16) symptoms but not for the prevalence of sleep disturbances. While we planned to include other genders apart from male and female in this subgroup analysis, no studies reported relevant subgroup outcomes for noncisgender subgroups. Female youths reported higher prevalences of depressive and anxiety symptoms compared to male youths (see Figures 3, 4, 5).
Subgroup analyses by electronics usage
There were significant subgroup interactions by electronics usage for the prevalence of depressive (see Figure S17) and anxiety (see Figure S18) symptoms but not for the prevalence of sleep disturbances. The definitions used by each study to define high electronics usage are tabulated in Table S11. Youths with high electronics usage reported a higher prevalence of depressive and anxiety symptoms compared to youths with low electronics usage (see Figures 3, 4, 5).
Other subgroup analyses
None of the subgroup analyses yielded significant interactions apart from the aforementioned subgroups. Subgroup analyses by physical activity levels and parental healthcare occupations were not conducted for the prevalence of sleep disturbances due to a lack of data. The results of these subgroups are listed in Figures 3, 4, 5.
Meta‐regression analyses
Based on the meta‐regression analyses, there were significant positive correlations between the prevalence of depressive symptoms and age (p < 0.01; see Figure 6A) and grade levels (p < 0.01; see Figure 6B). The prevalence of anxiety was positively correlated with grade levels (p < 0.01; see Figure 6C) but not age (p = 0.07). The prevalence of sleep disturbances was not correlated with age (p = 0.16) or grade levels (p = 0.65).
FIGURE 6.
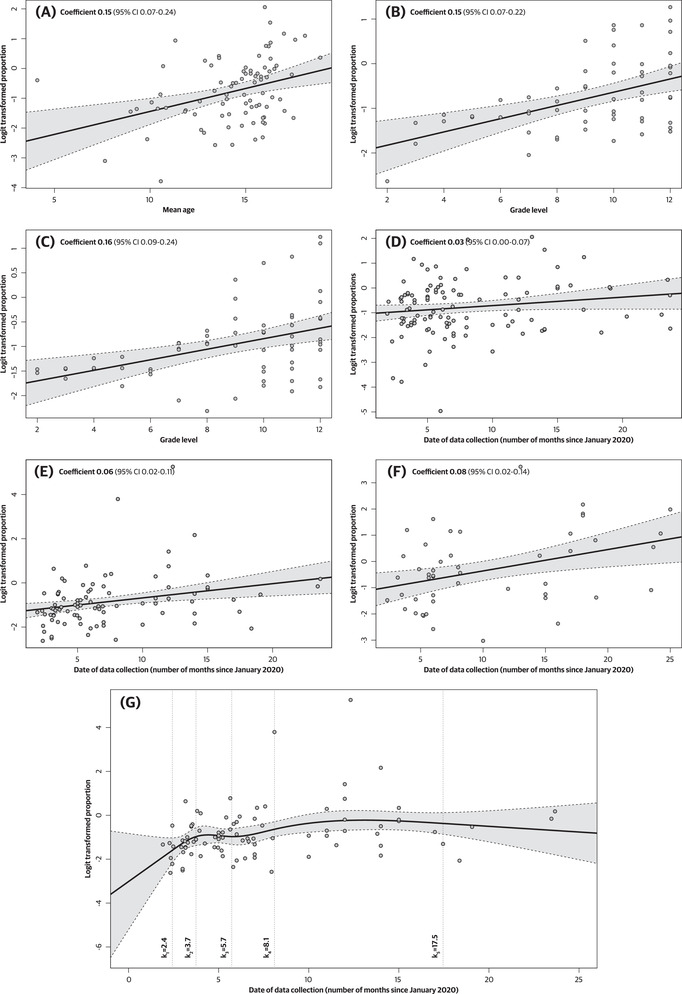
Bubble plots showing results of the meta‐regression analysis between the prevalence of depressive symptoms, anxiety symptoms, sleep disturbances, and moderator variables. The solid line represents the regression line, while the dotted lines show the 95% confidence interval around the regression line. (A) Meta‐regression between the prevalence of depressive symptoms and mean age. (B) Meta‐regression between the prevalence of depressive symptoms and grade level. (C) Meta‐regression between the prevalence of anxiety symptoms and grade level. (D) Meta‐regression between the prevalence of depressive symptoms and date of data collection. (E) Meta‐regression between the prevalence of anxiety symptoms and date of data collection. (F) Meta‐regression between the prevalence of sleep disturbances and date of data collection. (G) Nonlinear meta‐regression using a restricted cubic spline model between the prevalence of anxiety symptoms and date of data collection. Locations of the five knots are shown in the plot.
All three outcomes were positively correlated with the date of data collection in the linear meta‐regression (p < 0.05 for depressive symptoms and p < 0.01 for both anxiety symptoms and sleep disturbances; see Figure 6D–F). However, only the prevalence of anxiety was correlated with date of data collection in the nonlinear RCS model meta‐regression (p < 0.01, with p = 0.13 for depressive symptoms and p = 0.10 for sleep disturbances). As shown in Figure 6G, the prevalence of anxiety symptoms rapidly increased during the first 5 months of the pandemic, before transitioning to a more gradual rate of increase during the summer and the following fall school semester. Although study data became more scarce after 2020, a slight downward trend in the prevalence of anxiety symptoms can be identified starting in the winter semester of 2021. The nonlinear RCS model showed a slightly better model fit (AIC = 264.6) compared to the linear model (AIC = 269.5) for the prevalence of anxiety symptoms based on AIC.
DISCUSSION
The current systematic review and meta‐analysis provides a comprehensive global estimate of the prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances among youths during the COVID‐19 pandemic. The pooled prevalence of depressive symptoms was 31% based on data from 129 studies, including 524,417 youths, the prevalence of anxiety symptoms was 31% based on 123 studies, including 1,241,604 youths, and the prevalence of sleep disturbances was 42% based on 50 studies, including 104,219 youths. These findings are higher compared to the previous review on this topic, which found a pooled prevalence of depressive and anxiety symptoms of 25% and 21%, respectively, based on early pandemic data from 80,879 youths. 36
Differences in prevalence estimates by geographical regions
The results of our subgroup analyses and meta‐regressions identified several significant associations. First, the prevalence estimates differed significantly based on geographical regions for all assessed outcomes. While the prevalence estimates for the Region of the Americas and the European Region were similar to the overall pooled prevalence, prevalence estimates from the South‐East Asian Region and the Eastern Mediterranean Region were substantially elevated compared with other regions studied. A possible explanation for this observation is the more limited mental health coverage in these areas. For example, recent studies found that India (which constituted a majority of the sample size from the South‐East Asian Region) has a treatment gap of approximately 95% in all age groups for common mental health disorders. 245 The national and state‐level policies regarding mental health coverage in India also do not have a specific emphasis on children and adolescent mental health, with most initiatives in the country being led by nonprofit organizations. 245 Additionally, the disparities in prevalence estimates could be attributable to the higher rates of poverty in these regions. Notably, while the Eastern Mediterranean Region consists of a mix of high‐income and LMIC countries, the participants included in this study mainly originated from LMIC countries in the region, such as Jordan and Iran. The impact of socioeconomic indicators on youth wellness and mental health has been well‐established in previous studies. 246 , 247 , 248 Lastly, geopolitical instability and tension in the Eastern Mediterranean Region may also contribute to the high prevalence estimates in the region. 249
Meanwhile, studies from the Western Pacific Region yielded a substantially lower prevalence of anxiety symptoms and sleep disturbances compared to other regions. This observation (which included mainly Chinese youths) is not unique to this review as similar trends have been observed in meta‐analyses involving other populations in this region during the pandemic. 8 , 9 Previous reviews mainly attributed this observation to the stigma associated with the disclosure of mental health conditions in Asian countries, where mental illness and psychological disorders are commonly associated with a distorted personality or moral defects. 250 , 251 , 252 , 253 , 254 , 255 It has also been shown in prepandemic studies that most Chinese individuals with mental health issues do not exhibit help‐seeking behaviors, 256 and the general Chinese population is not familiar with the causes and prevention methods of mental health illnesses. 257
Differences in prevalence estimates by gender
Apart from geographical factors, we identified significant subgroup differences between girls and boys for the prevalence of depressive and anxiety symptoms, where girls exhibited higher prevalence estimates compared to boys. These observations are consistent with findings from prepandemic mental health studies. 258 , 259 The exact cause of this difference is multifactorial and not well understood. 260 However, previous research has shown that boys may have more difficulties acknowledging their mental health problems. Thus, they are more prone to masking these issues by displaying externalizing disorders, such as substance abuse or antisocial behaviors. 261 In contrast, girls are more likely to display internalizing disorders, such as depression and anxiety—both of which were assessed in this review. 261 Societal roles and cultural norms may also contribute to this difference, since girls are more commonly stereotyped as emotionally sensitive and are expected to have greater reactions to stressors and traumatic events (such as the pandemic or the death of family members from viral infection) than boys. 260 , 262
Differences in prevalence estimates by age, education levels, and grade levels
In this review, we assessed the mental health symptoms of different age groups of youths using meta‐regressions by mean age and grade levels as well as a subgroup analysis by education levels. We found that the prevalence of depressive symptoms was positively correlated with all three moderators, while the prevalence of anxiety symptoms was positively correlated with education levels and grade levels only. Similarly, the previous review by Racine et al. also failed to detect age as a significant moderator for the prevalence of anxiety symptoms. Specifically, they attributed this finding to increased anxiety from disruptions in the daily routines of young children. 36 This explanation may be applicable to our current observations as the meta‐regression by age included preschool and early primary school children who may be at‐risk for developing anxiety symptoms due to routine disruptions. Additionally, these younger participants may not be accounted for in the meta‐regression and subgroup analyses by education and grade levels, which consists largely of older children and adolescents.
For school‐aged children, the positive correlation between symptoms of anxiety and depressive with grade and education levels may be attributable to increased academic demands in high school compared to middle and elementary school. 263 These pressures could have been exacerbated by the sudden transition to distance education during lockdowns. 264 Older adolescents may also be more aware of the implications of the pandemic due to greater exposure to news sources and social media, 265 which have been identified as key drivers of mental health issues during the pandemic. 5 , 266
Temporal trends in prevalence estimates
The previous systematic review by Racine et al. identified a positive correlation between the date of data collection and the prevalence of depressive and anxiety symptoms; however, since a majority of the included studies were conducted during the early stages of the pandemic, it was unclear whether this trend would continue. 36 The current review identified a similar correlation after incorporating more studies from later stages of the pandemic (i.e., in late 2020 and 2021). It is likely that prolonged disruptions to youths’ daily routines, academic milestones, and social interactions resulted in a compounding of mental health issues as the pandemic progressed. 36 Interestingly, nonlinear meta‐regression using an RCS model showed that the rate of increase in the prevalence of anxiety symptoms may have slowed after the first 5 months of the pandemic, and a slight downward trend can be observed starting from the winter semester of 2021. This pattern could indicate the recovery or stabilization of mental health in children and adolescents as lockdown efforts eased and distance learning became better established. Further investigations are needed to assess whether this downward trend persists.
Impact of electronics use and screen time on prevalence estimates
Lastly, we identified significant subgroup differences in the prevalence of depressive and anxiety symptoms based on the level of electronics usage. The prevalence of depressive and anxiety symptoms was over 15% lower in children and adolescents with low electronics usage compared to those with high electronics usage. While the impact of screen time on children and adolescent mental health during the pandemic has been widely debated—with proponents demonstrating that one‐on‐one communication with electronic devices can greatly alleviate feelings of isolation and loneliness in this population 267 , 268 —the majority of current evidence suggests that the use of electronics and digital media is more likely to result in worsened mental wellbeing. 267 As previously discussed, exposure to excessive amounts of alarmist or deceptive pandemic‐related information online can instill a constant feeling of worry and fear in youths, which can be detrimental to their mental health. 269 Social media use has also been associated with increased feelings of depression, anxiety, and low self‐esteem due to social comparisons and appearance‐related concerns in youths. 270 , 271 Finally, addiction to or over‐reliance on electronic devices can discourage children and adolescents from engaging in healthy behaviors, such as physical exercise and maintaining regular sleep schedules. 267 , 268 , 272
Implications of findings
The findings from our review show that the pandemic led to a high prevalence of mental health symptoms in children and adolescents, and these effects were exacerbated over time during the early stages of the pandemic. Among the youth population, girls and older adolescents were more prone to developing symptoms of depression and anxiety. Thus, the unique biological and social contexts surrounding these vulnerable populations demand mental health programs that are specifically tailored to their needs. Examples of possible adaptations include providing remote counseling services 273 and resilience‐focused interventions 274 for high school students, working with family members to offer social support during stressful periods, such as university entrance exams, or introducing cognitive‐based gender equality curriculums. 275 Educational antistigma interventions should also be incorporated into academic curriculums to help youths self‐identify signs of mental health issues and encourage help‐seeking behaviors. These measures may be especially important for children and adolescents in the Western Pacific Region.
In addition, we found that high electronics usage may be associated with an increased prevalence of depression or anxiety. It is notable that this finding is limited by small sample sizes and highly heterogeneous definition of electronics usage between studies, thus it should be viewed as hypothesis‐generating and serve as the basis for future large‐scale studies to further assess this association.
Apart from depression and anxiety, over a third of children and adolescents displayed symptoms of sleep disturbances in this review. Sleep disturbances may be a cause, symptom, or comorbidity associated with mental health disorders and substance abuse. 276 , 277 While we did not examine correlations between sleep disturbances and mental health impacts, previous studies have shown that having a regular sleep schedule can greatly improve the physiology and cognition of children and adolescents. 278 Thus, regulating sleep may be a viable way to introduce a routine schedule and reduce mental health disturbances during lockdowns and quarantine measures. Parents may also use the presence of sleep disturbances as an early indicator of mental health issues, thereby facilitating the ability to provide timely preventive measures and psychiatric assessments before the onset of mental health disorders. 279
Overall, there is a great need for further research into children and adolescent mental health during the pandemic, as well as significant resources and investments into evidence‐based and scalable mental health programs for children and adolescents. During future public health emergencies, it is critical to minimize the impact and disruption to youths by leaving school closures as a last resort option. 280
Study limitations
This systematic review has several limitations. First, we observed very high heterogeneity across our analyses. However, this observation is common among many prevalence studies—especially in studies concerning mental health—due to the wide variety of demographic, geographical, and methodological moderators that can lead to between‐study variations in the reported prevalence. 36 In this review, we explored potential sources of heterogeneity using a series of subgroup and meta‐regression analyses and identified several significant factors (such as age, gender, geographical regions, etc.) that may have contributed to the high heterogeneity.
Second, many of our subgroups were limited by low and/or imbalanced sample sizes and inconsistent definitions. As a result, we did not identify subgroup differences by financial difficulties, physical activity, parents who worked in healthcare settings, or children who had infected relatives. Nevertheless, these findings do not necessarily indicate that the aforementioned variables have no significant impact on the mental health of children and adolescents. Subgroup and meta‐regression analyses are exploratory in nature, 281 so further research is needed to fully elucidate the protective and harmful factors involved in children and adolescent mental health during the pandemic.
Additionally, our included studies were mostly rated as having moderate or high risks of bias. The inclusion of studies that lacked random sampling or those that did not include a representative population may limit the external validity of our findings. Notably, because most of our included studies were designed and administered in short timespans, they relied on nonprobabilistic (i.e., convenience) sampling methods, which may lead to a systematic overestimation of prevalence values compared to studies using probabilistic sampling methods. 7 , 282 Thus, caution should be exercised when comparing findings from the current review with prevalence estimates from prepandemic studies.
It is also possible for the design of the included studies to change over time, such as shifting from using convenience sampling methods to probability‐based methods as more time and resources become available. This shift may result in the appearance of a reduction in prevalence values. Thus, the temporal trends observed in this review, especially indications of decreased anxiety symptoms identified on the nonlinear RCS meta‐regression, should be reassessed and confirmed in future longitudinal studies.
Lastly, there was a highly heterogeneous set of screening tools and threshold values used to define clinically relevant symptoms of mental health disorders. While we detected significant differences between the prevalence measures assessed by different screening tools and thresholds, we cannot determine if these differences are due to the construct of the tools themselves or due to other factors (such as gender distribution or differences in geographical regions).
CONCLUSION
The pooled prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances among children and adolescents during the COVID‐19 pandemic was 31%, 31%, and 42%, respectively. Age, grade levels, education levels, gender, geographical regions, and electronics use were associated with an increased prevalence of mental health symptoms. The prevalence of mental health symptoms also increased as the pandemic progressed, although signs of recovery and stabilization were observed. Overall, our findings demonstrate the need for increased mental health research as well as monitoring and intervention for children and adolescents during the current and future pandemics.
AUTHOR CONTRIBUTIONS
J.D. conceptualized and designed the methodology of the study, performed database searches, supervised and performed article screening and data extraction, performed all statistical analyses, drafted the manuscript, and critically reviewed and revised the manuscript. F.Z. helped design the methodology of the study, performed article screening and data extraction, drafted the manuscript, and critically reviewed and revised the manuscript. W.H., K.H., S.L., U.A., Z.S., C.Y.W., O.C., E.H., Q.K.Z., M.M., H.B.R, and S.H. performed article screening and data extraction, as well as critically reviewed the manuscript. All authors have read and approved the final version of the manuscript to be submitted and published, and all authors accept responsibility for the integrity of the data analyzed.
COMPETING INTERESTS
The authors declare no competing interests.
PEER REVIEW
The peer review history for this article is available at: https://publons.com/publon/10.1111/nyas.14947.
Supporting information
Figure S1: Forest plot for the prevalence pooling of depressive symptoms
Figure S2: Forest plot for the subgroup analysis of depressive symptoms by screening tools and threshold values
Figure S3: Funnel plot for the meta‐analysis of depressive symptom prevalence
Figure S4: Forest plot for the prevalence pooling of anxiety symptoms
Figure S5: Forest plot for the subgroup analysis of anxiety symptoms by screening tools and threshold values
Figure S6: Funnel plot for the meta‐analysis of anxiety symptom prevalence
Figure S7: Forest plot for the prevalence pooling of sleep disturbances
Figure S8: Funnel plot for the meta‐analysis of sleep disturbance prevalence
Figure S9: Forest plot for the subgroup analysis of sleep disturbances by screening tools and threshold values
Figure S10: Forest plot for the subgroup analysis of depressive symptoms by geographical regions
Figure S11: Forest plot for the subgroup analysis of anxiety symptoms by geographical regions
Figure S12: Forest plot for the subgroup analysis of sleep disturbances by geographical regions
Figure S13: Forest plot for the subgroup analysis of depressive symptoms by education level
Figure S14: Forest plot for the subgroup analysis of anxiety symptoms by education level
Figure S15: Forest plot for the subgroup analysis of depressive symptoms by gender
Figure S16: Forest plot for the subgroup analysis of anxiety symptoms by gender
Figure S17: Forest plot for the subgroup analysis of depressive symptoms by electronics usage
Figure S18: Forest plot for the subgroup analysis of anxiety symptoms by electronics usage
Table S1: Preferred reporting items for systematic reviews and meta‐analyses (PRISMA 2020) checklist
Table S2: MEDLINE search strategy
Table S3: EMBASE search strategy
Table S4: APA PsycInfo search strategy
Table S5: PubMed search strategy
Table S6: China National Knowledge Infrastructure (CNKI) search strategy
Table S7: Web of Science Core Collection search strategy
Table S8: CINAHL search strategy
Table S9: Characteristics of included studies and patients
Table S10: Risk of bias ratings
Table S11: Subgroup definition for high electronics use
Table S12: Subgroup definition for high physical activity
Table S13: Subgroup definition for financial difficulty
ACKNOWLEDGMENTS
We would like to acknowledge Ms. Arani Kulamurugan, affiliated with Michael G. DeGroote School of Medicine (Niagara Regional Campus) at McMaster University, for her contributions to drafting the preliminary versions of the manuscript. We would also like to thank Ms. Kyra Kavanagh, affiliated with the Faculty of Science at Carleton University, for her contributions to critically revising the manuscript. Lastly, we would like to express our appreciation toward the peer‐reviewers and editors who dedicated their time toward reviewing this manuscript and providing their expertise and insights. The authors received no external support or funding for the completion of this study.
Deng, J. , Zhou, F. , Hou, W. , Heybati, K. , Lohit, S. , Abbas, U. , Silver, Z. , Wong, C. Y. , Chang, O. , Huang, E. , Zuo, Q. K. , Moskalyk, M. , Ramaraju, H. B. , & Heybati, S. (2022). Prevalence of mental health symptoms in children and adolescents during the COVID‐19 pandemic: A meta‐analysis. Ann NY Acad Sci., 00, 1–21. 10.1111/nyas.14947
DATA AVAILABILITY STATEMENT
Data involved in statistical analyses are disclosed in the manuscript, figures, tables, and supplementary materials. Please contact the corresponding author for additional inquiries.
REFERENCES
- 1. Kar, S. K. , Yasir Arafat, S. M. , Kabir, R. , Sharma, P. , & Saxena, S. K. (2020). Coping with mental health challenges during COVID‐19. In Saxena K. S. (Ed.), Coronavirus disease 2019 (COVID‐19): Epidemiology, pathogenesis, diagnosis, and therapeutics (pp. 199–213). Singapore: Springer Singapore. [Google Scholar]
- 2. Girum, T. , Lentiro, K. , Geremew, M. , Migora, B. , Shewamare, S. , & Shimbre, M. S. (2021). Optimal strategies for COVID‐19 prevention from global evidence achieved through social distancing, stay at home, travel restriction and lockdown: A systematic review. Archives of Public Health, 79, 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Msherghi, A. , Alsuyihili, A. , Alsoufi, A. , Ashini, A. , Alkshik, Z. , Alshareea, E. , Idheiraj, H. , Nagib, T. , Abusriwel, M. , Mustafa, N. , Mohammed, F. , Eshbeel, A. , Elbarouni, A. , & Elhadi, M. (2021). Mental health consequences of lockdown during the COVID‐19 pandemic: A cross‐sectional study. Frontiers in Psychology, 12, 605279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Makwana, N. (2019). Disaster and its impact on mental health: A narrative review. Journal of Family Medicine and Primary Care, 8, 3090–3095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thygesen, H. , Bonsaksen, T. , Schoultz, M. , Ruffolo, M. , Leung, J. , Price, D. , & Geirdal, A. Ø. (2021). Social media use and its associations with mental health 9 months after the COVID‐19 outbreak: A cross‐national study. Frontiers in Public Health, 9, 752004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Neill, R. D. , Blair, C. , Best, P. , McGlinchey, E. , & Armour, C. (2021). Media consumption and mental health during COVID‐19 lockdown: A UK cross‐sectional study across England, Wales, Scotland and Northern Ireland. Journal of Public Health, Published ahead of print. 10.1007/s10389-021-01506-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. COVID‐19 Mental Disorders Collaborators . (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID‐19 pandemic. Lancet, 398, 1700–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Deng, J. , Zhou, F. , Hou, W. , Silver, Z. , Wong, C. Y. , Chang, O. , Huang, E. , & Zuo, Q. K. (2020). The prevalence of depression, anxiety, and sleep disturbances in COVID‐19 patients: A meta‐analysis. Annals of the New York Academy of Sciences, 1486, 90–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Deng, J. , Zhou, F. , Hou, W. , Silver, Z. , Wong, C. Y. , Chang, O. , Drakos, A. , Zuo, Q. K. , & Huang, E. (2021). The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID‐19 pandemic: A systematic review and meta‐analysis. Psychiatry Research, 301, 113863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. G. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity, 88, 901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dhawan, M. , Priyanka, & Choudhary, O. P. (2022). Emergence of Omicron sub‐variant BA.2: Is it a matter of concern amid the COVID‐19 pandemic? International Journal of Surgery, 99, 106581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tagoe, E. T. , Sheikh, N. , Morton, A. , Nonvignon, J. , Sarker, A. R. , Williams, L. , & Megiddo, I. (2021). COVID‐19 vaccination in lower‐middle income countries: National stakeholder views on challenges, barriers, and potential solutions. Frontiers in Public Health, 9, 709127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang, X. , Zhang, W. , & Chen, S. (2022). Shanghai's life‐saving efforts against the current Omicron wave of the COVID‐19 pandemic. Lancet, 399, 2011–2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cheshmehzangi, A. , Zou, T. , & Su, Z. (2022). Commentary: China's zero‐COVID approach depends on Shanghai's outbreak control. Frontiers in Public Health, 10, 912992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huremović, D. (2019). Mental health of quarantine and isolation. In Huremović D. (Ed.), Psychiatry of pandemics (pp. 95–118). Cham: Springer International Publishing. [Google Scholar]
- 16. Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395, 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Education: From disruption to recovery . (2020). https://en.unesco.org/covid19/educationresponse
- 18. Brazendale, K. , Beets, M. W. , Weaver, R. G. , Pate, R. R. , Turner‐Mcgrievy, G. M. , Kaczynski, A. T. , Chandler, J. L. , Bohnert, A. , & Von Hippel, P. T. (2017). Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. International Journal of Behavioral Nutrition and Physical Activity, 14, 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang, G. , Zhang, J. , Lam, S. P. , Li, S. X. , Jiang, Y. , Sun, W. , Chan, N. Y. , Kong, A. P. S. , Zhang, Y. , Li, S. , Li, A. M. , Jiang, F. , Shen, X. , & Wing, Y. K. (2019). Ten‐year secular trends in sleep/wake patterns in Shanghai and Hong Kong school‐aged children: A tale of two cities. Journal of Clinical Sleep Medicine, 15, 1495–1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chu, Y.‐H. , & Li, Y. C. (2022). The impact of online learning on physical and mental health in university students during the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 19, 2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Korczak, D. J. , Madigan, S. , & Colasanto, M. (2017). Children's physical activity and depression: A meta‐analysis. Pediatrics, 139, e20162266. [DOI] [PubMed] [Google Scholar]
- 22. Alfano, C. A. , & Gamble, A. L. (2009). The role of sleep in childhood psychiatric disorders. Child & Youth Care Forum, 38, 327–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stiglic, N. , & Viner, R. M. (2019). Effects of screentime on the health and well‐being of children and adolescents: A systematic review of reviews. BMJ Open, 9, e023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang, G. , Zhang, Y. , Zhao, J. , Zhang, J. , & Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID‐19 outbreak. Lancet, 395, 945–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kumar, A. , Nayar, K. R. , & Bhat, L. D. (2020). Debate: COVID‐19 and children in India. Child and Adolescent Mental Health, 25, 165–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dalton, L. , & Rapa, E. , Stein, A. (2020). Protecting the psychological health of children through effective communication about COVID‐19. Lancet Child & Adolescent Health, 4, 346–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Guessoum, S. B. , Lachal, J. , Radjack, R. , Carretier, E. , Minassian, S. , Benoit, L. , & Moro, M. R. (2020). Adolescent psychiatric disorders during the COVID‐19 pandemic and lockdown. Psychiatry Research, 291, 113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bøe, T. , Sivertsen, B. , Heiervang, E. , Goodman, R. , Lundervold, A. J. , & Hysing, M. (2014). Socioeconomic status and child mental health: The role of parental emotional well‐being and parenting practices. Journal of Abnormal Child Psychology, 42, 705–715. [DOI] [PubMed] [Google Scholar]
- 29. Liu, J. J. , Bao, Y. , Huang, X. , Shi, J. , & Lu, L. (2020). Mental health considerations for children quarantined because of COVID‐19. Lancet Child & Adolescent Health, 4, 347–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Golberstein, E. , Wen, H. , & Miller, B. F. (2020). Coronavirus disease 2019 (COVID‐19) and mental health for children and adolescents. JAMA Pediatrics, 174, 819–820. [DOI] [PubMed] [Google Scholar]
- 31. Binagwaho, A. , & Senga, J. (2021). Children and adolescent mental health in a time of COVID‐19: A forgotten priority. Annals of Global Health, 87, 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hink, A. B. , Killings, X. , Bhatt, A. , Ridings, L. E. , & Andrews, A. L. (2022). Adolescent suicide—Understanding unique risks and opportunities for trauma centers to recognize, intervene, and prevent a leading cause of death. Current Trauma Reports, 8, 41–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mohammadi, M. R. , Salehi, M. , Khaleghi, A. , Hooshyari, Z. , Mostafavi, S. A. , Ahmadi, N. , Hojjat, S. K. , Safavi, P. , & Amanat, M. (2020). Social anxiety disorder among children and adolescents: A nationwide survey of prevalence, socio‐demographic characteristics, risk factors and co‐morbidities. Journal of Affective Disorders, 263, 450–457. [DOI] [PubMed] [Google Scholar]
- 34. Smetana, J. G. , Campione‐Barr, N. , & Metzger, A. (2006). Adolescent development in interpersonal and societal contexts. Annual Review of Psychology, 57, 255–284. [DOI] [PubMed] [Google Scholar]
- 35. Goodman, A. , Joyce, R. , & Smith, J. P. (2011). The long shadow cast by childhood physical and mental problems on adult life. Proceedings of the National Academy of Sciences of the United States of America, 108, 6032–6037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Racine, N. , Mcarthur, B. A. , Cooke, J. E. , Eirich, R. , Zhu, J. , & Madigan, S. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID‐19: A meta‐analysis. JAMA Pediatrics, 175, 1142–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Page, M. J. , Mckenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , Mcdonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Higgins, J. P. T. , & Green, S. (2008). Cochrane handbook for systematic reviews of interventions. New Jersey: Wiley. [Google Scholar]
- 39. Booth, A. , Clarke, M. , Dooley, G. , Ghersi, D. , Moher, D. , Petticrew, M. , & Stewart, L. (2012). The nuts and bolts of PROSPERO: An international prospective register of systematic reviews. Systematic Reviews, 1, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ouzzani, M. , Hammady, H. , Fedorowicz, Z. , & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5, 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hoy, D. , Brooks, P. , Woolf, A. , Blyth, F. , March, L. , Bain, C. , Baker, P. , Smith, E. , & Buchbinder, R. (2012). Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. Journal of Clinical Epidemiology, 65, 934–939. [DOI] [PubMed] [Google Scholar]
- 42. Cioana, M. , Deng, J. , Hou, M. , Nadarajah, A. , Qiu, Y. , Chen, S. S. J. , Rivas, A. , Banfield, L. , Chanchlani, R. , Dart, A. , Wicklow, B. , Alfaraidi, H. , Alotaibi, A. , & Thabane, L. , Samaan, M. C. (2021). Prevalence of hypertension and albuminuria in pediatric type 2 diabetes: A systematic review and meta‐analysis. JAMA Network Open, 4, e216069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cioana, M. , Deng, J. , Nadarajah, A. , Hou, M. , Qiu, Y. , Chen, S. S. J. , Rivas, A. , Banfield, L. , Alfaraidi, H. , Alotaibi, A. , Thabane, L. , & Samaan, M. C. (2022). Prevalence of polycystic ovary syndrome in patients with pediatric type 2 diabetes: A systematic review and meta‐analysis. JAMA Network Open, 5, e2147454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schwarzer, G. , Carpenter, J. R. , & Rücker, G. (2015). Meta‐analysis with R. New York: Springer International Publishing. [Google Scholar]
- 45. Schwarzer, G. , Chemaitelly, H. , Abu‐Raddad, L. J. , & Rücker, G. (2019). Seriously misleading results using inverse of Freeman–Tukey double arcsine transformation in meta‐analysis of single proportions. Research Synthesis Methods, 10, 476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Knapp, G. , & Hartung, J. (2003). Improved tests for a random effects meta‐regression with a single covariate. Statistics in Medicine, 22, 2693–2710. [DOI] [PubMed] [Google Scholar]
- 47. Sidik, K. , & Jonkman, J. N. (2002). A simple confidence interval for meta‐analysis. Statistics in Medicine, 21, 3153–3159. [DOI] [PubMed] [Google Scholar]
- 48. Egger, M. , Smith, G. D. , Schneider, M. , & Minder, C. (1997). Bias in meta‐analysis detected by a simple, graphical test. BMJ, 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Biddle, S. J. H. , & Asare, M. (2011). Physical activity and mental health in children and adolescents: A review of reviews. British Journal of Sports Medicine, 45, 886–895. [DOI] [PubMed] [Google Scholar]
- 50. Dong, H. , Yang, F. , Lu, X. , & Hao, W. (2020). Internet addiction and related psychological factors among children and adolescents in China during the coronavirus disease 2019 (COVID‐19) epidemic. Frontiers in Psychiatry, 11, 00751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Duan, L. , Shao, X. , Wang, Y. , Huang, Y. , Miao, J. , Yang, X. , & Zhu, G. (2020). An investigation of mental health status of children and adolescents in China during the outbreak of COVID‐19. Journal of Affective Disorders, 275, 112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Yeasmin, S. , Banik, R. , Hossain, S. , Hossain, M. N. , Mahumud, R. , Salma, N. , & Hossain, M. M. (2020). Impact of COVID‐19 pandemic on the mental health of children in Bangladesh: A cross‐sectional study. Children and Youth Services Review, 117, 105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hageman, J R. (2020). Children's and families' behavioral and mental health during COVID‐19. Pediatric Annals, 49, e405–e406. [DOI] [PubMed] [Google Scholar]
- 54. Stone, C. J. , & Koo, C. Y. (1985). Additive splines in statistics. Proceedings of the Statistical Computing Section ASA.
- 55. Gauthier, J. , Wu, Q. V. , & Gooley, T. A. (2020). Cubic splines to model relationships between continuous variables and outcomes: A guide for clinicians. Bone Marrow Transplantation, 55, 675–680. [DOI] [PubMed] [Google Scholar]
- 56. Garcia De Avila, M. , Hamamoto Filho, P. , Jacob, F. , Alcantara, L. , Berghammer, M. , Jenholt Nolbris, M. , Olaya‐Contreras, P. , & Nilsson, S. (2020). Children's anxiety and factors related to the COVID‐19 pandemic: An exploratory study using the Children's Anxiety Questionnaire and the Numerical Rating Scale. International Journal of Environmental Research and Public Health, 17, 5757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Baptista, A. S. , Prado, I. M. , Perazzo, M. F. , Pinho, T. , Paiva, S. M. , Pordeus, I. A. , & Serra‐Negra, J. M. (2021). Can children's oral hygiene and sleep routines be compromised during the COVID‐19 pandemic? International Journal of Paediatric Dentistry, 31, 12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chen, F. , Zheng, D. , Liu, J. , Gong, Y. , Guan, Z. , & Lou, D. (2020). Depression and anxiety among adolescents during COVID‐19: A cross‐sectional study. Brain, Behavior, and Immunity, 88, 36–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Chen, S. , Cheng, Z. , & Wu, J. (2020). Risk factors for adolescents’ mental health during the COVID‐19 pandemic: A comparison between Wuhan and other urban areas in China. Global Health, 16, 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Chen, Q. , Du, Y. , Zhu, H. , & Liu, X. F. (2020). Senior high school students’ mental status in home setting during COVID‐19 pandemic. China Journal of Health Psychology, 28, 1654–1660. [Google Scholar]
- 61. Crescentini, C. , Feruglio, S. , Matiz, A. , Paschetto, A. , Vidal, E. , Cogo, P. , & Fabbro, F. (2020). Stuck outside and inside: An exploratory study on the effects of the COVID‐19 outbreak on Italian parents and children's internalizing symptoms. Frontiers in Psychology, 11, 586074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Dai, X. R. , Liu, T. K. , & Liu, Y. W. (2020). Psychological status and influencing factors of high school students in Chengdu during the outbreak of COVID‐19. Modern Preventive Medicine, 47, 3911–3914. [Google Scholar]
- 63. Giannopoulou, I. , Efstathiou, V. , Triantafyllou, G. , Korkoliakou, P. , & Douzenis, A. (2021). Adding stress to the stressed: Senior high school students’ mental health amidst the COVID‐19 nationwide lockdown in Greece. Psychiatry Research, 295, 113560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. He, K. L. , Chen, X. G. , & Song, J. J. (2020). [The psychological impact of the novel coronavirus pneumonia epidemic on middle school students and suggestions]. Sichuan Education, 2020.04B, 11–13. [Google Scholar]
- 65. Hou, T.‐Y. , Mao, X.‐F. , Dong, W. , Cai, W.‐P. , & Deng, G.‐H. (2020). Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID‐19 outbreak. Asian Journal of Psychiatry, 54, 102305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Sama, B. K. , Kaur, P. , Thind, P. S. , Verma, M. K. , Kaur, M. , & Singh, D. D. (2021). Implications of COVID‐19‐induced nationwide lockdown on children's behaviour in Punjab, India. Child Care Health and Development, 47, 128–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Li, S. W. , Wang, Y. , Yang, Y. Y. , Lei, X. M. , & Yang, Y. F. (2020). Investigation on the influencing factors for anxiety related emotional disorders of children and adolescents with home quarantine during the prevalence of coronavirus disease 2019. Chinese Journal of Child Health Care, 28, 407–410. [Google Scholar]
- 68. Liu, G. , You, M. , & Lu, H. (2020). Impact of COVID‐19 pandemic on the mental health of high school seniors in Guangxi. Journal of Guangxi Medical University, 37, 1731–1734. [Google Scholar]
- 69. Lu, C. , Chi, X. , Liang, K. , Chen, S.‐T. , Huang, L. , Guo, T. , Jiao, C. , Yu, Q. , Veronese, N. , Soares, F. C. , Grabovac, I. , Yeung, A. , & Zou, L. (2020). Moving more and sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID‐19 pandemic. Psychology Research and Behavior Management, 13, 1223–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Mcguine, T. A. , Biese, K. M. , Petrovska, L. , Hetzel, S. J. , Reardon, C. , Kliethermes, S. , Bell, D. R. , Brooks, A. , & Watson, A. M. (2021). Mental health, physical activity, and quality of life of US adolescent athletes during COVID‐19‐related school closures and sport cancellations: A study of 13 000 athletes. Journal of Athletic Training, 56, 11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Mo, D. M. , Yan, J. W. , Li, X. , Guo, P. F. , Hu, S. W. , & Zhong, H. (2020). Prevalence rate and related influencing factors of anxiety disorder in children and adolescents during the outbreak of COVID‐19. Sichuan Mental Health, 33, 202–206. [Google Scholar]
- 72. Murata, S. , Rezeppa, T. , Thoma, B. , Marengo, L. , Krancevich, K. , Chiyka, E. , Hayes, B. , Goodfriend, E. , Deal, M. , Zhong, Y. , Brummit, B. , Coury, T. , Riston, S. , Brent, D. A. , & Melhem, N. M. (2021). The psychiatric sequelae of the COVID‐19 pandemic in adolescents, adults, and health care workers. Depression and Anxiety, 38, 233–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Qi, H. , Liu, R. , Chen, X. , Yuan, X. F. , Li, Y. Q. , Huang, H. H. , Zheng, Y. , & Wang, G. (2020). Prevalence of anxiety and associated factors for Chinese adolescents during the COVID‐19 outbreak. Psychiatry and Clinical Neurosciences, 74, 555–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Qi, M. , Zhou, S.‐J. , Guo, Z.‐C. , Zhang, L.‐G. , Min, H.‐J. , Li, X.‐M. , & Chen, J.‐X. (2020). The effect of social support on mental health in Chinese adolescents during the outbreak of COVID‐19. Journal of Adolescent Health, 67, 514–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Song, M. (2020). Investigation and suggestions on the physical and mental health of senior two students in our school during the period of epidemic prevention and control: A case study on grade 2021 students of Zunyi No.4 High School. Science & Education, 27, 168–170. [Google Scholar]
- 76. Su, C. L. , & Sun, Y. G. (2020). Psychological status and coping strategies of primary school students during the novel coronavirus epidemic. Mental Health Education in Primary and Secondary School, 452, 24–28. [Google Scholar]
- 77. Tang, L. , & Ying, B. (2020). Middle school students during the novel coronavirus pneumonia epidemic: Investigation and analysis of mental health status and influencing factors. Mental Health Education in Primary and Secondary School, 429, 57–61. [Google Scholar]
- 78. Tang, S. , & Pang, H. W. (2020). Anxiety and depression among children and adolescents during the COVID‐19 pandemic. Mental Health Education in Primary and Secondary School, 438, 15–18. [Google Scholar]
- 79. Tang, S. , Xiang, M. , Cheung, T. , & Xiang, Y.‐T. (2021). Mental health and its correlates among children and adolescents during COVID‐19 school closure: The importance of parent–child discussion. Journal of Affective Disorders, 279, 353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Wang, Y. , Yang, Y. Y. , Li, S. W. , Lei, X. M. , & Yang, Y. F. (2020). Investigation on the status and influencing factors for depression symptom of children and adolescents with home quarantine during the prevalence of novel coronavirus pneumonia. Chinese Journal of Child Health Care, 28, 277–280. [Google Scholar]
- 81. Wang, N. X. , & Xu, P. F. (2020). A survey of adolescents’ psychological stress and coping styles during the COVID‐19 epidemic. Journal of Dali University, 5, 123–128. [Google Scholar]
- 82. Wang, L. L. , & Sun, D. J. (2020). Investigation and research on anxiety status of middle school students in Beijing under the background of epidemic. Fundamental Education Forum, 26, 79–80. [Google Scholar]
- 83. Wang, P. P. , Zhang, C. , Zheng, Q. L. , Sun, F. , & Wang, G. H. (2020). Association study between screen exposure and sleep in home‐based junior high school students during the novel coronavirus pneumonia (COVID‐19) outbreak: A cross‐sectional survey. In Compilation of the 12th National Academic Annual Conference (pp. 153–154). China Sleep Research Society. [Google Scholar]
- 84. Xie, X. , Xue, Q. , Zhou, Y. , Zhu, K. , Liu, Q. , Zhang, J. , & Song, R. (2020). Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics, 174, 898–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Xue, Q. , Xie, X. , Liu, Q. , Zhou, Y. , Zhu, K. , Wu, H. , Wan, Z. , Feng, Y. , Meng, H. , Zhang, J. , Zuo, P. , & Song, R. (2021). Knowledge, attitudes, and practices towards COVID‐19 among primary school students in Hubei Province, China. Children and Youth Services Review, 120, 105735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Yu, Q. X. , Zeng, Y. M. , & Lu, W. J. (2020). Investigation and analysis on the mental health status of middle school students during the novel coronavirus pneumonia epidemic. Jiangsu Education, 32, 44–47. [Google Scholar]
- 87. Yue, J. , Zang, X. , Le, Y. , & An, Y. (2022). Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID‐19) outbreak in China. Current Psychology, 41, 5723–5730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Zhang, L. , Zhang, D. , Fang, J. , Wan, Y. , Tao, F. , & Sun, Y. (2020). Assessment of mental health of Chinese primary school students before and after school closing and opening during the COVID‐19 pandemic. JAMA Network Open, 3, e2021482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Zhang, X. M. , Yang, T. , Hu, Y. Q. , & Chen, Q. R. (2020). Investigation and analysis on the psychological status of junior high school students in Jiangyou area during the outbreak of novel coronavirus pneumonia. Baojian Wenhui, 29, 155–157. [Google Scholar]
- 90. Zhou, S.‐J. , Zhang, L.‐G. , Wang, L.‐L. , Guo, Z.‐C. , Wang, J.‐Q. , Chen, J.‐C. , Liu, M. , Chen, X. , & Chen, J.‐X. (2020). Prevalence and socio‐demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID‐19. European Child & Adolescent Psychiatry, 29, 749–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Zhou, J. , Yuan, X. , Qi, H. , Liu, R. , Li, Y. , Huang, H. , Chen, X. , & Wang, G. (2020). Prevalence of depression and its correlative factors among female adolescents in China during the coronavirus disease 2019 outbreak. Global Health, 16, 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Zhou, S.‐J. , Wang, L.‐L. , Yang, R. , Yang, X.‐J. , Zhang, L.‐G. , Guo, Z.‐C. , Chen, J.‐C. , Wang, J.‐Q. , & Chen, J.‐X. (2020). Sleep problems among Chinese adolescents and young adults during the coronavirus‐2019 pandemic. Sleep Medicine, 74, 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Zhou, R. , & Han, B. (2020). Investigation on the psychological status of junior high school students after returning to school and counseling countermeasures. Mental Health Education in Primary and Secondary School, 442, 72–75. [Google Scholar]
- 94. Zhu, K. H. , Zhou, Y. , Xie, X. Y. , Wu, H. , Xue, Q. , Liu, Q. , Wan, Z. H. , & Song, R. R. (2020). Anxiety symptom and its associates among primary school students in Hubei province during novel coronavirus disease 2019 epidemic. Chinese Journal of Public Health, 36, 673–676. [Google Scholar]
- 95. Cao, C. , Wang, L. , Fang, R. , Liu, P. , Bi, Y. , Luo, S. , Grace, E. , & Olff, M. (2022). Anxiety, depression, and PTSD symptoms among high school students in China in response to the COVID‐19 pandemic and lockdown. Journal of Affective Disorders, 296, 126–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Humer, E. , Dale, R. , Plener, P. L. , Probst, T. , & Pieh, C. (2021). Assessment of mental health of high school students 1 semester after COVID‐19‐associated remote schooling measures were lifted in Austria in 2021. JAMA Network Open, 4, e2135571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Pieh, C. , Plener, P. L. , Probst, T. , Dale, R. , & Humer, E. (2021). Assessment of mental health of high school students during social distancing and remote schooling during the COVID‐19 pandemic in Austria. JAMA Network Open, 4, e2114866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Jung, Y. H. , Jang, B. N. , Park, M. , & Park, E.‐C. (2022). Association between family financial decline due to COVID‐19 and generalized anxiety disorder among Korean adolescents. Journal of Affective Disorders, 309, 411–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Xu, Q. , Mao, Z. , Wei, D. , Fan, K. , Liu, P. , Wang, J. , Wang, X. , Lou, X. , Lin, H. , Wang, C. , & Wu, C. (2022). Association between mask wearing and anxiety symptoms during the outbreak of COVID 19: A large survey among 386,432 junior and senior high school students in China. Journal of Psychosomatic Research, 153, 110709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Liu, Y. , Yue, S. , Hu, X. , Zhu, J. , Wu, Z. , Wang, J. , & Wu, Y. (2021). Associations between feelings/behaviors during COVID‐19 pandemic lockdown and depression/anxiety after lockdown in a sample of Chinese children and adolescents. Journal of Affective Disorders, 284, 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Ghorbani, S. , Afshari, M. , Eckelt, M. , Dana, A. , & Bund, A. (2021). Associations between physical activity and mental health in Iranian adolescents during the COVID‐19 pandemic: An accelerometer‐based study. Children, 8, 1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wang, W. , Guo, Y. , Du, X. , Li, W. , Wu, R. , Guo, L. , & Lu, C. (2021). Associations between poor sleep quality, anxiety symptoms, and depressive symptoms among Chinese adolescents before and during COVID‐19: A longitudinal study. Frontiers in Psychiatry, 12, 786640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Kaman, A. , Otto, C. , Adedeji, A. , Devine, J. , Erhart, M. , Napp, A.‐K. , Becker, M. , Blanck‐Stellmacher, U. , Fertmann, R. , Saier, U. , & Ravens‐Sieberer, U. (2021). Belastungserleben und psychische Auffälligkeiten von Kindern und Jugendlichen in Hamburg während der COVID‐19‐pandemie. Nervenheilkunde, 40, 319–326. [Google Scholar]
- 104. Bazett‐Jones, D. M. , Garcia, M. C. , Taylor‐Haas, J. A. , Long, J. T. , Rauh, M. J. , Paterno, M. V. , & Ford, K. R. (2021). Changes in motivation, socialization, wellness and mental health in youth long‐distance runners during COVID‐19 social distancing restrictions. Frontiers in Sports and Active Living, 3, 696264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. O'Kane, S. M. , Lahart, I. M. , Gallagher, A. M. , Carlin, A. , Faulkner, M. , Jago, R. , & Murphy, M. H. (2021). Changes in physical activity, sleep, mental health, and social media use during COVID‐19 lockdown among adolescent girls: A mixed‐methods study. Journal of Physical Activity and Health, 18, 677–685. [DOI] [PubMed] [Google Scholar]
- 106. Alazzam, M. , Abuhammad, S. , Abdalrahim, A. , & Hamdan‐Mansour, A. M. (2021). Predictors of depression and anxiety among senior high school students during COVID‐19 pandemic: The context of home quarantine and online education. Journal of School Nursing, 37, 241–248. [DOI] [PubMed] [Google Scholar]
- 107. Albrecht, J. N. , Werner, H. , Rieger, N. , Jenni, O. G. , & Huber, R. (2022). Sleep and health‐related characteristics among adolescents during COVID‐19: An update. International Journal of Environmental Research and Public Health, 19, 5078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Alqassim, A. Y. , Mahfouz, M. S. , Hakami, M. M. , Al Faqih, A. A. , Shugairi, A. A. , Alsanosy, M. R. , Rayyani, A. Y. , Albrraq, A. Y. , Muaddi, M. A. , & Alharbi, A. A. (2022). Depression, anxiety, stress and their association with the use of electronic devices among adolescents during the COVID‐19 pandemic. International Journal of Mental Health Promotion, 24, 251–262. [Google Scholar]
- 109. Argiansya, F. , Soedjadhi, R. , Indra, R. M. , & Kesuma, Y. (2021). Electronic media use and sleep disorders among adolescents during the COVID‐19 pandemic. Sleep Disorders, 2021, 2096944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Becker, S. P. , Dvorsky, M. R. , Breaux, R. , Cusick, C. N. , Taylor, K. P. , & Langberg, J. M. (2021). Prospective examination of adolescent sleep patterns and behaviors before and during COVID‐19. Sleep, 44, zsab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Berki, T. , & Pikó, B. F. (2021). Sedentary lifestyle may contribute to the risk of depression during the COVID‐19 pandemic: A snapshot of Hungarian adolescents. European Journal of Mental Health, 16, 99–119. [Google Scholar]
- 112. Bhatta, A. , Kafley, R. K. , Yadav, A. , Phuyal, R. , & Chikanbanjar, V. K. (2021). Anxiety during COVID‐19 among school going adolescents of six private schools in Kathmandu Valley: A descriptive cross‐sectional study. Journal of Nepal Medical Association, 59, 231–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Black, S. R. , Evans, M. L. , Aaron, L. , Brabham, D. R. , & Kaplan, R. M. (2021). Covariance between parent and child symptoms before and during the COVID‐19 pandemic. Journal of Pediatric Psychology, 46, 1182–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Cao, Y. , Huang, L. , Si, T. , Wang, N. Q. , Qu, M. , & Zhang, X. Y. (2021). The role of only‐child status in the psychological impact of COVID‐19 on mental health of Chinese adolescents. Journal of Affective Disorders, 282, 316–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Castillo‐Martínez, M. , Castillo‐Martínez, M. , Ferrer, M. , & González‐Peris, S. (2022). Child and adolescent depression and other mental health issues during lockdown and SARS‐CoV‐2/COVID‐19 pandemic: A survey in school setting. Annals of Pediatrics, 96, 61–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Chen, X. , Qi, H. , Liu, R. , Feng, Y. , Li, W. , Xiang, M. , Cheung, T. , Jackson, T. , Wang, G. , & Xiang, Y.‐T. (2021). Depression, anxiety and associated factors among Chinese adolescents during the COVID‐19 outbreak: A comparison of two cross‐sectional studies. Translational Psychiatry, 11, 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Chi, X. , Liang, K. , Chen, S.‐T. , Huang, Q. , Huang, L. , Yu, Q. , Jiao, C. , Guo, T. , Stubbs, B. , Hossain, M. , Yeung, A. , Kong, Z. , & Zou, L. (2021). Mental health problems among Chinese adolescents during the COVID‐19: The importance of nutrition and physical activity. International Journal of Clinical and Health Psychology, 21, 100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Choukas‐Bradley, S. , Maheux, A. J. , Roberts, S. R. , Hutchinson, E. A. , Lu, C. , Ladouceur, C. D. , & Silk, J. S. (2022). Picture perfect during a pandemic? Body image concerns and depressive symptoms in U.S. adolescent girls during the COVID‐19 lockdown. Journal of Children and Media, 16, 481–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Denerel, N. , Şenışık, S. , Köyağasıoğlu, O. , Çiğdem, S. , & Tunç, S. (2021). Effects of long‐duration home isolation linked to the COVID‐19 pandemic on mental health of adolescent athletes. Pediatric Exercise Science, 33, 170–176. [DOI] [PubMed] [Google Scholar]
- 120. Ding, F. , Jia, Y. , Xiong, X. , Chen, P. , Xiong, S. , & Cheng, G. (2022). The protective role of parental involvement at home in negative psychological outcomes among Chinese adolescents during the COVID‐19 epidemic. Journal of Affective Disorders, 308, 123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Dönmez, Y. E. , & Uçur, Ö. (2021). Frequency of anxiety, depression, and irritability symptoms in children during the COVID‐19 outbreak and potential risk factors associated with these symptoms. Journal of Nervous and Mental Disease, 209, 727–733. [DOI] [PubMed] [Google Scholar]
- 122. El Refay, A. S. , Hashem, S. A. , Mostafa, H. H. , Kamel, I. H. , & Sherif, L. S. (2021). Sleep quality and anxiety symptoms in Egyptian children and adolescents during COVID‐19 pandemic lockdown. Bulletin of the National Research Centre, 45, 134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Fidancı, İ. , Aksoy, H. , Yengil Taci, D. , Fidancı, İ. , Ayhan Başer, D. , & Cankurtaran, M. (2021). Evaluation of the effect of the COVID‐19 pandemic on sleep disorders and nutrition in children. International Journal of Clinical Practice, 75, e14170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Fogarty, A. , Brown, S. , Gartland, D. , Mensah, F. , Seymour, M. , Savopoulos, P. , FitzPatrick, K. , Papadopoullos, S. , & Giallo, R. (2022). Psychosocial factors associated with adolescent depressive and anxiety symptoms during the COVID‐19 pandemic. International Journal of Behavioral Development, 46, 308–319. [Google Scholar]
- 125. Giannini, D. T. , Tavares, C. M. , Takey, M. , Aloise, M. L. R. , da Costa, A. J. , de Carvalho, D. S. , da Silva, S. C. , Pontes, M. H. P. , & Monteiro, C. B. (2022). Adolescents emotional state and behavioral and dietary habit changes during isolation due to the COVID‐19 pandemic. Journal of the American Nutrition Association, 41, 415–423. [DOI] [PubMed] [Google Scholar]
- 126. Forte, A. , Orri, M. , Brandizzi, M. , Iannaco, C. , Venturini, P. , Liberato, D. , Battaglia, C. , Nöthen‐Garunja, I. , Vulcan, M. , Brusìc, A. , Quadrana, L. , Cox, O. , Fabbri, S. , & Monducci, E. (2021). “My life during the lockdown”: Emotional experiences of European adolescents during the COVID‐19 crisis. International Journal of Environmental Research and Public Health, 18, 7638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Gladstone, T. R. G. , Schwartz, J. A. J. , Pössel, P. , Richer, A. M. , Buchholz, K. R. , & Rintell, L. S. (2022). Depressive symptoms among adolescents: Testing vulnerability‐stress and protective models in the context of COVID‐19. Child Psychiatry and Human Development, 53, 1372–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Glynn, L. M. , Davis, E. P. , Luby, J. L. , Baram, T. Z. , & Sandman, C. A. (2021). A predictable home environment may protect child mental health during the COVID‐19 pandemic. Neurobiology of Stress, 14, 100291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Guo, P. F. , Li, X. , Liu, S. , Hu, S. W. , Mo, D. M. , Yan, J. W. , Shen, X. S. , & Zhong, H. (2020). Status and influencing factors of anxiety among adolescents in Anhui during the epidemic of COVID‐19. Sichuan Mental Health, 33, 501–505. [Google Scholar]
- 130. Hamid, M. A. , Rahat Qureshi, A. , Kapoor, S. , Shabbir, W. , Arulchelvan, A. , Vanama, M. , Abdi, F. , & Gunaseelan, L. (2022). Mental health consequences of the COVID‐19 pandemic among Ontario's youth: A cross‐sectional study. Cureus, 14, e22526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Han, J. M. , & Song, H. (2021). Effect of subjective economic status during the COVID‐19 pandemic on depressive symptoms and suicidal ideation among South Korean adolescents. Psychology Research and Behavior Management, 14, 2035–2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. He, Y. , Li, X. S. , Zhao, J. , & An, Y. (2022). Family resilience, media exposure, and children's mental health in China during COVID‐19. Family Journal, 30, 579–588. [Google Scholar]
- 133. Hermosillo‐De‐La‐Torre, A. E. , Arteaga‐De‐Luna, S. M. , Acevedo‐Rojas, D. L. , Juárez‐Loya, A. , Jiménez‐Tapia, J. A. , Pedroza‐Cabrera, F. J. , González‐Forteza, C. , Cano, M. , & Wagner, F. A. (2021). Psychosocial correlates of suicidal behavior among adolescents under confinement due to the COVID‐19 pandemic in Aguascalientes, Mexico: A cross‐sectional population survey. International Journal of Environmental Research and Public Health, 18, 4977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Hertz, M. F. , Kilmer, G. , Verlenden, J. , Liddon, N. , Rasberry, C. N. , Barrios, L. C. , & Ethier, K. A. (2022). Adolescent mental health, connectedness, and mode of school instruction during COVID‐19. Journal of Adolescent Health, 70, 57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Hou, T. , Xie, Y. , Mao, X. , Liu, Y. , Zhang, J. , Wen, J. , Chen, Y. , Luo, Z. , & Cai, W. (2021). The mediating role of loneliness between social support and depressive symptoms among Chinese rural adolescents during COVID‐19 outbreak: A comparative study between left‐behind and non‐left‐behind students. Frontiers in Psychiatry, 12, 740094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Jenabi, E. , Bashirian, S. , Khazaei, S. , Poorsdavood, M. , Heidarimoghadam, R. , Barati, M. , Shirahmadi, S. , Zareian, S. , Shamsaei, F. , Farzian, S. , Asgari, A. , Nankali, Y. , & Haghighi, M. (2021). Rates of anxiety, depression, and stress among high school students during the COVID‐19 pandemic. Current Psychiatry Research and Reviews, 17, 98–104. [Google Scholar]
- 137. Kakaer, A. , Zhang, S. X. , Huang, S. Z. , Chen, Z. , Tan, K. Y. , Liang, J. H. , & Chen, Y. J. (2021). Emotional and behavioral problems and determinants among primary and middle school students aged 6 to 17‐year‐old in Guangdong Province during the COVID‐19 pandemic. Chinese Journal of School Health, 42, 1129–1134. [Google Scholar]
- 138. Kuty‐Pachecka, M. , Kozłowska, M. , Skórska, K. , Gucwa, K. , Trzebińska, M. , Stępień‐Grzelak, P. , & Żurawska, E. (2020). Anxiety, depression and health locus of control in secondary school students during the COVID‐19 pandemic. Psychiatria i Psychologia Kliniczna, 20, 219–233. [Google Scholar]
- 139. Lee, H. , Noh, Y. , Seo, J. , Park, S. H. , Kim, M. H. , & Won, S. (2021). Impact of the COVID‐19 pandemic on the mental health of adolescent students in Daegu, Korea. Journal of Korean Medical Science, 36, e321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Li, Y. , Zhou, Y. , Ru, T. , Niu, J. , He, M. , & Zhou, G. (2021). How does the COVID‐19 affect mental health and sleep among Chinese adolescents: A longitudinal follow‐up study. Sleep Medicine, 85, 246–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Li, M. , Li, L. , Wu, F. , Cao, Y. , Zhang, H. , Li, X. , Zou, J. , Guo, Z. , & Kong, L. (2021). Perceived family adaptability and cohesion and depressive symptoms: A comparison of adolescents and parents during COVID‐19 pandemic. Journal of Affective Disorders, 287, 255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Li, S. H. , Beames, J. R. , Newby, J. M. , Maston, K. , Christensen, H. , & Werner‐Seidler, A. (2022). The impact of COVID‐19 on the lives and mental health of Australian adolescents. European Child & Adolescent Psychiatry, 31, 1465–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Liang, Z. , Mazzeschi, C. , & Delvecchio, E. (2021). The impact of parental stress on Italian adolescents’ internalizing symptoms during the COVID‐19 pandemic: A longitudinal study. International Journal of Environmental Research and Public Health, 18, 8074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Liao, X. X. (2021). The impact of the 2019 novel coronavirus infection on sleep in children aged 2–12 (unpublished master's thesis). Chongqing Medical University, Chongqing, China.
- 145. Liao, X. X. , Chen, L. , Yang, T. , Chen, H. Y. , & Li, T. Y. (2022). Impact of 2019 novel coronavirus epidemic on sleep of children aged 2–12 years old. Chongqing Medicine, 51, 127–131. [Google Scholar]
- 146. Liu, S. S. , Chen, X. , Li, Y. Q. , Yuan, X. F. , Yu, H. Y. , & Fang, M. (2021). Investigation of depression and anxiety and their influencing factors among adolescents in Beijing during the coronavirus disease 2019 epidemic. Journal of Capital Medical University, 42, 412–417. [Google Scholar]
- 147. Liu, S. , Zou, S. , Zhang, D. , Wang, X. , & Wu, X. (2022). Problematic Internet use and academic engagement during the COVID‐19 lockdown: The indirect effects of depression, anxiety, and insomnia in early, middle, and late adolescence. Journal of Affective Disorders, 309, 9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Lu, T. , Yu, Y. , Zhao, Z. , & Guo, R. (2022). Mental health and related factors of adolescent students during coronavirus disease 2019 (COVID‐19) pandemic. Psychiatry Investigation, 19, 16–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Luijten, M. A. J. , Van Muilekom, M. M. , Teela, L. , Polderman, T. J. C. , Terwee, C. B. , Zijlmans, J. , Klaufus, L. , Popma, A. , Oostrom, K. J. , Van Oers, H. A. , & Haverman, L. (2021). The impact of lockdown during the COVID‐19 pandemic on mental and social health of children and adolescents. Quality of Life Research, 30, 2795–2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Ma, J. , Ding, J. , Hu, J. , Wang, K. , Xiao, S. , Luo, T. , Yu, S. , Liu, C. , Xu, Y. , Liu, Y. , Wang, C. , Guo, S. , Yang, X. , Song, H. , Geng, Y. , Jin, Y. , Chen, H. , & Liu, C. (2021). Children and adolescents’ psychological well‐being became worse in heavily hit Chinese Provinces during the COVID‐19 epidemic. Journal of Psychiatry and Brain Science, 6, e210020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Ma, Z. , Idris, S. , Zhang, Y. , Zewen, L. , Wali, A. , Ji, Y. , Pan, Q. , & Baloch, Z. (2021). The impact of COVID‐19 pandemic outbreak on education and mental health of Chinese children aged 7–15 years: An online survey. BMC Pediatrics, 21, 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Mansfield, K. L. , Newby, D. , Soneson, E. , Vaci, N. , Jindra, C. , Geulayov, G. , Gallacher, J. , & Fazel, M. (2021). COVID‐19 partial school closures and mental health problems: A cross‐sectional survey of 11,000 adolescents to determine those most at risk. JCPP Advances, 1, e12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Mcarthur, B. A. , Racine, N. , Mcdonald, S. , Tough, S. , & Madigan, S. (2021). Child and family factors associated with child mental health and well‐being during COVID‐19. European Child & Adolescent Psychiatry, Published ahead of print. 10.1007/s00787-021-01849-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Mcguine, T. A. , Biese, K. M. , Petrovska, L. , Hetzel, S. J. , Reardon, C. L. , Kliethermes, S. , Bell, D. R. , Brooks, A. , & Watson, A. M. (2021). Changes in the health of adolescent athletes: A comparison of health measures collected before and during the COVID‐19 pandemic. Journal of Athletic Training, 56, 836–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. McGuine, T. , Biese, K. , Hetzel, S. , Schwarz, A. , Reardon, C. , Bell, D. , Brooks, A. , Dickman, J. , & Watson, A. (2022). A multi‐year assessment of sport participation during the COVID‐19 pandemic on the health of adolescent athletes. Journal of Athletic Training, Published ahead of print. 10.4085/1062-6050-0679.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Mcguine, T. A. M. , Biese, K. , Hetzel, S. J. , Schwarz, A. , Kliethermes, S. , Reardon, C. L. , Bell, D. R. , Brooks, M. A. , & Watson, A. M. (2022). High school sports during the COVID‐19 pandemic: The effect of sport participation on the health of adolescents. Journal of Athletic Training, 57, 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Min, S.‐K. , Son, W.‐H. , Choi, B.‐H. , Lee, H.‐J. , Ahn, C.‐Y. , Yoo, J. , Park, S. , Lee, J.‐W. , & Jee, Y.‐S. (2021). Psychophysical condition of adolescents in coronavirus disease 2019. Journal of Exercise Rehabilitation, 17, 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Mohler‐Kuo, M. , Dzemaili, S. , Foster, S. , Werlen, L. , & Walitza, S. (2021). Stress and mental health among children/adolescents, their parents, and young adults during the first COVID‐19 lockdown in Switzerland. International Journal of Environmental Research and Public Health, 18, 4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Moitra, P. , & Madan, J. (2022). Impact of screen time during COVID‐19 on eating habits, physical activity, sleep, and depression symptoms: A cross‐sectional study in Indian adolescents. PLoS One, 17, e0264951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Monnier, M. , Moulin, F. , Thierry, X. , Vandentorren, S. , Côté, S. , Barbosa, S. , Falissard, B. , Plancoulaine, S. , Charles, M.‐A. , Simeon, T. , Geay, B. , Marchand, L. , Ancel, P.‐Y. , Melchior, M. , Rouquette, A. , Bajos, N. , Carrat, F. , Ancel, P.‐Y. , Charles, M.‐A. , … Galera, C. (2021). Children's mental and behavioral health, schooling, and socioeconomic characteristics during school closure in France due to COVID‐19: The SAPRIS project. Scientific Reports, 11, 22373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Nakachi, K. , Kawabe, K. , Hosokawa, R. , Yoshino, A. , Horiuchi, F. , & Ueno, S.‐I. (2021). Differences in psychological and behavioral changes between children following school closure due to COVID‐19. Psychiatry Journal, 2021, 5567732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Oliva, S. , Russo, G. , Gili, R. , Russo, L. , Di Mauro, A. , Spagnoli, A. , Alunni Fegatelli, D. , Romani, M. , Costa, A. , Veraldi, S. , & Manti, F. (2021). Risks and protective factors associated with mental health symptoms during COVID‐19 home confinement in Italian children and adolescents: The #Understandingkids Study. Frontiers in Pediatrics, 9, 664702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Orgilés, M. , Espada, J. P. , Delvecchio, E. , Francisco, R. , Mazzeschi, C. , Pedro, M. , & Morales, A. (2021). Anxiety and depressive symptoms in children and adolescents during COVID‐19 pandemic: A transcultural approach. Psicothema, 33, 125–130. [DOI] [PubMed] [Google Scholar]
- 164. Ozbaran, B. , Turer, F. , Yilancioglu, H. Y. , Kose, S. , Senturk Pilan, B. , Guzel, O. , Baskol, D. , Polat, F. , Bildik, T. , Sertoz, S. R. , Arda, B. , & Ozhan, M. H. (2022). COVID‐19‐related stigma and mental health of children and adolescents during pandemic. Clinical Child Psychology and Psychiatry, 27, 185–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Paiva, E. , da Silva, L. R. , Machado, M. E. D. , Aguiar, R. , Garcia, K. R. D. S. , & Acioly, P. G. A. M. (2021). Child behavior during the social distancing in the COVID‐19 pandemic. Revista Brasileira De Enfermagem, 74(1), e20200762. [DOI] [PubMed] [Google Scholar]
- 166. Peng, X. , Liang, S. , Liu, L. , Cai, C. , Chen, J. , Huang, A. , Wang, X. , & Zhao, J. (2022). Prevalence and associated factors of depression, anxiety and suicidality among Chinese high school E‐learning students during the COVID‐19 lockdown. Current Psychology, Published ahead of print. 10.1007/s12144-021-02512-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Pisano, S. , Catone, G. , Gritti, A. , Almerico, L. , Pezzella, A. , Santangelo, P. , Bravaccio, C. , Iuliano, R. , & Senese, V. P. (2021). Emotional symptoms and their related factors in adolescents during the acute phase of Covid‐19 outbreak in South Italy. Italian Journal of Pediatrics, 47, 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Pizarro‐Ruiz, J. P. , & Ordóñez‐Camblor, N. (2021). Effects of Covid‐19 confinement on the mental health of children and adolescents in Spain. Scientific Reports, 11, 11713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Puteikis, K. , Mameniškytė, A. , & Mameniškienė, R. (2022). Sleep quality, mental health and learning among high school students after reopening schools during the COVID‐19 pandemic: Results of a cross‐sectional online survey. International Journal of Environmental Research and Public Health, 19, 2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Qi, H. , Liu, R. , Feng, Y. , Luo, J. , Lei, S. , Cheung, T. , Ungvari, G. S. , Chen, X. , & Xiang, Y.‐T. (2021). Prevalence of depression and its associated factors among adolescents in China during the early stage of the COVID‐19 outbreak. PeerJ, 9, e12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Ravens‐Sieberer, U. , Kaman, A. , Erhart, M. , Otto, C. , Devine, J. , Löffler, C. , Hurrelmann, K. , Bullinger, M. , Barkmann, C. , Siegel, N. A. , Simon, A. M. , Wieler, L. H. , Schlack, R. , & Hölling, H. (2021). Quality of life and mental health in children and adolescents during the first year of the COVID‐19 pandemic: Results of a two‐wave nationwide population‐based study. European Child & Adolescent Psychiatry, Published ahead of print. 10.1007/s00787-021-01889-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Ren, Z. , Xin, Y. , Wang, Z. , Liu, D. , Ho, R. M. , & Ho, C. S. H. (2021). What factors are most closely associated with mood disorders in adolescents during the COVID‐19 pandemic? A cross‐sectional study based on 1,771 adolescents in Shandong Province, China. Frontiers in Psychiatry, 12, 728278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Sarvari, S. , Rahimzadeh, M. , Saei, S. M. , & Salehian, M. H. (2022). Do the adolescents’ physical activity and screen time during the COVID‐19 quarantine correlate to their upper extremity abnormalities and anxiety? International Journal of Pediatrics, 10, 15567–15576. [Google Scholar]
- 174. Selçuk, E. B. , Demir, A. Ç. , Erbay, L. G. , Özcan, Ö. Ö. , Gürer, H. , & Dönmez, Y. E. (2021). Anxiety, depression and post‐traumatic stress disorder symptoms in adolescents during the COVID‐19 outbreak and associated factors. International Journal of Clinical Practice, 75, e14880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. She, R. , Wong, K. , Lin, J. , Leung, K. , Zhang, Y. , & Yang, X. (2021). How COVID‐19 stress related to schooling and online learning affects adolescent depression and Internet gaming disorder: Testing Conservation of Resources theory with sex difference. Journal of Behavioral Addictions, 10, 953–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Siachpazidou, D. I. , Kotsiou, O. S. , Chatziparasidis, G. , Papagiannis, D. , Vavougios, G. D. , Gogou, E. , Stavrou, V. T. , & Gourgoulianis, K. I. (2021). Action and reaction of pre‐primary and primary school‐age children to restrictions during COVID‐19 pandemic in Greece. Journal of Personalized Medicine, 11, 451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Sicouri, G. , March, S. , Pellicano, E. , De Young, A. C. , Donovan, C. L. , Cobham, V. E. , Rowe, A. , Brett, S. , Russell, J. K. , Uhlman, L. , & Hudson, J. L. (2022). Mental health symptoms in children and adolescents during COVID‐19 in Australia. Australian and New Zealand Journal of Psychiatry, Published ahead of print. 10.1177/00048674221090174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Sifat, R. I. , Ruponty, M. M. , Rahim Shuvo, M. K. , Chowdhury, M. , & Suha, S. M. (2022). Impact of COVID‐19 pandemic on the mental health of school‐going adolescents: Insights from Dhaka city, Bangladesh. Heliyon, 8, e09223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. da Silva, B. B. L. , de Melo, M. C. F. , & Studart‐Pereira, L. M. (2022). Adolescents’ sleep quality during the COVID‐19 pandemic. Sleep Science, 15, 257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Spiratos, K. N. (2021). Problematic smartphone use among high school students and its relationships with depression, stress, self‐esteem, grit and academic performance (Doctoral thesis). Available from ProQuest Dissertations and Theses database. (UMI No. 28492117).
- 181. Stewart, T. M. , Fry, D. , Mcara, L. , Hamilton, S. , King, A. , Laurie, M. , & Mccluskey, G. (2022). Rates, perceptions and predictors of depression, anxiety and post traumatic stress disorder (PTSD)‐like symptoms about Covid‐19 in adolescents. PLoS One, 17, e0266818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Tamarit, A. , de la Barrera, U. , Mónaco, E. , Schoeps, K. , & Montoya‐Castilla, I. (2020). Psychological impact of COVID‐19 pandemic in Spanish adolescents: Risk and protective factors of emotional symptoms. Revista de Psicología Clínica con Niños y Adolescentes, 7, 73–80. [Google Scholar]
- 183. Teker, A. G. , & Yakşi, N. (2021). Factors affecting sleep quality in high school students and its relationship with nomophobia. Journal of Turkish Sleep Medicine, 8, 216–221. [Google Scholar]
- 184. Ustuner Top, F. , & Cam, H. H. (2022). Sleep disturbances in school‐aged children 6–12 years during the COVID‐19 pandemic in Turkey. Journal of Pediatric Nursing, 63, 125–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Türk, F. , Kul, A. , & Kilinç, E. (2021). Depression‐anxiety and coping strategies of adolescents during the Covid‐19 pandemic. Turkish Journal of Education, 10, 58–75. [Google Scholar]
- 186. Ursache, A. , Barajas‐Gonzalez, R. G. , Adhikari, S. , Kamboukos, D. , Brotman, L. M. , & Dawson‐Mcclure, S. (2022). A quasi‐experimental study of parent and child well‐being in families of color in the context of COVID‐19 related school closure. SSM Population Health, 17, 101053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Vaidya, R. , Kaza, S. K. , Gupta, P. , Weine, S. M. , Nooyi, S. C. , & Chaudhury, N. (2022). Depression, anxiety, and stress among Indian youth during the COVID‐19 lockdown – A cross‐sectional survey. Journal of Mental Health and Human Behaviour, 26, 153–160. [Google Scholar]
- 188. Valero‐Moreno, S. (2022). Impacto emocional y resiliencia en adolescentes de España y Ecuador durante la COVID‐19: Estudio transcultural. Revista de Psicología Clínica con Niños y Adolescentes, 9, 29–36. [Google Scholar]
- 189. Villanti, A. C. , LePine, S. E. , Peasley‐Miklus, C. , West, J. C. , Roemhildt, M. , Williams, R. , & Copeland, W. E. (2022). COVID‐related distress, mental health, and substance use in adolescents and young adults. Child and Adolescent Mental Health, 27, 138–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Vivechana, S. , & Bimala, P. (2021). Daily activities and anxiety among school going children during COVID 19 pandemic and school closure. International Journal of Caring Sciences, 14, 197–204. [Google Scholar]
- 191. Wang, P. Y. , Li, W. , Hu, Y. B. , Wang, G. H. , Jiang, F. , & Chen, J. (2021). Investigation on sleep problems and related factors in preschool children during home quarantine. Chinese Journal of Child Health Care, 29, 479–483. [Google Scholar]
- 192. Wang, Y. L. , Luo, Y. , Zhu, Y. , Xiao, D. W. , Mo, Y. S. , Li, H. , Liu, S. Q. , & Liu, C. (2021). Psychological and behavioral problems of school‐age children in Guizhou during COVID‐19 pandemic. Chinese Journal of Preventive Medicine, 22, 53–58. [Google Scholar]
- 193. Wang, L. , Yeerjiang, Y. , Gao, H. F. , Pei, J. F. , Zhang, R. X. , & Xu, W. H. (2022). Self‐reported anxiety level and related factors in senior high school students in China during the outbreak of coronavirus disease 2019. Journal of Affective Disorders, 301, 260–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Wearick‐Silva, L. E. , Richter, S. A. , Viola, T. W. , & Nunes, M. L. (2022). Sleep quality among parents and their children during COVID‐19 pandemic. Journal of Pediatrics, 98, 248–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Wen, F. , Meng, Y. , Liu, K. , Xia, J. , Li, H. , Qi, H. , Meng, K. , & Zhang, L. (2022). Depression among schoolchildren and adolescents aged 9–17 years during the outbreak of COVID‐19 in Beijing: A cross‐sectional online survey. Psychology, Health & Medicine, Published ahead of print. 10.1080/13548506.2022.2058029 [DOI] [PubMed] [Google Scholar]
- 196. Windiani, I. G. A. T. , Noviyani, N. M. R. , Adnyana, I. G. A. N. S. , Murti, N. L. S. P. , & Soetjiningsih, S. (2021). Prevalence of sleep disorders in adolescents and its relation with screen time during the COVID‐19 pandemic era. Journal of Medical Sciences, 9, 297–300. [Google Scholar]
- 197. Xie, X. , Liu, Q. , Zhu, K. , Jiang, Q. , Feng, Y. , Xiao, P. , Wu, X. , & Song, R. (2022). Psychological symptom progression in school‐aged children after COVID‐19 home confinement: A longitudinal study. Frontiers in Psychiatry, 13, 809107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Xu, Q. , Mao, Z. , Wei, D. , Liu, P. , Fan, K. , Wang, J. , Wang, X. , Lou, X. , Lin, H. , Wang, C. , & Wu, C. (2021). Prevalence and risk factors for anxiety symptoms during the outbreak of COVID‐19: A large survey among 373216 junior and senior high school students in China. Journal of Affective Disorders, 288, 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Yakşi, N. , Eroğlu, M. , & Özdemir, M. (2021). Covid‐19: Lise Öğrencilerinde Depresyon ve Anksiyetenin Prediktörleri. Cyprus Turkish Journal of Psychiatry & Psychology, 3, 192–202. [Google Scholar]
- 200. Yin, M. Y. , Li, J. H. , Huang, S. H. , Hong, Z. J. , Qin, G. L. , & Yi, Y. (2022). Analysis of mental health and influencing factors of middle school students in some areas of Guangxi. Health Vocational Education, 40, 146–149. [Google Scholar]
- 201. Zainel, A. A. , Qotba, H. , Al‐Maadeed, A. , Al‐Kohji, S. , Al Mujalli, H. , Ali, A. , Al Mannai, L. , Aladab, A. , Alsaadi, H. , Alkarbi, K. A. , & Al‐Baghdadi, T. (2021). Psychological and coping strategies related to home isolation and social distancing in children and adolescents during the COVID‐19 pandemic: Cross‐sectional study. JMIR Formative Research, 5, e24760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Zhai, X. , Zeng, J. , Eshak, E. S. , Zhang, Y. , Yang, M. , Di, L. , Xiang, B. , & Cao, J. (2021). The influencing factors of sleep quality among Chinese junior and senior high school adolescents during the COVID‐19 pandemic. Journal of Tropical Pediatrics, 67, fmab069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Zhan, N. , Zhang, Y. , Xie, D. , & Geng, F. (2022). The associations of parental COVID‐19 related worries, lifestyles, and insomnia with child insomnia during the COVID‐19 outbreak. Journal of Sleep Research, 31, e13590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Zhang, Z. , Zhai, A. , Yang, M. , Zhang, J. , Zhou, H. , Yang, C. , Duan, S. , & Zhou, C. (2020). Prevalence of depression and anxiety symptoms of high school students in Shandong Province during the COVID‐19 epidemic. Frontiers in Psychiatry, 11, 570096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Zhang, X. , Yang, H. , Zhang, J. , Yang, M. , Yuan, N. , & Liu, J. (2021). Prevalence of and risk factors for depressive and anxiety symptoms in a large sample of Chinese adolescents in the post‐COVID‐19 era. Child and Adolescent Psychiatry and Mental Health, 15, 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Zhang, Y. , Zhan, N. , Zou, J. , Xie, D. , Liu, M. , & Geng, F. (2022). The transmission of psychological distress and lifestyles from parents to children during COVID‐19. Journal of Affective Disorders, 303, 74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Zhao, J. , Xu, J. , He, Y. , & Xiang, M. (2022). Children and adolescents’ sleep patterns and their associations with mental health during the COVID‐19 pandemic in Shanghai, China. Journal of Affective Disorders, 301, 337–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Zhen, R. , & Zhou, X. (2022). Latent patterns of posttraumatic stress symptoms, depression, and posttraumatic growth among adolescents during the COVID‐19 pandemic. Journal of Traumatic Stress, 35, 197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Zhong, H. P. , Zhou, C. M. , & Wang, C. C. (2021). Investigation of anxiety symptom in children and adolescents during COVID‐19 epidemic. China Standardization, 591, 128–131. [Google Scholar]
- 210. Zhou, C. , Li, R. , Yang, M. , Duan, S. , & Yang, C. (2021). Psychological status of high school students 1 year after the COVID‐19 emergency. Frontiers in Psychiatry, 12, 729930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Zhu, J. , Li, J. , Yue, S. , Liu, M. , Gu, M. Y. , Li, X. M. , Zhang, D. , Li, Y. R. , Liu, D. B. , & Liu, Y. (2021). Correlated factors of depression in children and adolescents during the COVID‐19 pandemic. Journal of Jining Medical College, 44, 398–402. [Google Scholar]
- 212. Bani‐Issa, W. , Radwan, H. , Saqan, R. , Hijazi, H. , Fakhry, R. , Alameddine, M. , Naja, F. , Ibrahim, A. , Lin, N. , Naing, Y. T. , & Awad, M. (2022). Association between quality of sleep and screen time during the COVID‐19 outbreak among adolescents in the United Arab Emirates. Journal of Sleep Research, Published ahead of print. 10.1111/jsr.13666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Håkansson, A. , Moesch, K. , & Kenttä, G. (2022). COVID‐19‐related impact on mental health and career uncertainty in student‐athletes—Data from a cohort of 7,025 athletes in an elite sport high school system in Sweden. Frontiers in Sports and Active Living, 4, 943402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Deb, S. , Kar, S. , Deb, S. , Biswas, S. , Ahmad Dar, A. , & Mukherjee, T. (2022). A cross‐sectional study on mental health of school students during the COVID‐19 pandemic in India. Data, 7, 99. [Google Scholar]
- 215. Adams, D. P. , Holt, J. R. , Martin, J. A. , Houpy, D. M. , & Hollenbach, K. A. (2022). The effect of COVID‐19 lockdown on PHQ depression screening scores for high school athletes. International Journal of Environmental Research and Public Health, 19, 9943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Molu, B. , Taşdelen Baş, M. , & Özpulat, F. (2022). The effect of digital screen exposure and temperament on sleep problems in children during the COVID‐19 pandemic: Rural area in Turkey. Journal of Turkish Sleep Medicine, 9, 157–164. [Google Scholar]
- 217. Tural Büyük, E. , & Öztürk Savaş, Z. (2022). Effect of internet addiction on the sleep quality of adolescents during COVID‐19 pandemia duration period. Journal of Turkish Sleep Medicine, 9, 232–237. [Google Scholar]
- 218. Curatola, A. , Ferretti, S. , Gatto, A. , Valentini, P. , Giugno, G. , Della Marca, G. , Brunetti, V. , & Lazzareschi, I. (2022). The effects of COVID‐19 pandemic on Italian school‐aged children: Sleep‐related difficulties and trauma reactions. Journal of Child Neurology, 37, 568–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Kim, H. , Jhon, M. , Kim, J.‐W. , Kang, H.‐J. , Ryu, S. , Kim, J.‐M. , Lee, J.‐Y. , & Kim, S.‐W. (2022). Factors associated with depression and anxiety in Korean adolescents during the COVID‐19 pandemic. Psychiatry Investigation, 19, 551–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Lee, K.‐S. , Sung, H. K. , Lee, S. H. , Hyun, J. , Kim, H. , Lee, J.‐S. , Paik, J.‐W. , Kim, S.‐J. , Sohn, S. , & Choi, Y.‐K. (2022). Factors related to anxiety and depression among adolescents during COVID‐19: A web‐based cross‐sectional survey. Journal of Korean Medical Science, 37, e199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Magklara, K. , Lazaratou, H. , Barbouni, A. , Poulas, K. , & Farsalinos, K. (2022). The impact of COVID‐19 lockdown on children's and adolescents' mental health in Greece. Children & Society, Published ahead of print. 10.1111/chso.12605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Mcguine, T. , Biese, K. , Schwarz, A. , Dickman, J. , Hetzel, S. , Reardon, C. , & Watson, A. (2022). The impact of sport particiaption on the health of adolescents during the CoVID‐19 pandemic. Orthopaedic Journal of Sports Medicine, 10. 10.1177/2325967121S00426 [DOI] [Google Scholar]
- 223. Lee, J. , Ko, Y.‐H. , Chi, S. , Lee, M.‐S. , & Yoon, H.‐K. (2022). Impact of the COVID‐19 pandemic on Korean adolescents’ mental health and lifestyle factors. Journal of Adolescent Health, 71, 270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Fischer, K. , Tieskens, J. M. , Luijten, M. A. J. , Zijlmans, J. , Van Oers, H. A. , De Groot, R. , Van Der Doelen, D. L. , Van Ewijk, H. , Klip, H. , Van Der Lans, R. M. , De Meyer, R. , Van Der Mheen, M. , Van Muilekom, M. M. , Hyun Ruisch, I. , Teela, L. , Van Den Berg, G. , Bruining, H. , Van Der Rijken, R. , Buitelaar, J. , … Popma, A. (2022). Internalizing problems before and during the COVID‐19 pandemic in independent samples of Dutch children and adolescents with and without pre‐existing mental health problems. European Child & Adolescent Psychiatry, Published ahead of print. 10.1007/s00787-022-01991-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Dale, R. , Jesser, A. , Pieh, C. , O'Rourke, T., Probst, T. , & Humer, E. (2022). Mental health burden of high school students, and suggestions for psychosocial support, 1.5 years into the COVID‐19 pandemic in Austria. European Child & Adolescent Psychiatry, Published ahead of print. 10.1007/s00787-022-02032-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Jin, M. , Ding, L. , Fan, J. , Sheng, X. , Luo, B. , Hang, R. , Feng, L. , & Huang, L. (2022). Moderating role of resilience between depression and stress response of vocational middle school students during the COVID‐19 pandemic. Frontiers in Psychiatry, 13, 904592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Arazi, L. C. , García, M. , Salvatierra, D. B. , Nova, S. V. , Mello, F. C. , Garrido, M. , Smitarello, A. , & Alberti, A. (2022). Mood, emotions, and behaviors of children during the COVID‐19 pandemic in Autonomous City of Buenos Aires. Archivos Argentinos De Pediatria, 120, 106–110. [DOI] [PubMed] [Google Scholar]
- 228. Wesley, K. L. , Cooper, E. H. , Brinton, J. T. , Meier, M. , Honaker, S. , & Simon, S. L. (2022). A national survey of U.S. adolescent sleep duration, timing, and social jetlag during the COVID‐19 pandemic. Behavioral Sleep Medicine, Published ahead of print. 10.1080/15402002.2022.2086871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Leon Rojas, D. , Castorena Torres, F. , Garza‐Ornelas, B. M. , Castillo Tarquino, A. M. , Salinas Silva, C. A. , Almanza Chanona, J. L. , & Rodríguez‐de‐Ita, J. (2022). Parents and school‐aged children's mental well‐being after prolonged school closures and confinement during the COVID‐19 pandemic in Mexico: A cross‐sectional online survey study. BMJ Paediatrics Open, 6, e001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. Jeelani, A. , Dkhar, S. A. , Quansar, R. , & Khan, S. M. S. (2022). Prevalence of depression and anxiety among school‐going adolescents in Indian Kashmir valley during COVID‐19 pandemic. Middle East Current Psychiatry, 29, 18. [Google Scholar]
- 231. Alnamnakani, M. , Alenezi, S. , Temsah, H. , Alothman, M. , Murshid, R. E. , Alonazy, H. , & Alqurashi, H. (2022). Psychosocial impact of lockdown on children due to COVID‐19: A cross‐sectional study. Clinical Practice and Epidemiology in Mental Health, 18. 10.2174/17450179-v18-e2203210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Koyuncu, Z. , Gokler, M. E. , Secen Yazici, M. , Can Aydin, A. B. , Adiyaman, F. , Tarakcioglu, M. C. , Kadak, M. T. , & Erdogan, F. (2022). Relationship of sleep disturbances in children with depression/anxiety symptoms in children and their parents during the covid‐19 pandemic. Neuropsychiatric Investigation, 60, 42–48. [Google Scholar]
- 233. Janousch, C. , Anyan, F. , Morote, R. , & Hjemdal, O. (2022). Resilience patterns of Swiss adolescents before and during the COVID‐19 pandemic: A latent transition analysis. International Journal of Adolescence and Youth, 27, 294–314. [Google Scholar]
- 234. Lee, B. , & Hong, J. S. (2022). Short‐ and long‐term impacts of the COVID‐19 pandemic on suicide‐related mental health in Korean adolescents. International Journal of Environmental Research and Public Health, 19, 11491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Kim, D. H. , Kim, B. , Jang, S.‐Y. , Lee, S. G. , & Kim, T. H. (2022). Sleep and mental health among adolescents during the COVID‐19 pandemic. Psychiatry Investigation, 19, 637–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Chi, S. , Ko, M.‐S. , Lee, J.‐H. , Yi, H.‐S. , & Lee, M.‐S. (2022). Smartphone usage and sleep quality in Korean middle school students during the COVID‐19 pandemic. Psychiatry Investigation, 19, 722–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Liu, Y. , Hu, J. , & Liu, J. (2022). Social support and depressive symptoms among adolescents during the COVID‐19 pandemic: The mediating roles of loneliness and meaning in life. Frontiers in Public Health, 10, 916898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238. Adegboye, D. , Lennon, J. , Batterbee, O. , Thapar, A. , Collishaw, S. , Shelton, K. , Langley, K. , Hobson, C. , Higgins, A. , & Van Goozen, S. (2022). Understanding de novo onset of anxiety during COVID‐19: Pre‐pandemic socio‐emotional functioning in vulnerable children. JCPP Advances, 2, e12076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Mactavish, A. , Mastronardi, C. , Menna, R. , Babb, K. A. , Battaglia, M. , Amstadter, A. B. , & Rappaport, L. M. (2021). Children's mental health in Southwestern Ontario during summer 2020 of the COVID‐19 pandemic. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 30, 177–190. [PMC free article] [PubMed] [Google Scholar]
- 240. Asanov, I. , Flores, F. , Mckenzie, D. , Mensmann, M. , & Schulte, M. (2021). Remote‐learning, time‐use, and mental health of Ecuadorian high‐school students during the COVID‐19 quarantine. World Development, 138, 105225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241. Cheah, C. S. L. , Wang, C. , Ren, H. , Zong, X. , Cho, H. S. , & Xue, X. (2020). COVID‐19 racism and mental health in Chinese American families. Pediatrics, 146, e2020021816. [DOI] [PubMed] [Google Scholar]
- 242. Li, W. , Zhang, Y. , Wang, J. , Ozaki, A. , Wang, Q. , Chen, Y. , & Jiang, Q. (2021). Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID‐19 pandemic. JAMA Pediatrics, 175, 313–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Luthar, S. S. , Ebbert, A. M. , & Kumar, N. L. (2021). Risk and resilience during COVID‐19: A new study in the Zigler paradigm of developmental science. Development and Psychopathology, 33, 565–580. [DOI] [PubMed] [Google Scholar]
- 244. Zhang, C. , Ye, M. , Fu, Y. , Yang, M. , Luo, F. , Yuan, J. , & Tao, Q. (2020). The psychological impact of the COVID‐19 pandemic on teenagers in China. Journal of Adolescent Health, 67, 747–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Hossain, M. , & Purohit, N. (2019). Improving child and adolescent mental health in India: Status, services, policies, and way forward. Indian Journal of Psychiatry, 61, 415–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Reiss, F. , Meyrose, A.‐K. , Otto, C. , Lampert, T. , Klasen, F. , & Ravens‐Sieberer, U. (2019). Socioeconomic status, stressful life situations and mental health problems in children and adolescents: Results of the German BELLA cohort‐study. PLoS One, 14, e0213700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Golberstein, E. , Gonzales, G. , & Meara, E. (2019). How do economic downturns affect the mental health of children? Evidence from the National Health Interview Survey. Health Economics, 28, 955–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Gariepy, G. , Elgar, F. J. , Sentenac, M. , & Barrington‐Leigh, C. (2017). Early‐life family income and subjective well‐being in adolescents. PLoS One, 12, e0179380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Persaud, A. , Day, G. , Gupta, S. , Ventriglio, A. , Ruiz, R. , Chumakov, E. , Desai, G. , Castaldelli‐Maia, J. , Torales, J. , Juan Tolentino, E. , Bhui, K. , & Bhugra, D. (2018). Geopolitical factors and mental health I. International Journal of Social Psychiatry, 64, 778–785. [DOI] [PubMed] [Google Scholar]
- 250. Liu, F. , Zhou, N. , Cao, H. , Fang, X. , Deng, L. , Chen, W. , Lin, X. , Liu, L. , & Zhao, H. (2017). Chinese college freshmen's mental health problems and their subsequent help‐seeking behaviors: A cohort design (2005–2011). PLoS One, 12, e0185531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251. Parker, G. , Gladstone, G. , & Chee, K. T. (2001). Depression in the planet's largest ethnic group: The Chinese. American Journal of Psychiatry, 158, 857–864. [DOI] [PubMed] [Google Scholar]
- 252. Subramaniam, M. , Abdin, E. , Picco, L. , Pang, S. , Shafie, S. , Vaingankar, J. A. , Kwok, K. W. , Verma, K. , & Chong, S. A. (2017). Stigma towards people with mental disorders and its components ‐ A perspective from multi‐ethnic Singapore. Epidemiology and Psychiatric Sciences, 26, 371–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253. Zhang, Z. , Sun, K. , Jatchavala, C. , Koh, J. , Chia, Y. , Bose, J. , Li, Z. , Tan, W. , Wang, S. , Chu, W. , Wang, J. , Tran, B. , & Ho, R. (2019). Overview of stigma against psychiatric illnesses and advancements of anti‐stigma activities in six Asian societies. International Journal of Environmental Research and Public Health, 17, 280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Yu, M. , Cheng, S. , Fung, K. P.‐L. , Wong, J. P. , & Jia, C. (2022). More than mental illness: Experiences of associating with stigma of mental illness for Chinese college students. International Journal of Environmental Research and Public Health, 19, 864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255. Xu, Z. , Huang, F. , Kösters, M. , & Rüsch, N. (2017). Challenging mental health related stigma in China: Systematic review and meta‐analysis. II. Interventions among people with mental illness. Psychiatry Research, 255, 457–464. [DOI] [PubMed] [Google Scholar]
- 256. Yin, H. , Wardenaar, K. J. , Xu, G. , Tian, H. , & Schoevers, R. A. (2019). Help‐seeking behaviors among Chinese people with mental disorders: A cross‐sectional study. BMC Psychiatry, 19, 373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Yin, H. , Wardenaar, K. J. , Xu, G. , Tian, H. , & Schoevers, R. A. (2020). Mental health stigma and mental health knowledge in Chinese population: A cross‐sectional study. BMC Psychiatry, 20, 323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Fink, E. , Patalay, P. , Sharpe, H. , Holley, S. , Deighton, J. , & Wolpert, M. (2015). Mental health difficulties in early adolescence: A comparison of two cross‐sectional studies in England from 2009 to 2014. Journal of Adolescent Health, 56, 502–507. [DOI] [PubMed] [Google Scholar]
- 259. Yoon, Y. , Eisenstadt, M. , Lereya, S. T. , & Deighton, J. (2022). Gender difference in the change of adolescents’ mental health and subjective wellbeing trajectories. European Child & Adolescent Psychiatry, Published ahead of print. 10.1007/s00787-022-01961-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Van Droogenbroeck, F. , Spruyt, B. , & Keppens, G. (2018). Gender differences in mental health problems among adolescents and the role of social support: Results from the Belgian health interview surveys 2008 and 2013. BMC Psychiatry, 18, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Patel, V. , Flisher, A. J. , Hetrick, S. , & Mcgorry, P. (2007). Mental health of young people: A global public‐health challenge. Lancet, 369, 1302–1313. [DOI] [PubMed] [Google Scholar]
- 262. Matud, M. P. (2004). Gender differences in stress and coping styles. Personality and Individual Differences, 37, 1401–1415. [Google Scholar]
- 263. Evans, D. , Borriello, G. A. , & Field, A. P. (2018). A review of the academic and psychological impact of the transition to secondary education. Frontiers in Psychology, 9, 1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264. Abuhammad, S. (2020). Barriers to distance learning during the COVID‐19 outbreak: A qualitative review from parents’ perspective. Heliyon, 6, e05482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Impact of media use on children and youth. (2003). Paediatrics and Child Health, 8, 301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266. Rocha, Y. M. , de Moura, G. A. , Desidério, G. A. , de Oliveira, C. H. , Lourenço, F. D. , & de Figueiredo Nicolete, L. D. (2021). The impact of fake news on social media and its influence on health during the COVID‐19 pandemic: A systematic review. Journal of Public Health, Published ahead of print. 10.1007/s10389-021-01658-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267. Marciano, L. , Ostroumova, M. , Schulz, P. J. , & Camerini, A. L. (2021). Digital media use and adolescents’ mental health during the Covid‐19 pandemic: A systematic review and meta‐analysis. Frontiers in Public Health, 9, 793868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Hale, L. , Kirschen, G. W. , LeBourgeois, M. K. , Gradisar, M. , Garrison, M. M. , Montgomery‐Downs, H. , Kirschen, H. , McHale, S. M. , Chang, A. M. , & Buxton, O. M. (2018). Youth screen media habits and sleep: Sleep‐friendly screen behavior recommendations for clinicians, educators, and parents. Child and Adolescent Psychiatric Clinics of North America, 27, 229–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Liu, H. , Liu, W. , Yoganathan, V. , & Osburg, V.‐S. (2021). COVID‐19 information overload and generation Z's social media discontinuance intention during the pandemic lockdown. Technological Forecasting and Social Change, 166, 120600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270. Hudimova, A. , Popovych, I. , Baidyk, V. , Buriak, O. , & Kechyk, O. (2021). The impact of social media on young web users’ psychological well‐being during the COVID‐19 pandemic progression. Revista Amazonia Investiga, 10, 50–61. [Google Scholar]
- 271. Vall‐Roqué, H. , Andrés, A. , & Saldaña, C. (2021). The impact of COVID‐19 lockdown on social network sites use, body image disturbances and self‐esteem among adolescent and young women. Progress in Neuro‐Psychopharmacology & Biological Psychiatry, 110, 110293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272. Foerster, M. , Henneke, A. , Chetty‐Mhlanga, S. , & Röösli, M. (2019). Impact of adolescents’ screen time and nocturnal mobile phone‐related awakenings on sleep and general health symptoms: A prospective cohort study. International Journal of Environmental Research and Public Health, 16, 518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Schueller, S. M. , Stiles‐Shields, C. , & Yarosh, L. (2017). Online treatment and virtual therapists in child and adolescent psychiatry. Child and Adolescent Psychiatric Clinics of North America, 26, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Dray, J. , Bowman, J. , Campbell, E. , Freund, M. , Wolfenden, L. , Hodder, R. K. , Mcelwaine, K. , Tremain, D. , Bartlem, K. , Bailey, J. , Small, T. , Palazzi, K. , Oldmeadow, C. , & Wiggers, J. (2017). Systematic review of universal resilience‐focused interventions targeting child and adolescent mental health in the school setting. Journal of the American Academy of Child and Adolescent Psychiatry, 56, 813–824. [DOI] [PubMed] [Google Scholar]
- 275. Chung, Y. , & Huang, H.‐H. (2021). Cognitive‐based interventions break gender stereotypes in kindergarten children. International Journal of Environmental Research and Public Health, 18, 13052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Eller, T. , Aluoja, A. , Vasar, V. , & Veldi, M. (2006). Symptoms of anxiety and depression in Estonian medical students with sleep problems. Depression and Anxiety, 23, 250–256. [DOI] [PubMed] [Google Scholar]
- 277. Ohayon, M. M. , Caulet, M. , Priest, R. G. , & Guilleminault, C. (1997). DSM‐IV and ICSD‐90 insomnia symptoms and sleep dissatisfaction. British Journal of Psychiatry, 171, 382–388. [DOI] [PubMed] [Google Scholar]
- 278. Tarokh, L. , Saletin, J. M. , & Carskadon, M. A. (2016). Sleep in adolescence: Physiology, cognition and mental health. Neuroscience and Biobehavioral Reviews, 70, 182–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279. Loayza, H. M. P. , Ponte, T. S. , Carvalho, C. G. , Pedrotti, M. R. , Nunes, P. V. , Souza, C. M. , Zanette, C. B. , Voltolini, S. , & Chaves, M. L. F. (2001). Association between mental health screening by self‐report questionnaire and insomnia in medical students. Arquivos De Neuro‐Psiquiatria, 59, 180–185. [DOI] [PubMed] [Google Scholar]
- 280. Christakis, D. A. , Van Cleve, W. , & Zimmerman, F. J. (2020). Estimation of US children's educational attainment and years of life lost associated with primary school closures during the coronavirus disease 2019 pandemic. JAMA Network Open, 3, e2028786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Baker, W. L. , Michael White, C. , Cappelleri, J. C. , Kluger, J. , & Coleman, C. I. (2009). Understanding heterogeneity in meta‐analysis: The role of meta‐regression. International Journal of Clinical Practice, 63, 1426–1434. [DOI] [PubMed] [Google Scholar]
- 282. Pierce, M. , Mcmanus, S. , Jessop, C. , John, A. , Hotopf, M. , Ford, T. , Hatch, S. , Wessely, S. , & Abel, K. M. (2020). Says who? The significance of sampling in mental health surveys during COVID‐19. Lancet Psychiatry, 7, 567–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1: Forest plot for the prevalence pooling of depressive symptoms
Figure S2: Forest plot for the subgroup analysis of depressive symptoms by screening tools and threshold values
Figure S3: Funnel plot for the meta‐analysis of depressive symptom prevalence
Figure S4: Forest plot for the prevalence pooling of anxiety symptoms
Figure S5: Forest plot for the subgroup analysis of anxiety symptoms by screening tools and threshold values
Figure S6: Funnel plot for the meta‐analysis of anxiety symptom prevalence
Figure S7: Forest plot for the prevalence pooling of sleep disturbances
Figure S8: Funnel plot for the meta‐analysis of sleep disturbance prevalence
Figure S9: Forest plot for the subgroup analysis of sleep disturbances by screening tools and threshold values
Figure S10: Forest plot for the subgroup analysis of depressive symptoms by geographical regions
Figure S11: Forest plot for the subgroup analysis of anxiety symptoms by geographical regions
Figure S12: Forest plot for the subgroup analysis of sleep disturbances by geographical regions
Figure S13: Forest plot for the subgroup analysis of depressive symptoms by education level
Figure S14: Forest plot for the subgroup analysis of anxiety symptoms by education level
Figure S15: Forest plot for the subgroup analysis of depressive symptoms by gender
Figure S16: Forest plot for the subgroup analysis of anxiety symptoms by gender
Figure S17: Forest plot for the subgroup analysis of depressive symptoms by electronics usage
Figure S18: Forest plot for the subgroup analysis of anxiety symptoms by electronics usage
Table S1: Preferred reporting items for systematic reviews and meta‐analyses (PRISMA 2020) checklist
Table S2: MEDLINE search strategy
Table S3: EMBASE search strategy
Table S4: APA PsycInfo search strategy
Table S5: PubMed search strategy
Table S6: China National Knowledge Infrastructure (CNKI) search strategy
Table S7: Web of Science Core Collection search strategy
Table S8: CINAHL search strategy
Table S9: Characteristics of included studies and patients
Table S10: Risk of bias ratings
Table S11: Subgroup definition for high electronics use
Table S12: Subgroup definition for high physical activity
Table S13: Subgroup definition for financial difficulty
Data Availability Statement
Data involved in statistical analyses are disclosed in the manuscript, figures, tables, and supplementary materials. Please contact the corresponding author for additional inquiries.


