Abstract
Accurate and timely tracking of COVID-19 deaths is essential to a well-functioning public health surveillance system. The extent to which official COVID-19 death tallies have captured the true toll of the pandemic in the United States is unknown. In the current study, we develop a Bayesian hierarchical model to estimate monthly excess mortality in each county over the first two years of the pandemic and compare these estimates to the number of deaths officially attributed to Covid-19 on death certificates. Overall, we estimated that 268,176 excess deaths were not reported as Covid-19 deaths during the first two years of the Covid-19 pandemic, which represented 23.7% of all excess deaths that occurred. Differences between excess deaths and reported COVID-19 deaths were substantial in both the first and second year of the pandemic. Excess deaths were less likely to be reported as COVID-19 deaths in the Mountain division, in the South, and in nonmetro counties. The number of excess deaths exceeded COVID-19 deaths in all Census divisions except for the New England and Middle Atlantic divisions where there were more COVID-19 deaths than excess deaths in large metro areas and medium or small metro areas. Increases in excess deaths not assigned to COVID-19 followed similar patterns over time to increases in reported COVID-19 deaths and typically preceded or occurred concurrently with increases in reported COVID-19 deaths. Estimates from this study can be used to inform targeting of resources to areas in which the true toll of the COVID-19 pandemic has been underestimated.
Introduction
Excess mortality is a measure that has been widely used to assess the mortality impact of the COVID-19 pandemic.1 Excess mortality refers to the difference between the observed number of deaths that occurred during a given period and the number of deaths that would be expected based on mortality trends prior to the period.2 Prior estimates reveal that more than 1.1 million excess deaths occurred in the United States during the first two years of the pandemic, with approximately 620,000 occurring in the first year and 540,000 occurring in the second year.3 Most studies have found that the number of excess deaths substantially exceeded the number of deaths assigned to COVID-19 on death certificates.4–8 While a large body of research has investigated the spatial and temporal patterning of deaths assigned to COVID-19 and excess deaths during the pandemic,4,5,9–11 less attention has been given to how excess deaths not assigned to COVID-19 have been dispersed across the U.S.
Excess deaths not assigned to COVID-19 are deaths above those expected based on pre-pandemic trends that were not attributed to COVID-19 on death certificates.12,13 There are several reasons why excess deaths may not be assigned to COVID-19. First, the death may have been directly related to COVID-19 but unrecognized as a COVID-19 death by the certifier.14 This could occur due to a lack of COVID-19 testing before death, a lack of post-mortem COVID-19 testing due to limited death investigation resources, or resistance to assigning the death to COVID-19 from the deceased’s family or the death certifier as a result of personal or political beliefs.15,16 It could also relate to difficulty with assignment resulting from atypical presentations of COVID-19 symptoms or the presence of multiple comorbidities.17,18 Second, the death could be indirectly related to the pandemic as a result of health care interruptions or delays in health care that occurred especially during periods when COVID-19 cases increased and hospitals were overcrowded with COVID-19 patients.19,20 Lastly, the death could be indirectly related to the pandemic through the social and economic consequences of the pandemic.21 These deaths could be caused by changes in health resulting from food insecurity, housing instability, and other stressors and by increases in poisonings, suicide, and accidents.22–26
Identifying the spatial and temporal patterning of excess deaths not assigned to COVID-19 throughout the pandemic has important implications for the death investigation system and for social programs providing pandemic relief.15 Communities with high proportions of these deaths may represent areas where COVID-19 deaths were not accurately recognized because of flawed death investigation practices.16 These communities may be potential targets for additional training on death investigation.27 One important social program that has been established during the pandemic to provide economic relief to families who have lost loved ones to the pandemic is FEMA’s funeral assistance program. This program provides families with a maximum of $9,000 per deceased individual and a maximum of $35,500 per application to cover funeral costs.28 The application, however, requires that families provide a death certificate stating that the death may have been caused by or was likely a result of COVID-19. Deaths that were not assigned to COVID-19 on death certificates are not eligible for this program. As a result, communities with large numbers of these deaths may represent areas where this social program has had less impact. Thus, estimates of excess deaths not assigned to COVID-19 may help inform reforms to FEMA’s program and the development of new relief programs.
In the present study, we compare monthly estimates of excess mortality generated using a Bayesian hierarchical model based on all-cause mortality to county-month data on deaths assigned to COVID-19 for 3,127 counties during the first two years of the pandemic (March 2020 to February 2022). This comparison produces estimates of excess deaths not assigned to COVID-19 for each county-month. We then explore spatial and temporal patterning of these deaths relative to expected all-cause deaths across Census divisions and large metros, medium/small metros, and nonmetro areas throughout the first and second year of the pandemic.
Data and Methods
Experimental Design
This study focuses on the comparison between estimated excess mortality for the period March 2020 - February 2022 and official COVID-19 mortality. We modeled monthly all-cause excess mortality using a Bayesian hierarchical model for 3,127 counties for the period March 2020 to February 2022. We used publicly available data for the period January 2015 - December 2019 to fit the model, and examined a set of metrics to assess the goodness of fit and the model’s sensitivity to different specifications. Starting from the county-month estimates, we built geographically (Census divisions, metropolitan-nonmetropolitan categories) aggregated counts to investigate how excess mortality compared to COVID-19 mortality across the U.S. during the pandemic’s first two years.
Data
We extracted monthly death counts at the county-level from the CDC WONDER online tool. See Supplementary Text for further details about data extraction procedures. We extracted all-cause death counts and COVID-19 death counts from the Multiple Cause of Death database using the provisional counts for 2021 and 2022 and the final counts for 2015–2020. We define COVID-19 deaths as those in which COVID-19 was listed as the underlying cause of death using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) code U07.1. COVID-19 is listed as the underlying cause of death in approximately 92% of cases in which it is mentioned somewhere on the death certificate29. To transform the number of deaths into rates, we used publicly available yearly county-level population estimates from the Census Bureau (2010–202030 and 202131). To obtain monthly population estimates, we assumed the population grew linearly between each two time points. For the August 2021 - February 2022 period, for which no population estimates are available, we projected county-level population by computing county-specific average monthly growth rates for the period January 2018 - July 2021 (the most recent month for which Census Bureau estimates were available) and then applying these rates to the July 2021 population.
In some of the tables and figures, we present aggregate quantities by grouping counties into 3 metropolitan-nonmetropolitan categories (large metro, medium or small metro, and nonmetro) based on the 2013 NCHS Rural-Urban Classification Scheme for Counties.32 We also grouped counties into 9 Census Bureau Divisions (New England, Middle Atlantic, East North Central, West North Central, South Atlantic, East South Central, West South Central, Mountain, and Pacific). Finally, in some analyses, we stratified the Census Divisions by the metropolitan-nonmetropolitan categories. The Supplementary Text provides further details about the geographic classifications used in this study.
Statistical Methods
We used a Bayesian hierarchical model to predict the monthly county-level number of deaths. Our methods are described in more detail elsewhere3, but in summary we started from the framework described in a prior paper33 and made some adaptations to fit our specific application. Let yts be the number of deaths in spatial unit s at time t. Let Pts be the population of spatial unit s at time t. We assume a Poisson distribution for the number of monthly deaths yts and model the risk rts of dying using the following specification:
where β0 is the global intercept. We included dummy variables (fixed effects) for each combination of month and Census division to capture seasonal effects (allowing for division-level heterogeneity). The model incorporates a linear effect (captured by βTime) and non-linear effect f(⋅) of time (in months) since the start of the period (t = 1, 2, … with time 1 corresponding to January 2015). We added a non-linear effect of time, modeled as a first-order autoregressive process (AR1) model:
To capture the spatial structure of the data, we modeled county-level intercepts using the modified Besag, York and Mollie spatial model proposed by Riebler et al. (BYM2 model).34 This model is the sum of two random effects, a spatially unstructured one, and spatially structured one us. The term bs in the model is thus defined as:
where and are standardized versions of us and vs to have variance equal to 1. The term. 0 ≤ ϕ ≤ 1 is a mixing parameter which measures the proportion of the marginal variance explained by the spatially structured effect
We used minimally informative prior distributions for the fixed effects β0, the month-division specific intercepts Monthm · Divisions m = 1, 2, …, 12, the linear time effect βTime, and the ϕ1 parameter for the AR1 process. For the hyperparameters of the BYM2 model, ϕ and τb, we adopted priors that tend to regularize inference while not providing too strong information, the so-called penalized complexity (PC) priors introduced by Simpson et al.35 In particular, for the standard deviation I select a prior so that, Pr(σb > 1) = 0.01, implying that it is unlikely to have a spatial relative risk higher than exp(2) based solely on spatial or temporal variation. For ϕ we set Pr Pr (ϕ < 0. 5) = 0. 5 reflecting our lack of knowledge about which.spatial component, the unstructured or structured one, should dominate the spatial bs.
Finally, we also adopt PC priors for the remaining standard deviation such that Pr(σt > 1) = 0.01.
We fit the models using the Integrated Nested Laplace Approximation (INLA) method, through the R-INLA software package.36
To compare measures of excess mortality and differences between excess mortality and COVID-19 mortality across counties with different populations and numbers of deaths, we used relative measures of excess mortality throughout this study. Relative excess mortality refers to the number of excess deaths divided by the number of expected deaths in an area. Relative excess mortality not assigned to COVID-19 refers to the difference between excess deaths and deaths assigned to COVID-19 divided by the number of expected deaths in an area.
This study used de-identified publicly available data and was exempted from review by the Boston University Medical Center Institutional Review Board. Programming code was developed using R, version 4.1.0 (R Project for Statistical Computing) and Python, version 3.7.13 (Python Software Foundation).
Results
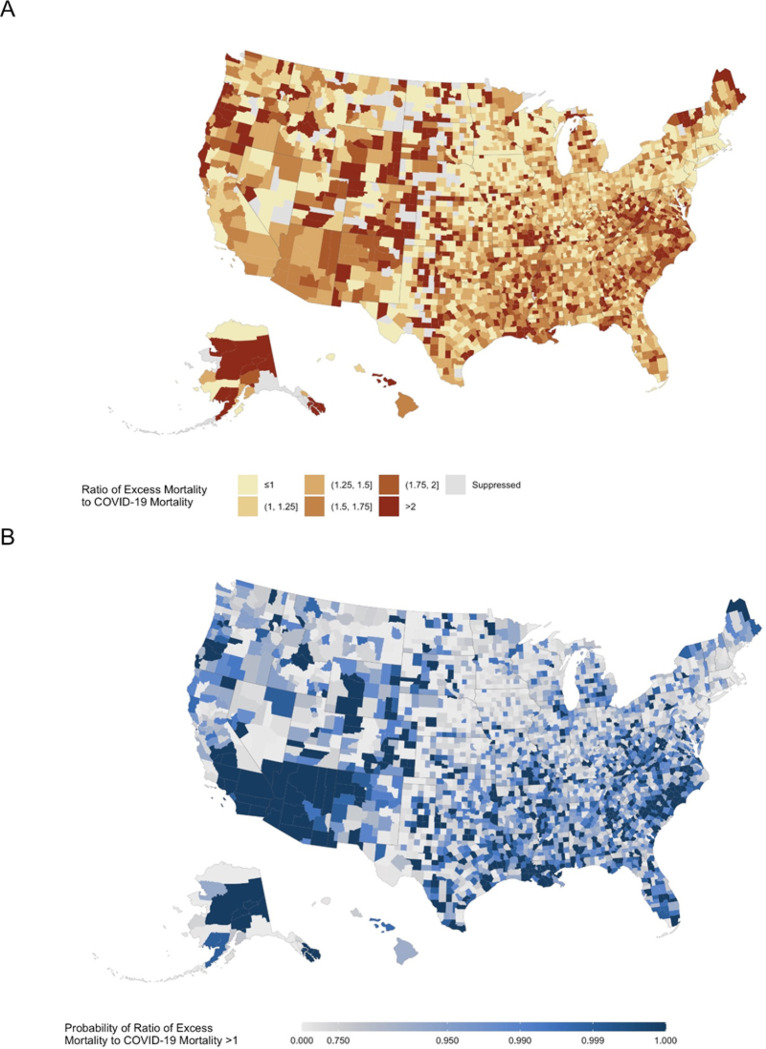
Table 1 presents estimates of excess deaths not assigned to COVID-19 in the U.S. and across Census divisions and metro-nonmetro categories. We estimated that between March 2020 and February 2022 there were 1,134,364 excess deaths (95% prediction interval (PI): 996,869 to 1,278,540) occurred in the U.S., of which 866,187 were assigned to COVID-19 and 268,176 (95% PI: 130,682 to 412,353) were not assigned to COVID-19. Proportionally, this indicates that 23.7% (95% PI: 11.5% to 36.4%) of excess deaths in the U.S. were not assigned to COVID-19. Figure 1 shows the ratio of excess mortality to COVID-19 mortality in counties across the U.S., revealing significant heterogeneity in the proportion of excess deaths not assigned to COVID-19 throughout the country. The Supplemental Table shows this heterogeneity at the state-level.
Table 1.
Excess mortality across U.S. Census Divisions and metro/nonmetro areas over the first two years of the pandemic.
| COVID-19 Deaths | Excess/COVID | Absolute Excess Mortality | Relative Excess Mortality | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Excluding COVID-19 | Total | Excluding COVID-19 | |||||||
| Median | PI (90%) | Median | PI (90%) | Median | PI (90%) | Median | PI (90%) | |||
| East North Central | ||||||||||
| Large Metro | 66,204 | 1.258 | 83,292 | (72,546 – 94,549) | 17,088 | (6,342 – 28,345) | 0.182 | (0.155 – 0.212) | 0.037 | (0.014 – 0.063) |
| Medium or Small Metro | 36,001 | 1.259 | 45,314 | (38,988 – 51,684) | 9,312 | (2,987 – 15,683) | 0.172 | (0.145 – 0.202) | 0.035 | (0.011 – 0.061) |
| Non Metro | 27,136 | 1.323 | 35,910 | (30,925 – 40,844) | 8,774 | (3,789 – 13,708) | 0.178 | (0.149 – 0.207) | 0.043 | (0.018 – 0.070) |
| Total | 129,341 | 1.272 | 164,532 | (143,026 – 187,186) | 35,192 | (13,685 – 57,845) | 0.178 | (0.152 – 0.208) | 0.038 | (0.014 – 0.064) |
| East South Central | ||||||||||
| Large Metro | 16,562 | 1.438 | 23,818 | (21,117 – 26,604) | 7,256 | (4,555 – 10,042) | 0.211 | (0.183 – 0.242) | 0.064 | (0.039 – 0.091) |
| Medium or Small Metro | 23,298 | 1.386 | 32,286 | (28,575 – 36,247) | 8,988 | (5,277 – 12,949) | 0.208 | (0.179 – 0.239) | 0.058 | (0.033 – 0.085) |
| Non Metro | 24,075 | 1.573 | 37,862 | (34,025 – 41,770) | 13,788 | (9,950 – 17,695) | 0.241 | (0.212 – 0.273) | 0.088 | (0.062 – 0.116) |
| Total | 63,935 | 1.471 | 94,031 | (84,142 – 104,474) | 30,096 | (20,207 – 40,539) | 0.221 | (0.193 – 0.252) | 0.071 | (0.046 – 0.098) |
| Middle Atlantic | ||||||||||
| Large Metro | 98,066 | 0.942 | 92,348 | (79,913 – 105,204) | −5,718 | (−18,152 – 7,138) | 0.178 | (0.150 – 0.208) | −0.011 | (−0.034 – 0.014) |
| Medium or Small Metro | 24,780 | 0.990 | 24,529 | (20,217 – 28,920) | −251 | (−4,562 – 4,140) | 0.137 | (0.110 – 0.166) | −0.001 | (−0.025 – 0.024) |
| Non Metro | 9,241 | 1.311 | 12,111 | (10,525 – 13,787) | 2,870 | (1,284 – 4,546) | 0.185 | (0.157 – 0.216) | 0.044 | (0.019 – 0.071) |
| Total | 132,087 | 0.977 | 128,990 | (110,681 – 147,798) | −3,096 | (−21,405 – 15,711) | 0.169 | (0.142 – 0.198) | −0.004 | (−0.027 – 0.021) |
| Mountain | ||||||||||
| Large Metro | 28,921 | 1.502 | 43,428 | (39,326 – 47,604) | 14,507 | (10,405 – 18,683) | 0.255 | (0.225 – 0.286) | 0.085 | (0.060 – 0.112) |
| Medium or Small Metro | 22,921 | 1.429 | 32,762 | (29,217 – 36,458) | 9,842 | (6,296 – 13,537) | 0.218 | (0.190 – 0.249) | 0.066 | (0.041 – 0.092) |
| Non Metro | 12,064 | 1.599 | 19,296 | (17,419 – 21,247) | 7,232 | (5,355 – 9,183) | 0.254 | (0.223 – 0.287) | 0.095 | (0.069 – 0.124) |
| Total | 63,906 | 1.495 | 95,527 | (85,924 – 105,371) | 31,621 | (22,018 – 41,465) | 0.241 | (0.212 – 0.272) | 0.080 | (0.054 – 0.107) |
| New England | ||||||||||
| Large Metro | 18,426 | 0.731 | 13,462 | (10,209 – 16,801) | −4,964 | (−8,216 – −1,624) | 0.100 | (0.074 – 0.128) | −0.037 | (−0.060 – −0.012) |
| Medium or Small Metro | 12,428 | 0.819 | 10,179 | (7,651 – 12,801) | −2,249 | (−4,776 – 373) | 0.098 | (0.072 – 0.126) | −0.022 | (−0.045 – 0.004) |
| Non Metro | 2,493 | 1.340 | 3,340 | (2,367 – 4,393) | 846 | (−125 – 1,900) | 0.084 | (0.058 – 0.114) | 0.021 | (−0.003 – 0.049) |
| Total | 33,347 | 0.808 | 26,948 | (20,345 – 33,857) | −6,398 | (−13,001 – 510) | 0.097 | (0.071 – 0.125) | −0.023 | (−0.046 – 0.002) |
| Pacific | ||||||||||
| Large Metro | 72,630 | 1.373 | 99,741 | (87,978 – 111,925) | 27,111 | (15,348 – 39,295) | 0.202 | (0.174 – 0.233) | 0.055 | (0.030 – 0.082) |
| Medium or Small Metro | 27,031 | 1.372 | 37,080 | (31,712 – 42,661) | 10,049 | (4,681 – 15,630) | 0.164 | (0.137 – 0.194) | 0.044 | (0.020 – 0.071) |
| Non Metro | 4,486 | 1.802 | 8,083 | (6,624 – 9,653) | 3,597 | (2,138 – 5,167) | 0.133 | (0.107 – 0.163) | 0.059 | (0.034 – 0.087) |
| Total | 104,147 | 1.392 | 144,926 | (126,401 – 164,083) | 40,778 | (22,254 – 59,936) | 0.186 | (0.158 – 0.216) | 0.052 | (0.028 – 0.079) |
| South Atlantic | ||||||||||
| Large Metro | 80,005 | 1.357 | 108,528 | (95,111 – 122,942) | 28,524 | (15,106 – 42,937) | 0.188 | (0.161 – 0.218) | 0.049 | (0.026 – 0.076) |
| Medium or Small Metro | 64,118 | 1.444 | 92,561 | (81,342 – 104,260) | 28,443 | (17,224 – 40,142) | 0.197 | (0.169 – 0.227) | 0.061 | (0.036 – 0.088) |
| Non Metro | 25,181 | 1.916 | 48,242 | (43,960 – 52,671) | 23,061 | (18,779 – 27,490) | 0.270 | (0.240 – 0.302) | 0.129 | (0.103 – 0.158) |
| Total | 169,304 | 1.472 | 249,185 | (220,605 – 279,355) | 79,881 | (51,301 – 110,051) | 0.203 | (0.176 – 0.233) | 0.065 | (0.041 – 0.092) |
| West North Central | ||||||||||
| Large Metro | 17,288 | 1.198 | 20,717 | (17,618 – 23,982) | 3,429 | (330 – 6,694) | 0.160 | (0.133 – 0.190) | 0.026 | (0.002 – 0.053) |
| Medium or Small Metro | 17,453 | 1.113 | 19,428 | (16,280 – 22,481) | 1,975 | (−1,172 – 5,028) | 0.155 | (0.127 – 0.184) | 0.016 | (−0.009 – 0.041) |
| Non Metro | 15,915 | 1.434 | 22,828 | (19,227 – 26,715) | 6,913 | (3,312 – 10,800) | 0.153 | (0.126 – 0.184) | 0.046 | (0.022 – 0.074) |
| Total | 50,656 | 1.242 | 62,931 | (53,291 – 72,996) | 12,275 | (2,635 – 22,340) | 0.156 | (0.129 – 0.185) | 0.030 | (0.006 – 0.057) |
| West South Central | ||||||||||
| Large Metro | 52,366 | 1.315 | 68,886 | (61,745 – 76,066) | 16,520 | (9,379 – 23,699) | 0.230 | (0.202 – 0.261) | 0.055 | (0.031 – 0.081) |
| Medium or Small Metro | 42,857 | 1.387 | 59,456 | (54,375 – 64,857) | 16,598 | (11,518 – 22,000) | 0.276 | (0.247 – 0.309) | 0.077 | (0.052 – 0.105) |
| Non Metro | 24,241 | 1.621 | 39,292 | (35,682 – 43,102) | 15,050 | (11,441 – 18,861) | 0.266 | (0.236 – 0.300) | 0.102 | (0.076 – 0.131) |
| Total | 119,464 | 1.403 | 167,616 | (151,975 – 184,103) | 48,152 | (32,511 – 64,639) | 0.253 | (0.224 – 0.285) | 0.073 | (0.048 – 0.100) |
| United States | ||||||||||
| Large Metro | 450,468 | 1.230 | 554,169 | (487,560 – 625,373) | 103,701 | (37,092 – 174,905) | 0.191 | (0.165 – 0.222) | 0.036 | (0.013 – 0.062) |
| Medium or Small Metro | 270,887 | 1.305 | 353,540 | (309,493 – 400,051) | 82,653 | (38,606 – 129,164) | 0.187 | (0.160 – 0.217) | 0.044 | (0.020 – 0.070) |
| Non Metro | 144,832 | 1.567 | 226,902 | (201,393 – 253,792) | 82,070 | (56,561 – 108,960) | 0.211 | (0.183 – 0.242) | 0.076 | (0.051 – 0.104) |
| Total | 866,187 | 1.310 | 1,134,364 | (996,869 – 1,278,540) | 268,176 | (130,682 – 412,353) | 0.194 | (0.166 – 0.224) | 0.046 | (0.022 – 0.072) |
Figure 1.
Ratio of excess mortality to COVID-19 mortality across U.S. counties, March 2020 - February 2022
Notes: Each county in the map is colored according to its ratio of excess mortality to COVID-19 mortality. Suppressed values reflect counties in which the cumulative number of COVID-19 deaths from March 2020 through February 2022 was less than 10 deaths.
Estimates Across Metro-Nonmetro Categories
After subtracting deaths assigned to COVID-19, the total of deaths observed from March 2020 to February 2022 was 4.6% (95% PI: 2.2% to 7.2%) higher than expected based on pre-pandemic trends. This estimate also known as relative excess mortality for deaths not assigned to COVID-19 was higher in non-metro counties (7.6% [95% PI: 5.1% to 10.4%]) compared to medium or small metro counties (4.4% [95% PI: 2.0% to 7.0%]) and large metro counties (3.6% [95% PI: 1.3% to 6.2%]).
Estimates Across Census Divisions
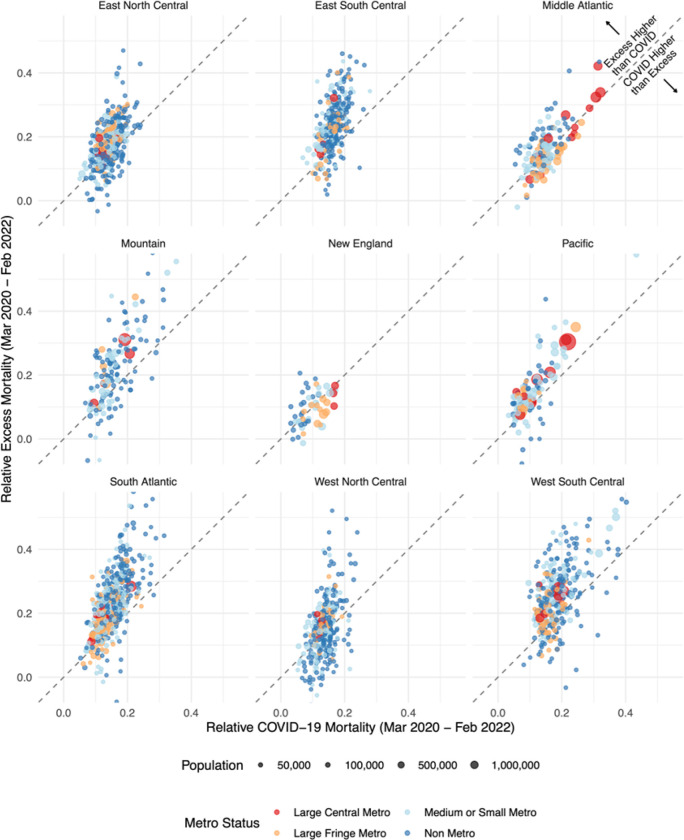
Figure 2 compares excess deaths to COVID-19 deaths in counties across Census divisions, revealing that all divisions except the New England and Middle Atlantic divisions appeared to have more excess deaths than COVID-19 deaths. Relative excess mortality for deaths not assigned to COVID-19 was highest in the Mountain division and in the South. It was 8.0% (95% PI: 5.4% to 10.7) in the Mountain division, 7.3% (95% PI: 4.8% to 10.0%) in the West South Central division, 7.1% (95% PI: 4.6% to 9.8%) in the East South Central division, and 6.5% (95% PI: 4.1% to 9.2%) in the South Atlantic division. In contrast, relative excess mortality for deaths not assigned to COVID-19 was negative in the New England division (−2.3% [95% PI: −4.6% to 0.2%]) and in the Middle Atlantic division (−0.4% [95% PI: −2.7% to 2.1%]).
Figure 2.
Comparison of excess deaths to COVID-19 deaths across U.S. counties by Census Division, March 2020 - February 2022
Notes: Each point in the graph represents a county and reflects its relative COVID-19 mortality from March 2020 to February 2022 (horizontal axis) and its relative excess mortality from March 2020 to February 2022 (vertical axis). Relative COVID-19 mortality is the ratio of COVID-19 deaths to expected deaths. We excluded counties with less than 10,000 residents to make the relationship between the two variables clearer. The 45 degrees line separates the plot into two parts. Points above the line saw more excess than COVID-19 mortality. Points falling below the line saw instead more COVID-19 mortality than excess mortality.
Estimates Across Combinations of Metro-Nonmetro Categories and Census Divisions
In all 9 divisions, relative excess mortality for deaths not assigned to COVID-19 was higher in nonmetro counties than metro counties. The areas that had the highest relative excess mortality for deaths not assigned to COVID-19 were nonmetro counties in the South Atlantic division (12.9% [10.3% to 15.8%]), West South Central division (10.2% [95% PI: 7.6% to 13.1%]), Mountain division (9.5% [95% PI: 6.9% to 12.4%]), and East South Central division (8.8% [95% PI: 6.2% to 11.6%]). The areas that had negative relative excess mortality for deaths not assigned to COVID-19 were large metro counties in the New England division (−3.7% [95% PI: −6.0% to −1.2%]) and the Middle Atlantic division (−1.1% [95% PI: −3.4% to 1.4%]) and medium or small metro counties in the New England division (−2.2% [95% PI: −4.5% to 0.4%]) and the Middle Atlantic division (−0.1% [95% PI: −2.5% to 2.4%]). Nonmetro counties in these divisions had positive relative excess mortality for deaths not assigned to COVID-19.
Temporal Patterns
Figure 3 shows temporal variations in excess deaths, reported COVID-19 deaths, and excess deaths not assigned to COVID-19 by month across combinations of metro-nonmetro categories and Census divisions. Pronounced differences between excess deaths and reported COVID-19 deaths emerged early in the pandemic and persisted into the pandemic’s second year. Between March 2020 and February 2022, reported COVID-19 deaths tracked closely with monthly excess mortality estimates across all areas. Excess deaths not assigned to COVID-19 were typically more frequent during reported COVID-19 peaks than during the troughs between peaks. This is most apparent in areas that had the largest relative amounts of excess deaths not assigned to COVID-19 such as in the East South Central and South Atlantic divisions. In contrast, in the New England and Middle Atlantic divisions where COVID-19 deaths exceeded excess deaths in many areas, excess deaths not assigned to COVID-19 remained relatively stable over time, not changing during reported COVID-19 peaks. Finally, in areas where excess deaths not assigned to COVID-19 did rise with reported COVID-19 peaks, it appeared that the rise in excess deaths not assigned to COVID-19 often preceded or occurred concurrently with the rise in COVID-19 deaths.
Figure 3.
Monthly variation in COVID-19 and excess mortality across Census Divisions and metro/nonmetro categories
Counties with the Largest Gaps Between Excess and COVID-19 Deaths
Table 2 presents estimates of excess deaths not assigned to COVID-19 for the counties with the highest ratios of excess to COVID-19 deaths in each Census Division over the first two years of the pandemic. For example, Shelby, Tennessee had 2.4 times more excess deaths than COVID-19 deaths during the first two years of the pandemic. In absolute terms, this equaled 4,014 (95% PI: 3,562 to 4,517) excess deaths that were not assigned to COVID-19 during this period. Lafeyette, Louisiana had 2.5 times more excess deaths than COVID-19 deaths during the first two years of the pandemic. This equaled 654 (95% PI: 504 to 805) excess deaths not assigned to COVID-19 during this period. Estimates of the ratio and difference between excess and COVID-19 deaths for all 3,127 counties in the study are available in the Supplementary Materials.
Table 2.
Excess mortality among U.S. counties with the highest excess to COVID-19 death ratios in each Census Division over the first two years of the pandemic.
| County | State | Excess/COVID | COVID-19 Deaths | Absolute Excess Mortality | Relative Excess Mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Excluding COVID-19 | Total | Excluding COVID-19 | ||||||||
| Median | PI (90%) | Median | PI (90%) | Median | PI (90%) | Median | PI (90%) | ||||
| East North Central | |||||||||||
| Jackson | Illinois | 2.580 | 138 | 356 | (293 – 415) | 218 | (155 – 277) | 0.392 | (0.303 – 0.488) | 0.240 | (0.161 – 0.326) |
| Isabella | Michigan | 2.257 | 167 | 377 | (313 – 439) | 210 | (146 – 272) | 0.399 | (0.310 – 0.497) | 0.222 | (0.145 – 0.308) |
| Monroe | Wisconsin | 2.250 | 80 | 180 | (122 – 244) | 100 | (42 – 164) | 0.201 | (0.128 – 0.294) | 0.112 | (0.044 – 0.198) |
| Coles | Illinois | 2.165 | 124 | 268 | (203 – 333) | 144 | (79 – 209) | 0.276 | (0.197 – 0.367) | 0.149 | (0.077 – 0.230) |
| Scioto | Ohio | 2.062 | 257 | 530 | (425 – 636) | 273 | (168 – 379) | 0.252 | (0.193 – 0.319) | 0.130 | (0.076 – 0.190) |
| East South Central | |||||||||||
| Pontotoc | Mississippi | 2.618 | 110 | 288 | (237 – 341) | 178 | (127 – 231) | 0.458 | (0.350 – 0.592) | 0.283 | (0.188 – 0.401) |
| Shelby | Tennessee | 2.419 | 2,830 | 6,844 | (6,392 – 7,347) | 4,014 | (3,562 – 4,517) | 0.401 | (0.365 – 0.444) | 0.235 | (0.204 – 0.273) |
| Marshall | Mississippi | 2.372 | 137 | 325 | (264 – 381) | 188 | (127 – 244) | 0.399 | (0.301 – 0.502) | 0.231 | (0.145 – 0.321) |
| Hinds | Mississippi | 2.183 | 706 | 1,542 | (1,383 – 1,701) | 836 | (677 – 995) | 0.357 | (0.309 – 0.409) | 0.193 | (0.151 – 0.239) |
| Robertson | Tennessee | 2.153 | 209 | 450 | (365 – 529) | 241 | (156 – 320) | 0.302 | (0.231 – 0.374) | 0.162 | (0.099 – 0.226) |
| Middle Atlantic | |||||||||||
| Clinton | New York | 2.198 | 106 | 233 | (144 – 315) | 127 | (38 – 209) | 0.157 | (0.092 – 0.225) | 0.086 | (0.025 – 0.149) |
| Delaware | New York | 2.091 | 88 | 184 | (109 – 249) | 96 | (21 – 161) | 0.170 | (0.094 – 0.245) | 0.089 | (0.018 – 0.158) |
| Wayne | Pennsylvania | 1.947 | 150 | 292 | (213 – 369) | 142 | (63 – 219) | 0.231 | (0.159 – 0.311) | 0.112 | (0.048 – 0.184) |
| Tioga | New York | 1.916 | 107 | 205 | (138 – 268) | 98 | (31 – 161) | 0.211 | (0.134 – 0.295) | 0.101 | (0.031 – 0.177) |
| Franklin | New York | 1.903 | 72 | 137 | (75 – 201) | 65 | (3 – 129) | 0.149 | (0.077 – 0.236) | 0.071 | (0.003 – 0.151) |
| Mountain | |||||||||||
| Uintah | Utah | 2.717 | 53 | 144 | (93 – 190) | 91 | (40 – 137) | 0.279 | (0.164 – 0.403) | 0.176 | (0.070 – 0.291) |
| Douglas | Colorado | 2.111 | 416 | 878 | (729 – 999) | 462 | (313 – 583) | 0.280 | (0.222 – 0.332) | 0.148 | (0.095 – 0.194) |
| Douglas | Nevada | 2.084 | 107 | 223 | (150 – 288) | 116 | (43 – 181) | 0.202 | (0.128 – 0.277) | 0.105 | (0.037 – 0.174) |
| La Plata | Colorado | 2.069 | 87 | 180 | (127 – 240) | 93 | (40 – 153) | 0.252 | (0.165 – 0.367) | 0.130 | (0.052 – 0.234) |
| Sweetwater | Wyoming | 2.035 | 115 | 234 | (186 – 284) | 119 | (71 – 169) | 0.388 | (0.286 – 0.514) | 0.197 | (0.109 – 0.306) |
| New England | |||||||||||
| Washington | Maine | 4.198 | 43 | 180 | (116 – 241) | 138 | (73 – 198) | 0.204 | (0.122 – 0.292) | 0.155 | (0.077 – 0.240) |
| Washington | Vermont | 3.470 | 33 | 114 | (46 – 189) | 82 | (13 – 156) | 0.100 | (0.038 – 0.176) | 0.071 | (0.011 – 0.145) |
| Addison | Vermont | 3.095 | 21 | 65 | (15 – 112) | 44 | (−6 – 91) | 0.098 | (0.021 – 0.182) | 0.066 | (−0.008 – 0.147) |
| Bennington | Vermont | 2.714 | 21 | 57 | (−9 – 126) | 36 | (−30 – 105) | 0.057 | (−0.009 – 0.136) | 0.036 | (−0.028 – 0.113) |
| Rutland | Vermont | 2.550 | 40 | 102 | (17 – 183) | 62 | (−22 – 143) | 0.069 | (0.011 – 0.130) | 0.042 | (−0.014 – 0.102) |
| Pacific | |||||||||||
| Maui | Hawaii | 3.455 | 88 | 304 | (187 – 413) | 216 | (99 – 325) | 0.128 | (0.075 – 0.182) | 0.091 | (0.040 – 0.143) |
| Mendocino | California | 2.538 | 104 | 264 | (174 – 360) | 160 | (70 – 256) | 0.143 | (0.091 – 0.206) | 0.087 | (0.037 – 0.147) |
| Amador | California | 2.478 | 46 | 114 | (47 – 181) | 68 | (1 – 135) | 0.118 | (0.045 – 0.201) | 0.070 | (0.001 – 0.150) |
| Lane | Oregon | 2.401 | 421 | 1,011 | (756 – 1,261) | 590 | (335 – 840) | 0.131 | (0.095 – 0.169) | 0.076 | (0.042 – 0.112) |
| San Francisco | California | 2.392 | 704 | 1,684 | (1,341 – 2,055) | 980 | (637 – 1,351) | 0.147 | (0.114 – 0.185) | 0.085 | (0.054 – 0.122) |
| South Atlantic | |||||||||||
| Amherst | Virginia | 2.983 | 59 | 176 | (120 – 233) | 117 | (61 – 174) | 0.248 | (0.157 – 0.357) | 0.165 | (0.080 – 0.267) |
| Duplin | North Carolina | 2.903 | 185 | 537 | (471 – 597) | 352 | (286 – 412) | 0.573 | (0.470 – 0.681) | 0.376 | (0.285 – 0.470) |
| Clarendon | South Carolina | 2.658 | 152 | 404 | (347 – 459) | 252 | (195 – 307) | 0.529 | (0.424 – 0.648) | 0.330 | (0.239 – 0.433) |
| Halifax | North Carolina | 2.628 | 156 | 410 | (336 – 485) | 254 | (180 – 329) | 0.315 | (0.244 – 0.395) | 0.195 | (0.131 – 0.268) |
| Louisa | Virginia | 2.486 | 69 | 172 | (109 – 225) | 102 | (40 – 156) | 0.224 | (0.133 – 0.316) | 0.134 | (0.050 – 0.219) |
| West North Central | |||||||||||
| Beltrami | Minnesota | 2.625 | 88 | 231 | (170 – 289) | 143 | (82 – 201) | 0.275 | (0.188 – 0.369) | 0.170 | (0.091 – 0.257) |
| Warren | Missouri | 2.612 | 80 | 209 | (153 – 261) | 129 | (73 – 181) | 0.315 | (0.213 – 0.427) | 0.195 | (0.102 – 0.296) |
| Camden | Missouri | 2.336 | 149 | 348 | (283 – 412) | 199 | (134 – 263) | 0.353 | (0.269 – 0.447) | 0.202 | (0.127 – 0.285) |
| Cass | Minnesota | 2.220 | 50 | 111 | (59 – 160) | 61 | (9 – 110) | 0.171 | (0.084 – 0.266) | 0.094 | (0.013 – 0.183) |
| Itasca | Minnesota | 2.000 | 94 | 188 | (120 – 253) | 94 | (26 – 159) | 0.174 | (0.106 – 0.250) | 0.087 | (0.024 – 0.157) |
| West South Central | |||||||||||
| Iberville | Louisiana | 3.469 | 32 | 111 | (83 – 138) | 79 | (51 – 106) | 0.474 | (0.317 – 0.667) | 0.338 | (0.195 – 0.512) |
| Lafayette | Louisiana | 2.481 | 442 | 1,096 | (946 – 1,247) | 654 | (504 – 805) | 0.294 | (0.244 – 0.349) | 0.176 | (0.130 – 0.225) |
| Acadia | Louisiana | 2.241 | 245 | 549 | (470 – 626) | 304 | (225 – 381) | 0.439 | (0.354 – 0.533) | 0.243 | (0.170 – 0.325) |
| Webster | Louisiana | 2.213 | 167 | 370 | (304 – 437) | 202 | (137 – 270) | 0.366 | (0.283 – 0.464) | 0.201 | (0.127 – 0.287) |
| Vermilion | Louisiana | 2.193 | 181 | 397 | (330 – 467) | 216 | (149 – 286) | 0.345 | (0.271 – 0.432) | 0.188 | (0.122 – 0.265) |
Notes: Limited to counties with more than 30,000 residents and at least 20 COVID-19 deaths cumulatively over the period from March 2020 through February 2022.
Discussion
In the present study, we generated estimates of excess mortality for counties across the U.S. and identified 268,176 excess deaths that were not assigned to COVID-19 during the first two years of the COVID-19 pandemic, which represented 23.7% of all excess deaths that occurred. Excess deaths were less likely to be assigned to COVID-19 in the Mountain division, in the South, and in nonmetro counties. The number of excess deaths exceeded COVID-19 deaths in all Census divisions except for the New England and Middle Atlantic divisions where there were more COVID-19 deaths than excess deaths in large metro areas and medium or small metro areas. In areas where substantial numbers of excess deaths were not assigned to COVID-19, rises in excess deaths not assigned to COVID-19 generally tracked temporally with rises in reported COVID-19 deaths. Contrary to prior literature which suggested that the majority of excess deaths not assigned to COVID-19 occurred early in the pandemic,37 differences between excess deaths and reported COVID-19 deaths were substantial in both the first and second year of the pandemic.
Although our study does not distinguish between unrecognized COVID-19 deaths and deaths indirectly related to the pandemic, emerging literature suggests that a large share of the excess deaths not assigned to COVID-19 represent unrecognized COVID-19 deaths.12,13,38 One study found that approximately 90% of excess mortality between March 2020 and April 2021 could be attributed to the direct effects of SARS-CoV-2 infection.38 Another study found significant temporal concordance between peaks in out-of-hospital COVID-19 deaths and excess deaths not assigned to COVID-19, with the latter preceding the former by 2 to 3 weeks.14 This suggests that many COVID-19 deaths go unrecognized during the beginning of COVID-19 surges when testing may be less frequent and medical providers are not expecting cases. Our study may provide further evidence to support this observation, as rises in excess deaths not assigned to COVID-19 typically preceded or occurred concurrently with rises in reported COVID-19 deaths in most Census divisions throughout the first two years of the pandemic. This possibility is also supported by investigative reporting during the pandemic which has documented widespread irregularities in cause-of-death assignment resulting from over-burdened and under-resourced death investigation systems.16 The individual county-level estimates generated in this study may be useful to reporters and public health officials interested in investigating possible irregularities in cause-of-death assignment within the death investigation system during the pandemic.
Discrepancies between COVID-19 and excess deaths are problematic because they have the potential to mislead scientists and policymakers about which areas were most heavily affected by the pandemic. Failure to accurately capture COVID-19 deaths also points to an urgent need to modernize the death investigation system in the United States, including expanding budgets for medical examiner officers and eliminating the coroner system.15 It can also affect individuals and families, as unrecognized COVID-19 deaths are not eligible for economic relief programs such as FEMA’s funeral assistance program.
Our study identified especially large discrepancies between COVID-19 and excess mortality rates in the Mountain division, in the South, and in nonmetro counties. More unrecognized COVID-19 deaths may have occurred in these areas as a result of limited COVID-19 testing and a greater share of deaths occuring outside of hospital settings, both of which complicate valid cause-of-death assignment.8,14,39 Another potential contributing factor is the greater reliance on coroners in these regions, who are typically elected and often hold other positions within the county such as sheriff-coroners.40 Medical training required for coroners is limited and highly variable across states,41 whereas medical examiners are physicians with extensive training in forensic pathology and death investigation.42 Coroners may also have more limited budgets for death investigation, affecting the likelihood they might pursue post-mortem COVID-19 testing.15 In fact, preliminary reporting has identified specific coroners across the United States who frequently defer to the decedent’s family regarding what they list as the underlying cause of death on the death certificate.43 Outside of COVID-19 mortality reporting, coroner systems have been shown to under-report opioid-related overdoses, and serious issues have been raised about the failures of medicolegal death investigation systems to monitor deaths in police custody.44,45
In the New England and Middle Atlantic divisions, we observed a different pattern around assignment of COVID-19 deaths than in other areas. In these divisions, a large share of counties had higher COVID-19 than excess death rates. Several explanations may exist for this pattern including that other causes of death (i.e. influenza) declined in these areas or that the economically privileged status of some of these counties shielded their residents from the negative indirect effect of the pandemic by allowing them to work-from-home and avoid household crowding. Finally, it is possible that deaths were over-assigned to COVID-19 in these areas due to different cause-of-death assignment protocols for COVID-19. For example, until March 2022, COVID-19 deaths in the state of Massachusetts included any death that occurred within 60 days of a COVID-19 diagnosis, which differed from other states and guidelines from the Council of State and Territorial Epidemiologists that recommended states use a 30 day window.46
Our study had several limitations. First, we were unable to distinguish between excess deaths that represented unrecognized COVID-19 deaths and excess deaths indirectly related to the pandemic. Future research should examine this distinction to clarify the extent to which the excess deaths not assigned to COVID-19 reported in this study represent under-reporting of COVID-19 deaths. Second, we used underlying cause of death data to identify deaths assigned to COVID-19 and thus did not identify deaths where COVID-19 was listed as a contributing cause or appeared elsewhere on the death certificate. Third, some counties and states have experienced prolonged reporting delays of COVID-19 deaths, which could affect our estimates of the proportion of excess deaths assigned to COVID-19, particularly in more recent months.
Conclusion
In this study, we used death certificate data to compare excess deaths during the COVID-19 pandemic to reported COVID-19 deaths in counties across the U.S.. We found that many excess deaths were not assigned to COVID-19, and that contrary to prior reports, the number of excess deaths not assigned to COVID-19 was substantial in year two of the pandemic along with year one. Specific regions – the Mountain division, the South, and nonmetro areas – were identified as being less likely to report excess deaths as COVID-19 deaths, suggesting there may be a greater proportion of unrecognized COVID-19 deaths in communities in these areas. In contrast, many counties in the New England and Middle Atlantic Divisions reported more COVID-19 deaths than excess deaths. Overall, the extent to which reported COVID-19 deaths reflected the true mortality impact of the pandemic varied by time and place throughout the U.S. during the first two years of the pandemic. Moving forward, efforts to target resources to the communities most impacted by the pandemic should consider this variation.
Supplementary Material
ACKNOWLEDGMENTS
Funding: The content is solely the responsibility of the authors and does not necessarily represent the official views of the study sponsors. The authors gratefully acknowledge financial support from the Robert Wood Johnson Foundation (77521), the National Institute on Aging (R01-AG060115-04 and R01-AG060115-04S1), the W.K. Kellogg Foundation, the Boston University Center for Emerging Infectious Diseases Policy and Research, and the Agency for Healthcare Research and Quality (T32HS013853).
Footnotes
Competing Interests: The authors report that they have no conflicts of interests to disclose.
Data and Materials Availability:
Data used in the study are publicly available from the US Centers for Disease Control and Prevention and US Census Bureau. Additional details about the data and programming code for replication can be accessed at the linked GitHub repository: https://github.com/eugeniopaglino/county-month-excess.
References
- 1.Wang H, Paulson KR, Pease SA, et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022;399(10334):1513–1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beaney T, Clarke JM, Jain V, et al. Excess mortality: the gold standard in measuring the impact of COVID-19 worldwide? J R Soc Med. 2020;113(9):329–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paglino E, Lundberg DJ, Cho A, et al. Excess all-cause mortality across counties in the United States, March 2020 to December 2021. medRxiv. Published online May 4, 2022. doi: 10.1101/2022.04.23.22274192 [DOI] [Google Scholar]
- 4.Woolf SH, Chapman DA, Sabo RT, Zimmerman EB. Excess Deaths From COVID-19 and Other Causes in the US, March 1, 2020, to January 2, 2021. JAMA. Published online April 2, 2021. doi: 10.1001/jama.2021.5199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinberger DM, Chen J, Cohen T, et al. Estimation of Excess Deaths Associated With the COVID-19 Pandemic in the United States, March to May 2020. JAMA Intern Med. 2020;180(10):1336–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ackley CA, Lundberg DJ, Ma L, Elo IT, Preston SH, Stokes AC. County-level estimates of excess mortality associated with COVID-19 in the United States. SSM Popul Health. 2022;17:101021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stokes AC, Lundberg DJ, Elo IT, Hempstead K, Bor J, Preston SH. COVID-19 and excess mortality in the United States: A county-level analysis. PLoS Med. 2021;18(5):e1003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stokes AC, Lundberg DJ, Bor J, Elo IT, Hempstead K, Preston SH. Association of Health Care Factors With Excess Deaths Not Assigned to COVID-19 in the US. JAMA Network Open. 2021;4(9):e2125287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen JT, Krieger N. Revealing the Unequal Burden of COVID-19 by Income, Race/Ethnicity, and Household Crowding: US County Versus Zip Code Analyses. J Public Health Manag Pract. 2021;27 Suppl 1, COVID-19 and Public Health: Looking Back, Moing Forward:S43–S56. [DOI] [PubMed] [Google Scholar]
- 10.Wrigley-Field E, Garcia S, Leider JP, Van Riper D. COVID-19 Mortality At The Neighborhood Level: Racial And Ethnic Inequalities Deepened In Minnesota In 2020. Health Aff. 2021;40(10):1644–1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lundberg DJ, Cho A, Raquib R, Nsoesie EO, Wrigley-Field E, Stokes AC. Geographic and Temporal Patterns in Covid-19 Mortality by Race and Ethnicity in the United States from March 2020 to February 2022. medRxiv. Published online July 21, 2022.doi: 10.1101/2022.07.20.22277872 [DOI] [Google Scholar]
- 12.Zhang Y, Chang HH, Iuliano AD, Reed C. Application of Bayesian spatial-temporal models for estimating unrecognized COVID-19 deaths in the United States. Spat Stat. Published online January 4, 2022:100584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iuliano AD, Chang HH, Patel NN, et al. Estimating under-recognized COVID-19 deaths, United States, march 2020-may 2021 using an excess mortality modelling approach. Lancet Reg Health Am. 2021;1:100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen YH, Stokes AC, Aschmann HE, et al. Excess natural-cause deaths in California by cause and setting: March 2020 through February 2021. PNAS Nexus. Published online June 8, 2022:gac079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stokes AC, Lundberg DJ, Bor J, Bibbins-Domingo K. Excess Deaths During the COVID-19 Pandemic: Implications for US Death Investigation Systems. Am J Public Health. 2021;111(S2):S53–S54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Documenting COVID-19 project and USA TODAY Network. Uncounted: Inaccurate death certificates across the country hide the true toll of COVID-19. USA Today. https://www.usatoday.com/in-depth/news/nation/2021/12/22/covid-deaths-obscured-inaccurate-death-certificates/8899157002/. Published December 26, 2021. Accessed April 19, 2022. [Google Scholar]
- 17.Bhaskaran K, Bacon S, Evans SJ, et al. Factors associated with deaths due to COVID-19 versus other causes: population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg Health Eur. 2021;6:100109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abobaker A, Raba AA, Alzwi A. Extrapulmonary and atypical clinical presentations of COVID-19. J Med Virol. 2020;92(11):2458–2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedman AB, Barfield D, David G, et al. Delayed emergencies: The composition and magnitude of non-respiratory emergency department visits during the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2021;2(1):e12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kiang MV, Irizarry RA, Buckee CO, Balsari S. Every Body Counts: Measuring Mortality From the COVID-19 Pandemic. Ann Intern Med. 2020;173(12):1004–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glei DA, Stokes A, Weinstein M. Changes in mental health, pain, and drug misuse since the mid-1990s: Is there a link? Soc Sci Med. 2020;246:112789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faust JS, Du C, Mayes KD, et al. Mortality From Drug Overdoses, Homicides, Unintentional Injuries, Motor Vehicle Crashes, and Suicides During the Pandemic, March-August 2020. JAMA. 2021;326(1):84–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Egede LE, Walker RJ. Structural Racism, Social Risk Factors, and Covid-19 - A Dangerous Convergence for Black Americans. N Engl J Med. 2020;383(12):e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matthay EC, Duchowny KA, Riley AR, Galea S. Projected All-Cause Deaths Attributable to COVID-19-Related Unemployment in the United States. Am J Public Health. 2021;111(4):696–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen R, Aschmann HE, Chen YH, et al. Racial and Ethnic Disparities in Estimated Excess Mortality From External Causes in the US, March to December 2020. JAMA Intern Med. 2022;182(7):776–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jentzen JM, Ernst MF. Developing medicolegal death investigator systems in forensic pathology. Clin Lab Med. 1998;18(2):279–322. [PubMed] [Google Scholar]
- 28.FEMA Tops $2 Billion of COVID-19 Funeral Assistance, Announces New Campaign to Increase Program Awareness. FEMA. Published March 15, 2022. Accessed May 20, 2022. https://www.fema.gov/press-release/20220315/fema-tops-2-billion-covid-19-funeral-assistance-announces-new-campaign [Google Scholar]
- 29.Excess Deaths Associated with COVID-19: Provisional Death Counts for Coronavirus Disease (COVID-19). Center for Disease Control and Prevention. Published April 13, 2022. Accessed April 18, 2022. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm [Google Scholar]
- 30.Datasets: 2010–2020: Counties: Totals. U.S. Census Bureau. Accessed October 28, 2022. https://www2.census.gov/programs-surveys/popest/datasets/2010-2020/counties/totals/ [Google Scholar]
- 31.Datasets: 2020–2021: Counties: Totals. U.S. Census Bureau. Accessed October 28, 2022. https://www2.census.gov/programs-surveys/popest/datasets/2020-2021/counties/totals/ [Google Scholar]
- 32.U.S. Department of Agriculture, Economic Research Service. 2013. Rural-Urban Continuum Codes. Accessed May 3, 2022. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx
- 33.Konstantinoudis G, Cameletti M, Gómez-Rubio V, et al. Regional excess mortality during the 2020 COVID-19 pandemic in five European countries. Nat Commun. 2022;13(1):482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Riebler A, Sørbye SH, Simpson D, Rue H. An intuitive Bayesian spatial model for disease mapping that accounts for scaling. Stat Methods Med Res. 2016;25(4):1145–1165. [DOI] [PubMed] [Google Scholar]
- 35.Simpson D, Rue H, Riebler A, Martins TG, Sørbye SH. Penalising Model Component Complexity: A Principled, Practical Approach to Constructing Priors. Statistical Science. 2017;32(1):1–28. [Google Scholar]
- 36.Rue H, Martino S, Chopin N. Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. J R Stat Soc Series B Stat Methodol. 2009;71(2):319–392. [Google Scholar]
- 37.Moghadas SM, Galvani AP. The Unrecognized Death Toll of COVID-19 in the United States. Lancet Reg Health Am. 2021;1:100033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee WE, Park SW, Weinberger DM, et al. Direct and indirect mortality impacts of the COVID-19 pandemic in the US, March 2020-April 2021. medRxiv. Published online February 15, 2022. doi: 10.1101/2022.02.10.22270721 [DOI] [Google Scholar]
- 39.Antonio-Villa NE, Bello-Chavolla OY, Fermín-Martínez CA, et al. Socio-demographic inequalities and excess non-COVID-19 mortality during the COVID-19 pandemic: a data-driven analysis of 1 069 174 death certificates in Mexico. Int J Epidemiol. Published online September 29, 2022. doi: 10.1093/ije/dyac184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Research Council. Strengthening Forensic Science in the United States: A Path Forward. The National Academies Press; 2009. [Google Scholar]
- 41.Hanzlick R. Coroner training needs. A numeric and geographic analysis. JAMA. 1996;276(21):1775–1778. [PubMed] [Google Scholar]
- 42.Hanzlick R, Combs D. Medical examiner and coroner systems: history and trends. JAMA. 1998;279(11):870–874. [DOI] [PubMed] [Google Scholar]
- 43.Kincaid J, Kravitz D, Barnard C. In one Missouri county, coroner excludes COVID from death certificates if family asks. The Kansas City Star. Published August 3, 2021. Accessed August 3, 2021. https://www.kansascity.com/news/coronavirus/article253147128.html [Google Scholar]
- 44.Feldman JM, Gruskin S, Coull BA, Krieger N. Quantifying underreporting of law-enforcement-related deaths in United States vital statistics and news-media-based data sources: A capture-recapture analysis. PLoS Med. 2017;14(10):e1002399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feldman JM, Bassett MT. Monitoring Deaths in Police Custody: Public Health Can and Must Do Better. Am J Public Health. 2021;111(S2):S69–S72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Massachusetts Department of Public Health. Department of Public Health updates COVID-19 death definition. Massachusetts: Department of Public Health. Accessed May 3, 2022. https://www.mass.gov/news/department-of-public-health-updates-covid-19-death-definition [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in the study are publicly available from the US Centers for Disease Control and Prevention and US Census Bureau. Additional details about the data and programming code for replication can be accessed at the linked GitHub repository: https://github.com/eugeniopaglino/county-month-excess.