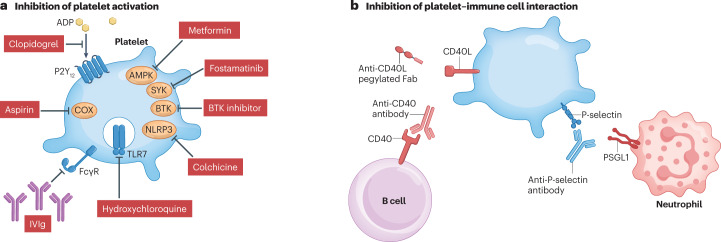
Fig. 4. Potential therapeutic strategies to target platelets in immune-mediated inflammatory disease.
Two strategies may be used to target platelets in immune-mediated inflammatory disease: inhibiting platelet activation or inhibiting the interaction between platelets and immune cells. a, Platelet activation can be inhibited by blocking agonist engagement (for example, blocking adenosine diphosphate (ADP) binding to its receptor P2Y12 with clopidogrel), inhibiting platelet cyclooxygenase (COX) activity using aspirin, inhibiting Toll-like receptor 7 (TLR7) activation using hydroxychloroquine, inhibiting Fcγ receptor (FcγR) engagement or activation using high-dose intravenous immunoglobulin (IVIg), inhibiting the NOD-, LRR- and pyrin domain-containing protein 3 (NLRP3) inflammasome with colchicine and inhibiting intracellular signalling (for example, targeting AMP-activated protein kinase (AMPK) with metformin, spleen tyrosine kinase (SYK) with fostamatinib or Bruton’s tyrosine kinase (BTK) with a specific inhibitor). b, Platelet–immune cell interactions can be inhibited by targeting ligand–receptor pairs that mediate these interactions. For example, antibody to P-selectin prevents P-selectin binding to P-selectin glycoprotein ligand 1 (PSGL1) on neutrophils and other immune cells, and antibodies targeting CD40 or CD40 ligand (CD40L) prevent interaction with B cells. Fab, antigen-binding fragment.