Abstract
The COVID-19 pandemic has led to a worsening of mental health among U.S. adults. However, no review to date has synthesized the overall prevalence of population depressive symptoms in the U.S. over the COVID-19 pandemic. We aimed to document the population prevalence of depressive symptoms and psychological distress across time since the start of the COVID-19 pandemic, both to identify patterns that emerged in the literature and to assess the data sources, methods, sampling, and measurement used to examine population mental health during the pandemic. In a systematic review of the peer review literature, we identified 49 articles reporting 88 prevalence points of depressive symptoms and related constructs in nationally representative samples of U.S. adults from March 2020 to June 2021. First, we found that the average prevalence of poor mental health across studies was 12.9% for severe depression, 26.0% for at least moderate depression, and 36.0% for at least mild depression. Second, we found that women reported significantly higher prevalence of probable depression than men in 63% of studies that reported depression levels by gender and that results on statistically significant differences between racial and ethnic groups were mixed. Third, we found that the 49 articles published were based on 12 studies; the most common sources were the Household Pulse Survey (n = 15, 31%), the AmeriSpeak panel (n = 8, 16%), the Qualtrics panel (n = 8, 16%), and the Understanding America Study (n = 5, 10%). Prevalence estimates varied based on mental health screening instruments and cutoffs used. The most commonly used instruments were the Patient Health Questionnaire (PHQ) (n = 36, 73%) and the Kessler (n = 8, 16%) series. While the prevalence of population depression varied over time depending on the survey instruments, severity, and constructs reported, the overall prevalence of depression remained high from March 2020 through June 2021 across instruments and severity. Understanding the scope of population mental health can help policymakers and providers address and prepare to meet the ongoing and future mental health needs of U.S. adults in the post-COVID-19 context and beyond.
1. Introduction
Depression is a leading cause of morbidity and reduced quality of life globally (Friedrich, 2017). In the U.S., it is estimated that depression cost an estimated $326 billion annually in healthcare fees, absenteeism (days of missed work due), and presenteeism (lowered productivity while at work) in 2018 (Greenberg et al., 2021). Depression is associated with a range of other negative health outcomes, including diabetes, cardiac disease, stroke, substance use, and premature mortality (Galea & Ettman, 2021; Kessler, 2012). Understanding the scope of population depressive symptoms can help inform decision making and public priorities that aim to reduce the burden of poor population mental health (Abdalla & Galea, 2021).
Depression is caused by a mix of genetic and environmental factors (Zajkowska et al., 2021), with economic and social determinants of health in particular shaping population mental health (Allen et al., 2014; Compton & Shim, 2015; Shim et al., 2012). The COVID-19 pandemic altered social and economic contexts; efforts to mitigate the virus caused major disruption and dismantled many of the factors that protect mental health such as social support, economic stability, routines, and access to resources like food, housing, and income (Shim, 2020). Efforts to contain the pandemic shifted behaviors: sleep patterns, eating habits, substance use, and social interaction changed (Czeisler, 2020; González-Monroy et al., 2021). The COVID-19 pandemic also brought about many stressors, which were themselves associated with poor mental health (Abdalla et al., 2021). It is therefore not surprising that a systematic review of studies comparing pre-versus post-pandemic depression found a significant increase in depression in U.S. adults (Robinson et al., 2022) at the start of the COVID-19 pandemic.
We do not know the prevalence of elevated depressive symptoms across studies in U.S. adults over the course of the COVID-19 pandemic. Reviews have been conducted globally (Salanti et al., 2022) and on sub-populations, such as healthcare workers (Li et al., 2021; Luo et al., 2020; Pappa et al., 2020; Sahebi et al., 2021), children and adolescents (Jones et al., 2021; Meherali et al., 2021; Panda et al., 2021), and COVID-19 patients (Deng et al., 2021; Renaud-Charest et al., 2021). Yet, no review to our knowledge has focused specifically on the prevalence of elevated symptoms of depression in U.S. adults beyond 2020. Robinson et al. (2022) conducted a systematic review of global longitudinal studies collected through July 2020 and reported a significant increase in the prevalence of depression, during relative to before, COVID-19 (Robinson et al., 2022). However, they reported on changes in depressive symptoms and did not report on the point prevalence of depression in U.S. adults through 2021. We also do not have a clear sense of whether prevalence of depression was mitigated over the course of the COVID-19 pandemic in U.S. adults as has been documented following other mass events (Goldmann & Galea, 2014) or if it remained elevated.
This paper aims to document the prevalence of depression in the population of U.S. adults as reported over the first year and five months of the COVID-19 pandemic in the peer reviewed literature. We aimed to document the population prevalence of depression across time, to identify patterns that emerged in the literature by race and gender, and to assess the methods used to determine population mental health during the pandemic. Previous work has suggested that tools used to screen for depression may measure different constructs in subpopulations (Barnes & Bates, 2017; Patel et al., 2019), so we also documented the screening tools, severity levels, and depression or depression related constructs reported. We use the term depression in this paper to represent probable depression and a range of related outcomes because the instruments reported in this review reflect screening tools measuring depressive symptoms, mental distress, and psychological distress. Previous studies showing differences in depression by gender and race/ethnicity groups motivated our goal to assess patterns in depression across these groups during the pandemic.
In sum, this paper aimed to.
-
1.
Document the prevalence of symptoms of depression in U.S. adults over the COVID-19 pandemic from 2020 to 2021.
-
2.
Summarize findings from the literature, identify patterns, and report comparative symptoms of depression prevalences across gender and race/ethnicity.
-
3.
Document the survey tools used to estimate population level depression symptoms, documenting the mental health screening instruments used, samples, and constructs reported throughout the pandemic.
2. Methods
We registered this systematic review in PROSPERO (CRD42021277976) and followed PRISMA guidelines to select included articles (Page et al., 2021).
3. Eligibility criteria
Articles were included if they were peer-reviewed quantitative articles, nationally representative of U.S. adults, and written in the English language. They must have reported a national depression or related prevalence during the COVID-19 pandemic. Articles were excluded if they studied a sub-population (for example, U.S. adults who had not experienced depression before COVID-19) or if they did not use a probability-based or quota sampling technique to ensure representativeness of the study sample. We excluded articles that used respondent driven sampling and convenience or snowball sampling (e.g., Amazon Mechanical Turk and social media platforms). Articles that only included a change or average score of depression (without a prevalence estimate) were excluded.
4. Search strategy
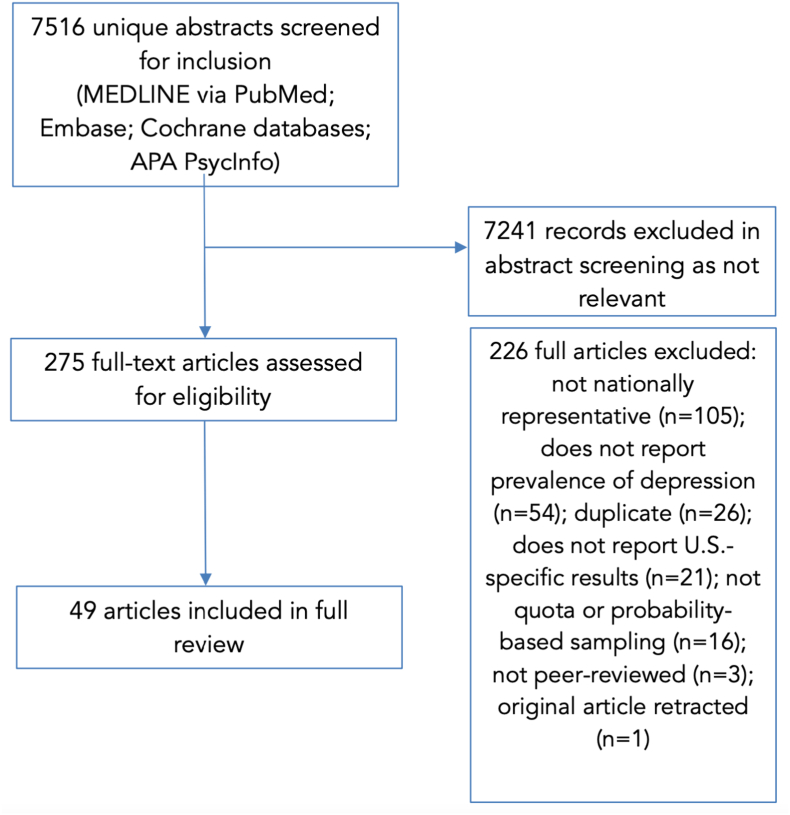
Articles published between January 2019 and May 16, 2022, were identified through a systematic search in MEDLINE via PubMed, Cochrane databases, Embase, and APA PsycInfo (Fig. 1). After deduplication in EndNote, 7516 unique articles were imported into Abstrackr, a free, online abstract screening tool developed at Brown University, USA (Wallace, Small, Brodley, Lau, & Trikalinos, 2012). The full search strategy can be found in Appendix A.
Fig. 1.
PRISMA flow-chart of article selection.
5. Screening
Two screeners (Removed for blind review) reviewed all abstracts. Following abstract screening, two screeners (Removed for blind review) read full text articles to determine eligibility. Disagreements between the two reviewers were resolved by the project lead (Removed for blind review).
6. Data extraction
Two authors (Removed for blind review) read the full text of all the articles and used a template for data extraction. Variables that were recorded from each of the articles were: date of publication, last date of data collection, data source, sampling technique, sample size, study design, depression screening tool, depression definition, number of waves, depression prevalence, and, if included, the findings stratified by gender and by race. For articles that reported multiple prevalence points of depression (such as longitudinal studies or serial cross-sectional studies), we extracted the dates of data collection for each prevalence point, the sample size that was used to estimate the prevalence of depression, and the details of the depression screener and severity measured at each time point.
6.1. Depression and mental distress screening instruments
To capture a comprehensive picture of mental health during the COVID-19 pandemic, we used a broad definition of depression to include depressive symptoms, psychological distress, and mental distress. Psychological distress is a separate but related construct that can include feelings of anxiety, depression, or general stress (Viertiö et al., 2021). Psychological or mental distress is a non-specific form of poor mental health that can impair functioning. A common scale for measuring psychological distress, the Kessler-6, includes in the screening instrument an item for frequency of feeling “so depressed that nothing could cheer you up” (Kessler et al., 2002). In this paper, depressive symptoms refers to the combination of poor mental health reported by screeners that measure depressive symptoms, psychological distress, and mental distress and related mental health constructs described in Supplemental Table 1 and Appendix B. We included studies that aggregated the prevalence of depression and anxiety and marked them as such. Although anxiety and depression are separate constructs, these results were included to maximize the number of articles included; results are presented separately in sensitivity analyses. To maximize articles in the review, we included articles that reported mild, moderate, and severe forms of depression. We disaggregated results by depression severity level. Where there was a discrepancy in the year published, we reported the year in which the article was published online instead of the print edition.
To document the methods of included articles, we reported the instruments used to measure mental health and the cutoff score reported when possible. We identified the depression or mental distress instrument core used (e.g., the Kessler or the PHQ), the specific version of instruments (e.g., PHQ-2 v. PHQ-9), and grouped articles accordingly. Severity of depression was defined as mild, moderate, and severe, using standard cutoff scores (Kim et al., 2017; Kroenke et al., 2001). We extracted outcomes measured by reporting the depression terminology reported by authors in the methods sections of articles (Supplemental Table 1). Sampling techniques were defined as probability based when articles reported use of probability-based techniques to recruit sample participants and non-probability based when articles used quota-based sampling techniques.
Because formal diagnosis of depression can only be made by a provider using DSM criteria, the constructs captured in survey data are positive screens for depression or related indicators. For example, the Patient Health Questionnaire (PHQ)-9 is a series of 9 questions used to screen individuals for depression. Participants are asked to describe how many days in the last two weeks (all the time, some of the time, none of the time) that they experienced the following: “Little interest or pleasure in doing things”; “Feeling down, depressed, or hopeless”; or “Trouble falling asleep or staying asleep, or sleeping too much” among others (Kroenke et al., 2001). Responses to the instrument are tallied to a final score, and the score is used to describe mild, moderate, or severe probable depression depending on cutoffs used. The PHQ-9, for example, has been validated against the gold standard of clinical diagnosis and has been found to have a sensitivity of 88% and a specificity of 88% relative to provider diagnosis. The PHQ (Kroenke et al., 2001), DASS (Antony et al., 1998), and CES-D (Radloff, 1977) measure probable depressive symptoms, and the Kessler series measures psychological distress. Details on depression or mental distress screening instruments can be found in Supplemental Table 2 and Appendix B.
7. Data analysis
7.1. Prevalence
The characteristics of included articles are described in Table 1. For reporting the prevalence of probable depression or mental distress by prevalence point, we documented moderate cutoffs when possible. If a study did not report a prevalence for moderate depression or mental distress, we reported the mild or severe prevalence estimate. If a study presented multiple categories of severity, we calculated the sum of the prevalence of “moderate” depression or distress and above across relevant instruments (Kroenke et al., 2001). Details on the process for calculating prevalence points can be found in Appendix B.
Table 1.
Characteristics of articles (n = 49) and prevalence points (n = 88) in review.
| Characteristic of articles | n (%) |
|---|---|
| Study design | |
| Cross-sectional | 29 (59%) |
| Serial cross-sectional | 15 (30%) |
| Longitudinal | 5 (10%) |
| Sampling technique | |
| Probability based | 37 (76%) |
| Non-probability sampling | 12 (24%) |
| Study data source | |
| Household Pulse Survey | 15 (31%) |
| AmeriSpeak | 8 (16%) |
| Qualtrics panel | 8 (16%) |
| Understanding America Study | 5 (10%) |
| Prolific Academic panel | 3 (6%) |
| Lucid | 3 (6%) |
| American Life Panel | 2 (4%) |
| Survey of Consumers | 1 (2%) |
| National Alcohol Survey | 1 (2%) |
| Ipsos KnowledgePanel | 1 (2%) |
| Dynata panel | 1 (2%) |
| Acumen Health Research Institute panel | 1 (2%) |
| Depression instrument core | |
| PHQ | 36 (73%) |
| Kessler | 8 (16%) |
| CES-D | 2 (4%) |
| DASS | 1 (2%) |
| Other | 2 (4%) |
| Instrument construct | |
| Depression | 41 (84%) |
| Depression or anxiety + | 8 (16%) |
| Used survey weights | |
| Yes | 41 (84%) |
| No | 3 (6%) |
| Did not state | 5 (10%) |
| Characteristic of prevalence points | |
| First date of data collection | March 10, 2020 (Daly, Sutin, & Robinson, 2020) |
| Last date of data collection | June 7, 2021 (Chen, Aruldass, & Cardinal, 2021) |
| Average sample size by prevalence point | 310,188 |
Note: HPS: Household Pulse Survey; UAS: Understanding America Survey; ALP: American Life Panel; NAS: United States National Alcohol Survey; CES-D: Center for Epidemiologic Studies––Depression Scale; DASS: Depression and Anxiety Stress Scale Test; PHQ: Patient Health Questionnaire.
Next, we estimated the average prevalence of depression reported across all prevalence points by month across mild, moderate, and severe depression or mental distress reported (Table 2). When a study did not explicitly define cutoffs by severity level, we used other studies included in our review to inform our judgment. If a study presented both unadjusted and adjusted results, we used the unadjusted results.
Table 2.
Average prevalence of depression by month over time by severity.
| Month of last date of data collection | Characteristics |
Prevalence of depression (%) |
|||
|---|---|---|---|---|---|
| Total prevalence points reported | Total sample size | Mild or above | Moderate or above | Severe or above | |
| 3/1/2020 | 4 | 19,774 | 29.0 | 14.5 | |
| 4/1/2020 | 13 | 1,023,590 | 31.7 | 24.9 | 16.8 |
| 5/1/2020 | 20 | 4,233,189 | 43.0 | 25.9 | 10.3 |
| 6/1/2020 | 10 | 3,336,599 | 30.9 | 28.2 | 10.8 |
| 7/1/2020 | 8 | 2,917,003 | 40.9 | 22.5 | 12.5 |
| 8/1/2020 | 3 | 1,425,249 | 26.1 | 24.5 | 10.2 |
| 9/1/2020 | 4 | 1,265,615 | 33.0 | 29.1 | 10.6 |
| 10/1/2020 | 4 | 1,125,850 | 33.4 | 13.4 | |
| 11/1/2020 | 3 | 988,982 | 46.0 | 13.7 | |
| 12/1/2020 | 8 | 3,797,550 | 39.10 | 26.9 | 13.8 |
| 1/1/2021 | 1 | 986,692 | 12.8 | ||
| 2/1/2021 | 2 | 987,195 | 12.4 | ||
| 3/1/2021 | 3 | 1,070,935 | 27.4 | 11.7 | |
| 4/1/2021 | 3 | 2,678,487 | 25.1 | 10.1 | |
| 5/1/2021 | 1 | 986,692 | 9.5 | ||
| 6/1/2021 |
1 |
453,167 |
20.3 |
||
| Total | 88 | 27,296,569 | 36.0 | 26.0 | 12.9 |
For estimating the average monthly prevalence of depression, we calculated the average prevalence of depression with data collection in that month, by severity level. When data collection spanned multiple months, we assigned the prevalence point to the month of the last date of data collection.
7.2. Gender and race/ethnicity comparisons
We reported the relative comparative depression prevalence between men and women and between racial and ethnic groups when reported (Table 3). To do this, we identified whether prevalence of probable depression was significantly higher, lower, or not different across gender and race/ethnicity groups. We labeled articles as “W > M” if articles reported that women had a significantly higher prevalence of depression than men, “M > W” if articles reported that men had a higher prevalence of depression than women, “W = M” if there was no significant difference, and “mixed findings” if there were significant differences reported within sub-groups. For reporting article findings by race/ethnicity, we described a study as “B > W” if Black populations reported depression more than White populations, “B < W” if White populations reported depression more, “B=W” if there was no significant difference, and “mixed findings” if there were significant differences based on subgroups. The same was reported for Hispanic (“H > W”, “H < W”, “H=W”) and Asian (“A > W”, “A < W”, “A = W”) populations. Statistically significant differences were based on a <0.05 p-value or 95% confidence intervals. If an article did not report statistical significance testing, we reported “N/A”.
Table 3.
Relative prevalence of depression by gender and race (n = 49).
| Relative groups | Relation | ||||
|---|---|---|---|---|---|
| Female to male populations | W > M | W < M | W = M | Mixed | Total |
| 17 (63%) | 2 (7%) | 8 (30%) | 0 (0%) | 27 (55%) | |
| Black to White populations | B > W | B < W | B=W | Mixed | Total |
| 7 (28%) | 8 (32%) | 8 (32%) | 2 (8%) | 25 (51%) | |
| Hispanic to White populations | H > W | H < W | H=W | Mixed | Total |
| 17 (35%) | 4 (15%) | 5 (19%) | 0 (0%) | 26 (53%) | |
| Asian to White populations | A > W | A < W | A = W | Mixed | Total |
| 0 (0%) | 10 (56%) | 7 (39%) | 1 (6%) | 18 (37%) | |
Note: Percentages in the total column represent the number of articles that reported on relative comparisons by group over the total articles in the review. Percentages in the other columns represent number of findings over articles that reported comparative results. B > W represents when Black populations report higher prevalence of depression than White populations; B < W represents when Black populations report lower prevalence of depression than White populations; B=W represents when Black populations prevalence at the same rate or at a level that is not significantly different than White populations; Mixed findings represent when findings differ across sub-populations or across prevalence points reported in papers.
7.3. Sensitivity analyses
To measure the variation in prevalence estimates based on article inclusion criteria, we calculated the average prevalence of depression by month using estimates that were unweighted and weighted by sample size (Supplemental Table 4 and Supplemental Fig. 8), full samples v. samples excluding non-probability-sample-based studies (Supplemental Table 5 and Supplemental Fig. 5), full samples v. samples excluding studies that reported presence of depression or anxiety (Supplemental Table 6 and Supplemental Fig. 6), and full samples v. samples excluding studies that reported presence of psychological distress (Supplemental Table 7 and Supplemental Fig. 7). We then graphed all prevalence points reported with a linear trendline by severity level and using the last day of data collection reported by each relevant study (Supplemental Fig. 9).
8. Results
Two authors (Removed for blind review) independently screened 7516 unique abstracts in Abstrackr. Abstracts marked for inclusion by either of the authors were included in full-text review. Two authors screened 275 articles in full text review. During full text review, 105 were not nationally representative of U.S. adults, 54 did not report a prevalence of depression, 26 were duplicates, 21 did not report U.S.-specific results, 16 did not use quota or probability-based sampling, 3 were not peer-reviewed, and one article was retracted. The final sample included 49 articles. Fig. 1 shows the distribution of articles through the search process.
8.1. Article characteristics
We identified 49 articles published in the peer review literature on the prevalence of depression in U.S. adults during the COVID-19 pandemic using nationally representative data from March 2020 through June 2021. Table 1 illustrates the characteristics of articles included in the review. Fifty-seven percent (n = 28) of studies used a cross-sectional design, 33% (n = 16) used a serial-cross sectional design, and 10% (n = 5) used a longitudinal design. Seventy-six percent (n = 37) of studies used a probability-based sampling technique to recruit study participants and the rest used quota sampling techniques. The 49 articles included in the review used a total of 12 data sources. The most published data source was the Household Pulse Survey (n = 15, 31%) followed by the NORC AmeriSpeak standing panel (n = 8, 16%) and Qualtrics panel (n = 8, 16%) and the Understanding America Study (n = 5, 10%). 27,296,569 participant prevalence points were included in the study, although this number includes people who were surveyed multiple times.
8.2. Prevalence point characteristics
We identified 88 unique prevalence points reported across the 49 articles in the review. The earliest reported prevalence point was March 10, 2020, and the last reported prevalence point was June 7, 2021, for a span of 16 months total. Fifty-three percent of the prevalence points (n = 47) included in this review were collected within the first four months of the pandemic (Table 2). The average number of days between last day of data collection and date of article publication was 205 days, with the shortest number of days being 45 (Czeisler, 2020) and the longest number of days being 634 (Martinez et al., 2022). Supplemental Fig. 1 shows the distribution of the count of prevalence points collected by month and the count of articles published by month. The distribution of prevalence points over time are presented by depression screening core tool (Supplemental Fig. 2), by detailed depression instrument and number of items in the instrument (Supplemental Fig. 3), and by study source (Supplemental Fig. 4).
8.3. Prevalence of depression by month of the pandemic
Table 2 shows the average prevalence of depression in each month of the pandemic through June 2021 by mild, moderate, and severe depression. Mild depression was reported in 10 prevalence points, moderate depression was reported in 53 prevalence points, and severe depression was reported in 24 prevalence points (Supplemental Table 3). The total average over the 16 months of reported prevalences of depression was 36% for mild depression, 26% for moderate depression, and 12.9% for severe depression.
In sensitivity analyses, we estimated the average prevalence of depression using weights for sample size (Supplemental Table 4), removing the studies that used non-probability-based samples (Supplemental Table 5), and removing the studies that reported combined depression or anxiety estimates (Supplemental Table 6) and psychological distress estimates (Supplemental Table 7). Results were within 1–2% of each other between different scenarios, except for mild depression, which most studies using depression or anxiety constructs reported. Supplemental Fig. 9 shows a visualization of the prevalence of depression across time featuring each prevalence point with visual depictions for severity, screening instrument used, and sample size.
8.4. Relative prevalence of depression by gender and race/ethnicity
Table 3 shows the relative prevalence of depression by gender and race. Fifty-five percent (n = 27) of studies reported prevalence by gender. Fifty-one percent (n = 25) of articles in the review showed Black to White population comparisons, 53% (n = 26) showed Hispanic to White population comparisons, and 37% (n = 18) showed Asian to White population comparisons. Among the studies that reported depression by gender, women had more depression in 63% of studies (n = 17); no significant difference by gender was reported in 30% of studies (n = 8) and 2 studies (7%) found that men had worse depression than women (details in Supplemental Table 8). Depression prevalence between White and Black populations was split with 28% of studies (n = 7) showing more depression among Black relative to White populations, 32% of studies (n = 8) showing less depression among Black relative to White populations, and 32% (n = 8) showing no difference in the prevalence of probable depression between Black and White populations. Thirty-five percent of studies showed that Hispanic persons had worse depression than White persons. No studies showed that Asian persons had worse depression than White persons in this review.
8.5. Methods used to define depression
Articles used different methods to measure population depression, which led to different severity scores and prevalence estimates across time. The most used depression instrument was the Patient Health Questionnaire (PHQ) with 73% of published articles using it (n = 36); 16% of articles used the Kessler screener (n = 8) and 4% of articles (n = 2) used the CES-D. Eighty-four percent of studies reported the construct of depression alone while 16% of studies (n = 8) reported a combined construct of depression or anxiety. Supplemental Table 1 shows the depression terms used by authors. Twenty percent of articles (n = 10) used the term “depression”, 18% (n = 9) used the term “depressive symptoms”, and 14% (n = 7) used the term “psychological distress” to describe the outcomes reported. Supplemental Table 2 illustrates the total depression instruments and severity scores reported, the total number of articles in each category, and the total sample size in each category. The most common instrument and cutoff combination was the PHQ-2 (with a cutoff of 3 or greater) (n = 20) followed by the Kessler-6 (with a cutoff of 13 or greater). Details on each instrument used, cutoff scores, and validation studies can be found in Appendix B. The distribution of depression severity by screening instrument used and the construct measured by each tool can also be found in Appendix B.
9. Discussion
In a systematic review of articles published during the first year and a half of the COVID-19 pandemic, we identified 49 articles that reported the prevalence of poor mental health (defined by probable depression or mental distress) in U.S. adults using nationally representative samples from March 2020 to June 2021. Among those articles, we identified 88 prevalence points that were reported. These studies showed that symptoms of depression and non-specific psychological distress remained high from March 2020 through June 2021: prevalence estimates averaged 36% for mild, 26% for moderate, and 12.9% for severe depression or psychological distress. Among studies that examined gender differences, 63% of studies reported that women had significantly greater depression or psychological distress than men. Among studies that examined racial differences, 28%, 35%, and 0% of studies showed that Black, Hispanic, and Asian populations, respectively, reported more depression or psychological distress than White populations. Prevalence estimates varied depending on instruments used, severity reported, and timing of data collection.
Much of our understanding of population depression during COVID-19 comes from 12 surveys. Further, focusing on date of collection rather than date of publication showed that there appeared to be a greater interest in measuring mental health at the start of the COVID-19 pandemic. Out of the 16 months of the pandemic covered by this review, more than half of the data on depression was collected in the first four months of the pandemic: between March 2020 and June 2020, there were 47 prevalence points of depression reported out of the 88 total points included in this review (53%). It is possible that interest in measuring mental health at the population level decreased over time or that there is a lag in publication; alternatively, there could also be higher standards for papers that contributed new knowledge after the initial wave of papers about mental health during COVID-19 were published. Additionally, although our search strategy collected articles published through May 2022, the most recently collected data that had been published was collected in June 2021. The lag between data collection and publication (Supplemental Fig. 1) is not new to the peer review process, however, it may be more important in times of mass emergencies for researchers and the media to highlight the dates of data collection, given rapidly evolving situations.
Depression was on the rise in U.S. adults before the COVID-19 pandemic (Weinberger et al., 2018) from 2005 to 2015. However, even the most recent estimates before COVID-19 suggest pre-pandemic prevalence levels were less than half of those reported during the pandemic: in 2019, prior to the COVID-19 pandemic, results from the CDC indicated that 11.5% of the U.S. adult population reported mild depressive symptoms, 4.2% reported moderate depressive symptoms, and 2.8% reported severe depressive symptoms (Villarroel & Terlizzi, 2020). Other nationally representative data, which were collected in 2013 and used the DSM-5 Major Depression Disorder Diagnostic Interview, estimated that 10.4% of U.S. adults experienced MDD in the last year (Hasin et al., 2018). Concerns have been raised about the extent to which measurements of mental health pre- and post-pandemic were assessing valid comparisons; for example, Kessler et al. summarize the challenges with interpreting estimates in changes of mental health from before to during the COVID-19 pandemic (Kessler et al., 2022). One goal of the current study was to highlight the heterogeneity of measurements used and the heterogeneity of results reported across studies conducted during the COVID-19 pandemic.
Our findings are within the range of prevalence estimates reported by reviews of depression globally. In a review of studies conducted in China, Italy, Turkey, Spain and Iran through May 2020, Luo et al. reported a pooled prevalence of depression of 28%. In a metanalysis of 14 studies on mental health conducted globally, Salari et al. reported a pooled prevalence of depression of 33.7%, relative to our estimates of 36% for mild depression and 26% for moderate depression or above (Salari et al., 2020). In a review of studies on mental health in Europe, Bonati et al. identified 16 studies that reported on depression and classified findings by mild, moderate, and severe depression (Bonati et al., 2022). In a review of articles on patients who tested positive for COVID-19, Deng et al. reported a prevalence of depression of 45% (Deng et al., 2021). A review of depression among healthcare workers through April 2020 reported a prevalence of depression of 22.8% (Pappa et al., 2020). Studies comparing prevalence of depression across countries have shown that the U.S. has reported some of the highest levels of depression relative to other countries (Généreux et al., 2020), which may explain why U.S. pooled prevalences would be slightly higher than those pooling depression across other countries.
Our findings are also consistent with other systematic reviews reporting on changes in mental health prevalence before and after community- and population-level disasters (North & Pfefferbaum, 2013), previous economic recessions (Mucci et al., 2016; Volkos & Symvoulakis, 2021), and other public health emergencies, including the H1N1 pandemic and Ebola, SARS, and MERS epidemics (Wang & Wang, 2021). This review adds further evidence that mental health should be included in public health responses following large-scale traumatic events.
We document gender and race/ethnicity differences in depression in the aftermath of COVID-19 that concur with those observed prior to the COVID-19 pandemic. The association between depression and female gender was documented widely before COVID-19 across countries and across the lifecourse (Piccinelli & Wilkinson, 2000; Salk et al., 2017). Within the U.S., nationally representative depression studies before the pandemic estimated the prevalence of depression to be almost two times higher in women than men (Ettman et al., 2020; Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings, n.d.). Our findings that 63% of studies in the U.S. showed that women had higher rates of depression is consistent with other systematic reviews conducted globally showing that female gender was a risk factor for depression during COVID-19 (Bonati et al., 2022; Mental Health and COVID-19: Early Evidence of the Pandemic's Impact: Scientific Brief, 2022, p. 19). Bonati et al. noted that female gender was the most common risk factor for depression in their review of studies conducted in Europe (Bonati et al., 2022). Comparisons of depression between race/ethnicity groups were mixed before COVID-19 (Bailey et al., 2019; Thomas Tobin et al., 2022; Williams, 2018) and remained mixed during COVID-19. It should be noted that multiple events occurred over the course of the COVID-19 pandemic and study period that could have contributed to the worsened mental health of racial and ethnic groups, including the highly visible deaths of unarmed Black men and women (Curtis et al., 2021) and other highly publicized shootings. Additionally, among articles that studied depression disparities across racial groups during the COVID-19 pandemic, there was a lack of comparisons for the Asian-American population relative to other minority racial groups, suggesting room for future research and inclusion in nationwide mental health assessments, particularly given increases in Asian-American discrimination during the COVID-19 pandemic (Chen et al., 2020; Zhou et al., 2021).
Although our study only included articles that reported a prevalence of depression, the findings from this review were consistent with the results in articles that reported mean scores of depression instead of a binary definition. For example, Wanberg et al. reported that depressive symptoms were higher during the pandemic relative to before the pandemic using a mean PHQ-8 score (Wanberg et al., 2020). Holman et al. found that depressive symptoms increased steadily from early March 2020 to late April 2020 across three waves of data collection in a large, probability-based nationally representative sample (Holman et al., 2020). Further, Hearne found that Hispanic persons reported a significantly higher mean score of depressive symptoms relative to White persons (Hearne, 2021). However, it is important to note that these three articles only used data from March and April 2020, illustrating that many of the gaps in data we find in our systematic review remain the same across the literature.
Finally, our third finding that depression prevalences varied considerably depending on methods deployed adds to a literature that assesses quality of data collection and that encourages close attention to mental health metrics being reported—particularly to the general public. Even before the COVID-19 pandemic, methodologists explored potential frameworks for evaluating quality surveys and reducing bias in samples that were not probability based (Baker et al., 2013; Cornesse et al., 2020) despite evidence that probability based samples remained the most accurate (MacInnis et al., 2018). For example, some evaluations have found online samples to be biased particularly for representing racial and ethnic minorities (Kennedy et al., 2016). In the case of the COVID-19 pandemic, there was a particularly compelling need for rapid work that could help institutions understand the scope of population mental health. As a result, we found that while the majority of studies included in the review used probability-based sampling, several high visibility studies used non-probability-based studies. We conducted multiple sensitivity analyses and presented findings across severity levels and across depression instruments in the hopes of showing the differences in findings depending on the constructs measured and reported by articles. The fact that only 12 studies informed our collective understanding of national mental health suggests that having ongoing mental health standing surveys is important for appropriate pre- and post-event comparisons; investing in infrastructure that allows for ongoing surveillance of population mental health can be valuable to researchers and the public alike. Additionally, although many studies noted that they were nationally representative, not all studies provided clear details on their sampling methods. The field would benefit if researchers conducting work that is intended to be nationally representative provided clear details either in their primary manuscripts or supplemental materials that note efforts in the study design and analysis stages (e.g., noting the sampling frame for samples, sampling techniques, and weighting strategy) to align samples with national populations.
Interpretation of the burden of depression in the U.S. adult population during COVID-19 should consider the methods, constructs, and severities reported in articles. It is noteworthy that articles reporting from the same data source over the same months reported different prevalences of depression; for example, Cai et al. and Park et al. both used the Household Pulse Survey to estimate depression in the months of April and May 2020. Cai et al. reported a prevalence of 35.9% and Park et al. reported a prevalence of 24.5%; this may be attributed to the fact that Park et al. measured the prevalence of positive screening for anxiety or depression (using the PHQ-4), while Cai et al. just assessed major depressive disorder (PHQ-2). This illustrates the need and sets further motivation to read closely and understand the severity of depression measured, instruments used, and the timing of data collection. The importance of these factors cannot be overstated while drawing conclusions from data; although similar data sources may be used during the same period of time, there are a number of factors that might influence heterogeneity in results. Accordingly, policymakers, reporters, and readers in general of articles on depression during the COVID-19 pandemic should make note of the severity of depression being reported, the time when data were collected, and the depression instruments used to ascertain poor mental health.
9.1. Limitations
This paper has five main limitations. First, this review does not provide a formal meta-analysis of prevalence estimates; the studies included in the review did not consistently report standard errors and, thus, we were unable to create appropriate estimates of total prevalence of depression over time. However, we grouped studies that were similar in severity and instruments to best present and compare relevant estimates. Second, the review did not include studies that reported only a continuous depression score. There were several nationally representative studies conducted that did not report binary cutoffs that can inform general trends in depression. We aimed to focus this analysis on clinically relevant cutoffs that could inform care and public health practice. We also report findings in this discussion on some of the excluded articles that reported means, whose patterns were similar to those reported by the articles included in this review. Third, some studies collected data across multiple months. To facilitate analyses, we used the last month of data collection. It is possible that the mental health of participants could have varied significantly across data collection. However, the majority of studies reported data collected within the same calendar month. Fourth, some aggregate point estimates were calculated manually. Because we were not able to use the survey weights used in articles, it is possible that these estimates may not represent the U.S. population as well as they would using weights from the original data. Our aggregation of findings that were weighted originally mitigates this concern. Fifth, this study combined psychological distress and depression as our main outcome of interest. The literature is unclear on differences and similarities between psychological distress and depression with blurring of lines between the two. There are ongoing debates on the measurement of mental health (Fried et al., 2022; Vanheule & Devisch, 2014) and the constructs used to measure mental health problems (Fried, 2022). We aimed to provide disaggregated results by mental health screeners and by severity levels to show the heterogeneity of results depending on the measurement instruments used. In sensitivity analyses, we removed the papers that captured psychological distress; the monthly average score for mild depression remained the same and the monthly average scores for moderate and severe depression decreased slightly, from 26% to 25.4% and from 12.9% to 11.8%, respectively. We also note that common screeners for psychological distress include as items questions about feeling depressed; in this way, the current review helps to get closer to understanding the burden of poor mental health during the COVID-19 pandemic and the variation in results depending on study design.
10. Conclusion
The current peer-reviewed literature shows an elevated prevalence of depression during COVID-19 that was sustained from Spring 2020 through Spring 2021. The instruments that have been used across studies provided different estimates of population mental health, suggesting heterogeneous estimates of the prevalence of depression and psychological distress during COVID-19. Understanding the population level burden of poor mental health is critical for policy makers and providers to plan and prepare to address the needs of patients. Consumers of research in this area should be aware of different levels of depression severity, sampling techniques, and mental health constructs reported by individual studies when reporting on study findings to best articulate the mental health status and needs of U.S. adults. Having accurate and ongoing estimates of mental health over time, as well as a deeper understanding of the methodologies behind them, is important for tracking population health and should be an expected standard for population health going forward.
Financial disclosure statement
The authors have no financial statements to disclose. Dr. Ettman’s time was supported in part by a gift from Meta (PI: Stuart). Dr. Galea's time was supported in part by Grant NIMH R01MH119193 from the National Institute of Mental Health (PI: Galea). Dr. Stuart’s time was supported in part by Grant R01MH115487 from the National Institute of Mental Health (PI: Stuart).
Ethical statement
This material is the authors' own original work, which has not been previously published elsewhere.
The paper is not currently being considered for publication elsewhere.
The paper reflects the authors' own research and analysis in a truthful and complete manner.
Declaration of competing interest
The authors have no conflicts of interest to disclose.
Acknowledgements
The authors wish to thank Frauke Kreuter for help in thinking through strengths and challenges of survey design and measurement.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2023.101348.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
Data availability
Data are available in the supplemental materials.
References
- Abdalla S.M., Ettman C.K., Cohen G.H., Galea S. Mental health consequences of COVID-19: A nationally representative cross-sectional study of pandemic-related stressors and anxiety disorders in the USA. BMJ Open. 2021;11(8) doi: 10.1136/bmjopen-2020-044125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdalla S.M., Galea S. The 3-D commission: Forging a transdisciplinary synthesis at the intersection of social determinants of health, data, and decision-making. Journal of Urban Health. 2021;98(S1):1–3. doi: 10.1007/s11524-021-00555-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen J., Marmot M., World Health Organization, & Fundação Calouste Gulbenkian . 2014. Social determinants of mental health.http://apps.who.int/iris/bitstream/10665/112828/1/9789241506809_eng.pdf?ua=1 [Google Scholar]
- Antony M.M., Bieling P.J., Cox B.J., Enns M.W., Swinson R.P. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10(2):176–181. doi: 10.1037/1040-3590.10.2.176. [DOI] [Google Scholar]
- Bailey R.K., Mokonogho J., Kumar A. Racial and ethnic differences in depression: Current perspectives. Neuropsychiatric Disease and Treatment. 2019;15:603–609. doi: 10.2147/NDT.S128584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker R., Brick J.M., Bates N., Battaglia M., Couper M., Dever J., Gile K., Roger R. American Association for Public Opinion Research; 2013. Non-probability sampling: Report of the AAPOR task force on non-probability sampling.https://www.aapor.org/Education-Resources/Reports/Non-Probability-Sampling.aspx [Google Scholar]
- Barnes D.M., Bates L.M. Do racial patterns in psychological distress shed light on the black–white depression paradox? A systematic review. Social Psychiatry and Psychiatric Epidemiology. 2017;52(8):913–928. doi: 10.1007/s00127-017-1394-9. [DOI] [PubMed] [Google Scholar]
- Bonati M., Campi R., Segre G. 2022. Psychological impact of the quarantine during the COVID-19 pandemic on the general European adult population: A systematic review of the evidence—PMC.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9069583/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J.A., Zhang E., Liu C.H. Potential impact of COVID-19–related racial discrimination on the health of Asian Americans. American Journal of Public Health. 2020;110(11):1624–1627. doi: 10.2105/AJPH.2020.305858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Aruldass A.R., Cardinal R.N. Mental health outcomes after SARS-CoV-2 vaccination in the United States: A national cross-sectional study. Journal of Affective Disorders. 2021;298:396–399. doi: 10.1016/j.jad.2021.10.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton M.T., Shim R.S. The social determinants of mental health. FOCUS. 2015;13(4):419–425. doi: 10.1176/appi.focus.20150017. [DOI] [Google Scholar]
- Cornesse C., Blom A.G., Dutwin D., Krosnick J.A., De Leeuw E.D., Legleye S., Pasek J., Pennay D., Phillips B., Sakshaug J.W., Struminskaya B., Wenz A. A review of conceptual approaches and empirical evidence on probability and nonprobability sample survey research. Journal of Survey Statistics and Methodology. 2020;8(1):4–36. doi: 10.1093/jssam/smz041. [DOI] [Google Scholar]
- Curtis D.S., Washburn T., Lee H., Smith K.R., Kim J., Martz C.D., Kramer M.R., Chae D.H. Highly public anti-Black violence is associated with poor mental health days for Black Americans. Proceedings of the National Academy of Sciences. 2021;118(17) doi: 10.1073/pnas.2019624118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É. Vol. 69. MMWR. Morbidity and Mortality Weekly Report; 2020. (Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Sutin A.R., Robinson E. Depression reported by US adults in 2017–2018 and March and April 2020. Journal of Affective Disorders. 2020;278:131–135. doi: 10.1016/j.jad.2020.09.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J., Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., Huang E., Zuo Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID‐19 patients: A meta‐analysis. Annals of the New York Academy of Sciences. 2021;1486(1):90–111. doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. e2019686–e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E.I. Studying mental health problems as systems, not syndromes. Current Directions in Psychological Science. 2022 doi: 10.1177/09637214221114089. [DOI] [Google Scholar]
- Fried E.I., Flake J.K., Robinaugh D.J. Revisiting the theoretical and methodological foundations of depression measurement. Nature Reviews Psychology. 2022;1(6):358–368. doi: 10.1038/s44159-022-00050-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedrich M.J. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517. doi: 10.1001/jama.2017.3826. [DOI] [PubMed] [Google Scholar]
- Galea S., Ettman C.K. Mental health and mortality in a time of COVID-19. American Journal of Public Health. 2021;111(S2):S73–S74. doi: 10.2105/AJPH.2021.306278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Généreux M., Schluter P.J., Hung K.K., Wong C.S., Pui Yin Mok C., O'Sullivan T., David M.D., Carignan M.-E., Blouin-Genest G., Champagne-Poirier O., Champagne É., Burlone N., Qadar Z., Herbosa T., Ribeiro-Alves G., Law R., Murray V., Chan E.Y.Y., Pignard-Cheynel N.…Roy M. One virus, four continents, eight countries: An interdisciplinary and international study on the psychosocial impacts of the COVID-19 pandemic among adults. International Journal of Environmental Research and Public Health. 2020;17(22):8390. doi: 10.3390/ijerph17228390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annual Review of Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- González-Monroy C., Gómez-Gómez I., Olarte-Sánchez C.M., Motrico E. Eating behaviour changes during the COVID-19 pandemic: A systematic review of longitudinal studies. International Journal of Environmental Research and Public Health. 2021;18(21) doi: 10.3390/ijerph182111130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg P.E., Fournier A.-A., Sisitsky T., Simes M., Berman R., Koenigsberg S.H., Kessler R.C. The economic burden of adults with major depressive disorder in the United States (2010 and 2018) PharmacoEconomics. 2021;39(6):653–665. doi: 10.1007/s40273-021-01019-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D.S., Sarvet A.L., Meyers J.L., Saha T.D., Ruan W.J., Stohl M., Grant B.F. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. doi: 10.1001/jamapsychiatry.2017.4602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hearne B.N. Psychological distress across intersections of race/ethnicity, gender, and marital status during the COVID-19 pandemic. Ethnicity and Health. 2021:1–20. doi: 10.1080/13557858.2021.1969537. [DOI] [PubMed] [Google Scholar]
- Holman E.A., Thompson R.R., Garfin D.R., Silver R.C. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Science Advances. 2020;6(42):eabd5390. doi: 10.1126/sciadv.abd5390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones E.A.K., Mitra A.K., Bhuiyan A.R. Impact of COVID-19 on mental health in adolescents: A systematic review. International Journal of Environmental Research and Public Health. 2021;18(5):2470. doi: 10.3390/ijerph18052470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy C., Mercer A., Keeter S., Hatley N., McGeeney K., Gimenez A. Evaluating online nonprobability surveys [pew research center]. Evaluating online nonprobability surveys. 2016. https://www.pewresearch.org/methods/2016/05/02/evaluating-online-nonprobability-surveys/ May 2.
- Kessler R.C. The costs of depression. Psychiatric Clinics of North America. 2012;35(1):1–14. doi: 10.1016/j.psc.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.-L.T., Walters E.E., Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Chiu W.T., Hwang I.H., Puac-Polanco V., Sampson N.A., Ziobrowski H.N., Zaslavsky A.M. Changes in prevalence of mental illness among US adults during compared with before the COVID-19 pandemic. Psychiatric Clinics of North America. 2022;45(1):1–28. doi: 10.1016/j.psc.2021.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Chung H., Askew R.L., Park R., Jones S.M.W., Cook K.F., Amtmann D. Translating CESD-20 and PHQ-9 scores to PROMIS depression. Assessment. 2017;24(3):300–307. doi: 10.1177/1073191115607042. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Scherer N., Felix L., Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0246454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—a systematic review and meta-analysis. Psychiatry Research. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacInnis B., Krosnick J.A., Ho A.S., Cho M.-J. The accuracy of measurements with probability and nonprobability survey samples: Replication and extension. Public Opinion Quarterly. 2018;82(4):707–744. doi: 10.1093/poq/nfy038. [DOI] [Google Scholar]
- Martinez P., Karriker-Jaffe K.J., Ye Y., Patterson D., Greenfield T.K., Mulia N., Kerr W.C. Mental health and drinking to cope in the early COVID period: Data from the 2019–2020 US National Alcohol Survey. Addictive Behaviors. 2022;128 doi: 10.1016/j.addbeh.2022.107247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meherali S., Punjani N., Louie-Poon S., Abdul Rahim K., Das J.K., Salam R.A., Lassi Z.S. Mental health of children and adolescents amidst COVID-19 and past pandemics: A rapid systematic review. International Journal of Environmental Research and Public Health. 2021;18(7):3432. doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mental health and COVID-19 . 2022. Early evidence of the pandemic's impact: Scientific brief.https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 World Health Organization. [Google Scholar]
- Mucci N., Giorgi G., Roncaioli M., Fiz Perez J., Arcangeli G. The correlation between stress and economic crisis: A systematic review. Neuropsychiatric Disease and Treatment. 2016;12:983–993. doi: 10.2147/NDT.S98525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North C., Pfefferbaum B. Mental health response to community disasters a systematic review. JAMA, the Journal of the American Medical Association. 2013;310(5):5. doi: 10.1001/jama.2013.107799. [DOI] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D.…Moher D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. The BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda P.K., Gupta J., Chowdhury S.R., Kumar R., Meena A.K., Madaan P., Sharawat I.K., Gulati S. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: A systematic review and meta-analysis. Journal of Tropical Pediatrics. 2021;67(1) doi: 10.1093/tropej/fmaa122. fmaa122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel J.S., Oh Y., Rand K.L., Wu W., Cyders M.A., Kroenke K., Stewart J.C. Measurement invariance of the patient health questionnaire-9 (PHQ-9) depression screener in U.S. Adults across sex, race/ethnicity, and education level: NHANES 2005-2016. Depression and Anxiety. 2019;36(9):813–823. doi: 10.1002/da.22940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccinelli M., Wilkinson G. Gender differences in depression: Critical review. The British Journal of Psychiatry. 2000;177(6):486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Renaud-Charest O., Lui L.M.W., Eskander S., Ceban F., Ho R., Di Vincenzo J.D., Rosenblat J.D., Lee Y., Subramaniapillai M., McIntyre R.S. Onset and frequency of depression in post-COVID-19 syndrome: A systematic review. Journal of Psychiatric Research. 2021;144:129–137. doi: 10.1016/j.jpsychires.2021.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings. (n.d.). 142.
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahebi A., Nejati-Zarnaqi B., Moayedi S., Yousefi K., Torres M., Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salanti G., Peter N., Tonia T., Holloway A., White I.R., Darwish L., Low N., Egger M., Haas A.D., Fazel S., Kessler R.C., Herrman H., Kieling C., De Quervain D.J.F., Vigod S.N., Patel V., Li T., Cuijpers P., Cipriani A. The impact of the COVID-19 pandemic and associated control measures on the mental health of the general population: A systematic review and dose–response meta-analysis. Annals of Internal Medicine. 2022;M22–1507 doi: 10.7326/M22-1507. MHCOVID Crowd Investigators. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health. 2020;16(1):57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk R.H., Hyde J.S., Abramson L.Y. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin. 2017;143(8):783–822. doi: 10.1037/bul0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim R.S. Mental health inequities in the context of COVID-19. JAMA Network Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.20104. e2020104–e2020104. [DOI] [PubMed] [Google Scholar]
- Shim R.S., Ye J., Baltrus P., Fry-Johnson Y., Daniels E., Rust G. Racial/ethnic disparities, social support, and depression: Examining a social determinant of mental health. Ethnicity & Disease. 2012;22(1):15–20. [PMC free article] [PubMed] [Google Scholar]
- Thomas Tobin C.S., Erving C.L., Hargrove T.W., Satcher L.A. Is the Black-White mental health paradox consistent across age, gender, and psychiatric disorders? Aging & Mental Health. 2022;26(1):196–204. doi: 10.1080/13607863.2020.1855627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanheule S., Devisch I. Mental suffering and the DSM-5: A critical review: Mental suffering and the DSM-5: A critical review. Journal of Evaluation in Clinical Practice. 2014;20(6):975–980. doi: 10.1111/jep.12163. [DOI] [PubMed] [Google Scholar]
- Viertiö S., Kiviruusu O., Piirtola M., Kaprio J., Korhonen T., Marttunen M., Suvisaari J. Factors contributing to psychological distress in the working population, with a special reference to gender difference. BMC Public Health. 2021;21(1):611. doi: 10.1186/s12889-021-10560-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarroel M.A., Terlizzi E.P. Symptoms of depression among adults. United States. 2020;379:8. 2019. [PubMed] [Google Scholar]
- Volkos P., Symvoulakis E.K. Impact of financial crisis on mental health: A literature review ‘puzzling’ findings from several countries. International Journal of Social Psychiatry. 2021;67(7):907–919. doi: 10.1177/00207640211011205. [DOI] [PubMed] [Google Scholar]
- Wallace B.C., Small K., Brodley C.E., Lau J., Trikalinos T.A. Proceedings of the 2nd ACM SIGHIT International Health Informatics Symposium. 2012. Deploying an interactive machine learning system in an evidence-based practice center: Abstrackr; pp. 819–824. [DOI] [Google Scholar]
- Wanberg C.R., Csillag B., Douglass R.P., Zhou L., Pollard M.S. Socioeconomic status and well-being during COVID-19: A resource-based examination. Journal of Applied Psychology. 2020;105(12):1382–1396. doi: 10.1037/apl0000831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Wang D. The influence and enlightenment of five public health emergencies on public psychology since new century: A systematic review. International Journal of Social Psychiatry. 2021;67(7):878–891. doi: 10.1177/00207640211002222. [DOI] [PubMed] [Google Scholar]
- Weinberger A.H., Gbedemah M., Martinez A.M., Nash D., Galea S., Goodwin R.D. Trends in depression prevalence in the USA from 2005 to 2015: Widening disparities in vulnerable groups. Psychological Medicine. 2018;48(8):1308–1315. doi: 10.1017/S0033291717002781. [DOI] [PubMed] [Google Scholar]
- Williams D.R. Stress and the mental health of populations of color: Advancing our understanding of race-related stressors. Journal of Health and Social Behavior. 2018;59(4):466–485. doi: 10.1177/0022146518814251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajkowska Z., Walsh A., Zonca V., Gullett N., Pedersen G.A., Kieling C., Swartz J.R., Karmacharya R., Fisher H.L., Kohrt B.A., Mondelli V. A systematic review of the association between biological markers and environmental stress risk factors for adolescent depression. Journal of Psychiatric Research. 2021;138:163–175. doi: 10.1016/j.jpsychires.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S., Banawa R., Oh H. The mental health impact of COVID-19 racial and ethnic discrimination against Asian American and pacific islanders. Frontiers in Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.708426. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available in the supplemental materials.