Abstract
The atypical spindle cell/pleomorphic lipomatous tumor (ASPLT) was classified as a new tumor by the World Health Organization (WHO) in 2020. The tumor is benign and commonly occurs in the limbs. Paraspinal presentations are rare. A 38‐year‐old man presented at our clinic complaining of sudden onset back pain. No neurological deficit was found. The magnetic resonance imaging (MRI) revealed a well‐defined heterogeneous mass in the left psoas muscle, from L1 to L3 extending over the L1 and L2 neuroforamen. The tumor was totally excised. Pathology led to an ASPLT diagnosis. Clinical symptoms improved and there was no postsurgical neurological deficit. This case of ASPLT, located in an uncommon location and present an unusual cluster of symptoms, could be treated by surgical excision, usually the first‐treatment strategy. Totally, removal was achieved because there was a clear morphological margin. The risk of metastatic dissemination was minimal, though there remains a nonnegligible risk of local recurrence.
Keywords: atypical spindle cell/pleomorphic lipomatous tumor (ASPLT), paraspinal
1. BACKGROUND
Atypical spindle cell/pleomorphic lipomatous tumor (ASPLT) is characterized as a primary neoplasm of fat content within the papillary and reticular formation tissue. 1 Pathologically, ASPLTs are benign adipocytic tumors and were found positive for CD34 but either negative or only minimally immunoreactive for MDM2 and CDK4. Although they have been reported to be distributed in various locations in humans, most of these tumors occur on the limbs. 2 , 3 In this study, we present a rare case of a typical spindle cell lipomatous tumor unusually located in the paraspinal region.
2. CASE PRESENTATION
A 38‐year‐old man presented in our clinic complaining of sudden onset back pain. This patient denied any history of trauma and exhibited no sensory or motor deficit. He also disaffirmed any medical, family, and surgical history. Computed tomography (CT) and magnetic resonance imaging (MRI) showed a well‐defined heterogeneous contrast‐enhanced mass, nearly 11.5 cm × 2 cm × 2 cm, in the left paraspinal region embedded in the left pasos muscle. The mass extended from L1 to L3 over L1 and L2 neuroforamen (Figure 1A,B).
FIGURE 1.
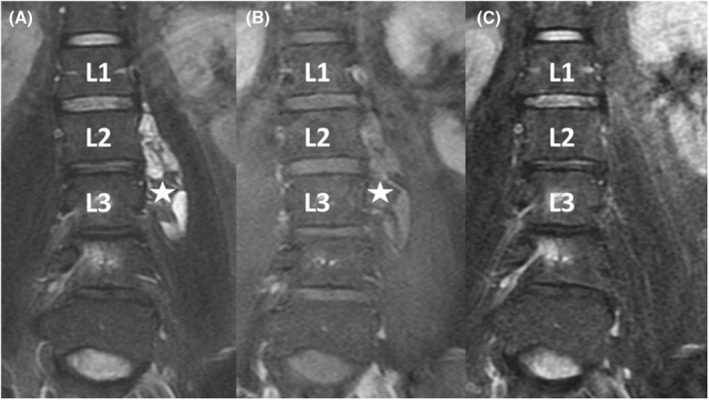
Lumbar MRI scan revealed a well‐defined lesion (see the star in the image) at the left L1–L3 paraspinal area on T2‐weighted image (A) with heterogenous enhancement (B). Postoperative MRI revealed total tumor removal (C). Pathology proved an atypical spindle cell lipomatous tumor.
The patient received surgical excision under general anesthesia. During the surgery, he was placed in a prone position and a C‐arm fluoroscopy was used to locate the L2 level. A paramedian skin incision was performed revealing the left side L2 and L3 transverse processes, which were removed by a high‐speed drill. Under the microscope, the tumor was seen to have a clear margin between the tumor and the surrounding tissue. The mass was removed using a cavitron ultrasonic surgical aspirator (CUSA). It was sent to pathology and the wound was closed after meticulously checking for bleeding. The patient recovered well, and his symptoms improved. Postoperative MRI confirmed the total removal of the tumor (Figure 1C).
Permanent tissue analysis of the specimen (hematoxylin and eosin) revealed increased cellularity of proliferative spindle cell components with minimal nuclear atypia and admixed adipocytic cells, including scant lipoblasts, in the fibromyxoid stroma with stout ropy collagen fibers (Figure 2A,B). Immunohistochemistry (IHC) showed the neoplastic cells to be positive for CD34 and p16 (focal) but negative for MDM2, CDK4, S100, and desmin (Figure 2C). The Rb expression was reduced to absent (Figure 2D), and p53 revealed wild‐type expression. Based on these findings, we were able to come to a final diagnosis of atypical spindle cell lipomatous.
FIGURE 2.
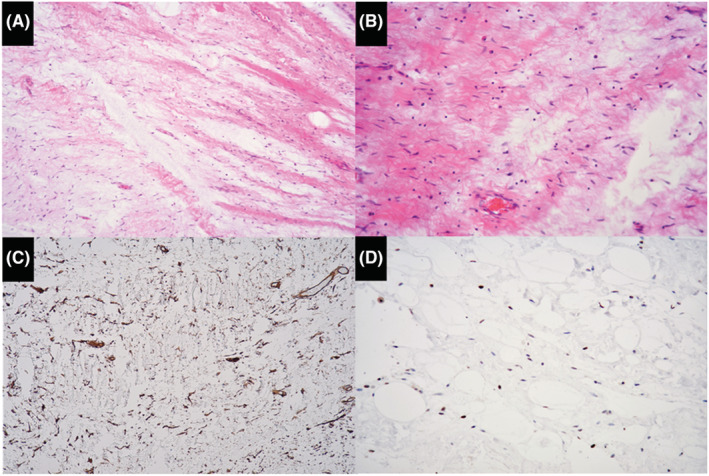
Pathology of resected atypical spindle cell lipomatous tumor showed increased cellularity of proliferative spindle cell components with minimal nuclear atypia and admixed adipocytic cells in the fibromyxoid stroma with stout ropy collagen fibers. Tumor cells demonstrated positive reactivity with CD34 and Rb. (A) Hematoxylin and eosin (H&E) stain, ×100, (B) H&E, ×200, (C) CD34, ×100, (D) RB, ×200.
3. DISCUSSION AND CONCLUSION
ASPLT is an extremely rare liposarcoma with a low potential for malignancy. 4 The original description of spindle cell liposarcoma focused on a group of atypical adipocytic neoplasms with spindle cell morphology, clinically characterized as having a striking tendency for local recurrence. According to the Fifth Edition of the World Health Organization (WHO) Classification of Tumors of Soft Tissue and Bone, published in early 2020, liposarcoma can be further categorized as pleomorphic liposarcoma, spindle cell/pleomorphic lipoma, and atypical lipomatous tumors. 5
Although the distribution of the tumors over the body is reported to vary, they predominately occur in the limbs and limb girdles, mainly in the hands and feet, with equal distribution between subcutaneous and deeper locations. 2 Clinically, the neoplasm presents as a persistent or enlarging mass. Under H&E staining, ASPLT is observed to have a disparate histologic appearance with varying degrees of mildly to moderately an atypical spindle cells, lipoblasts, and pleomorphic multinucleated cells in a matrix ranging from myxoid to collagenous. A definite diagnosis can be obtained using immunohistochemical staining. Tissue samples are often found to express CD34, which helps in its differential diagnosis. Other features that help distinguish ASPLT from other liposarcomas are loss or minor expression of Rb and no expression of murine double minute 2 (MDM2). These neoplastic cells frequently express CD34 (64%), S100 (40%), and desmin (22%). 6 The immunohistochemistry of the neoplastic cells in our case revealed positive expression of focal CD34 and p16 and negative expression of MDM2, CDK4, S100, and desmin. The Rb showed reduced to absent expression, and the p53 revealed wild‐type expression. These findings led to a final diagnosis of atypical spindle cell/pleomorphic lipomatous tumor.
The literature characterized ASPLTs as clinically benign lesions best treated by surgical excision. Although the tumor is characterized as having well‐defined margins due to lower infiltrative growth patency, there still exists a nonnegligible tendency for local recurrence, 12%. 7 The potential for metastasis seems minimal, possibly nonexistent. Most patients with ASPLT will have an excellent prognosis if the lesion is completely excised. Our case was successfully treated by surgical excision with no postsurgical neurological deficit. The patient's symptoms clearly improved and postoperative MRI confirmed the total removal of the lesion.
AUTHOR CONTRIBUTIONS
All authors were involved in the case report. Drafted the manuscript: Y‐W Cheng. Figures design: Y‐Y Chen. Crucially revised the manuscript: C‐H Kuo and W‐C Liao. Finalized the manuscript: Y‐W Cheng and A‐L Kwan.
FUNDING INFORMATION
Not applicable.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
ETHICS APPROVAL
This study was reviewed and approved by the Ethics Committee of Kaohsiung Veterans General Hospital. The patient was not required to provide informed consent because the analysis used anonymous clinical data and images that were obtained after the patient agreed to examinations and treatment by verbal and written consent. This study strictly followed the CARE guidelines.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENT
We are grateful for support from the Ministry of Science and Technology of Taiwan under Contract numbers of MOST 110‐2314‐B‐075B‐001‐MY21.
Cheng Y‐W, Chen Y‐Y, Kuo C‐H, Liao W‐C, Kwan A‐L. Lumbar paraspinal atypical spindle cell/pleomorphic lipomatous tumor: A report of a rare case. Clin Case Rep. 2023;11:e06868. doi: 10.1002/ccr3.6868
DATA AVAILABILITY STATEMENT
Considering the patient's privacy, the clinical information and images are available upon reasonable request to the first author for further application.
REFERENCES
- 1. Tchack MS, Broscius M, Reichel M. Primary cutaneous atypical spindle cell lipomatous tumor. Case Rep Pathol. 2021;2021:4082289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mariño‐Enriquez A, Nascimento AF, Ligon AH, Liang C, Fletcher CD. Atypical spindle cell lipomatous tumor: clinicopathologic characterization of 232 cases demonstrating a morphologic spectrum. Am J Surg Pathol. 2017;41(2):234‐244. [DOI] [PubMed] [Google Scholar]
- 3. Creytens D, Mentzel T, Ferdinande L, et al. “Atypical” pleomorphic lipomatous tumor: a clinicopathologic, immunohistochemical and molecular study of 21 cases, emphasizing its relationship to atypical spindle cell lipomatous tumor and suggesting a morphologic spectrum (atypical spindle cell/pleomorphic lipomatous tumor). Am J Surg Pathol. 2017;41(11):1443‐1455. [DOI] [PubMed] [Google Scholar]
- 4. Yoshida Y, Nakabayashi M, Harada Y, Shingu T, Takubo K. A case report of atypical spindle cell lipomatous tumor of the tongue. Yonago Acta Med. 2020;63(3):223‐227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kallen ME, Hornick JL. The 2020 WHO Classification: what's new in soft tissue tumor pathology? Am J Surg Pathol. 2021;45(1):e1‐e23. [DOI] [PubMed] [Google Scholar]
- 6. Memon R, Abdelfatah MM, Patel C, et al. Atypical spindle cell/pleomorphic lipomatous tumor of the stomach: a case report. Hum Pathol Case Rep. 2021;25:200540. [Google Scholar]
- 7. Wehrle CJ, Daigle JW, Ullah A, Sharma S, Ritter EF, Kruse EJ. Atypical spindle cell lipomatous lesion resected from patient with history of CLL. Am Surg. 2020;86(9):1208‐1211. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Considering the patient's privacy, the clinical information and images are available upon reasonable request to the first author for further application.


