Abstract
Aims
Atherosclerotic cardiovascular disease (ASCVD) risk prediction equations apply to older adults. For this study, the Pathobiologic Determinants of Atherosclerosis in Youth (PDAY) risk score, based on post-mortem measurements of atherosclerosis in 15–34-year olds dying accidentally, was used to predict ASCVD events, specifically myocardial infarction and revascularization, in middle age, from risk measured at ≤40 years of age.
Methods and results
The Coronary Artery Risk Development in Young Adults Study (CARDIA) collected longitudinal cardiovascular risk data, coronary artery calcium (CAC) scores, and ASCVD data beginning at age 18 and 30 years with 30-year follow-up. Predictive accuracy for ASCVD of the PDAY risk score, calculated at baseline (mean age 24) and at all six CARDIA examinations up until year 15, was examined. We also examined whether the presence of CAC improved model discrimination. The cohort for this study comprised 5004 Black and White men and women, at baseline and 3558 with data at year 15. Each standard deviation increase in PDAY score, at each examination, was significantly associated with future ASCVD. Hazard ratios (per standard deviation) increased from 1.74 to 2.04 from year 0 to year 15. C-statistics ranged from 0.771 to 0.794. Coronary artery calcium measurement at age 33–45 years improved risk prediction only if the score was 0. Cumulative risk exposure over the first 15 years of the CARDIA study also had high-predictive value (c-statistic 0.798, 95% confidence interval 0.762–0.835).
Conclusion
The PDAY risk score may be used in young adults, prior to age 40 years to predict ASCVD events.
Keywords: Cardiovascular epidemiology, Risk factors, Atherosclerosis, Myocardial infarction
Structured Graphical Abstract
Structured Graphical Abstract.
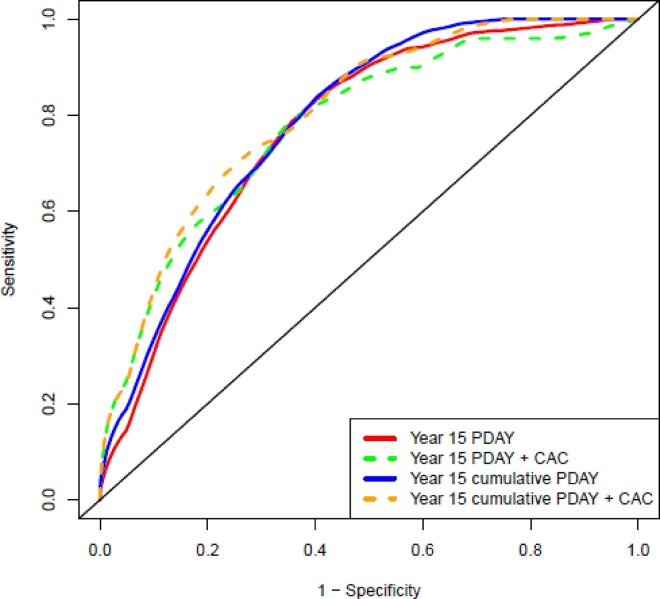
Receiver operating characteristic curves for the prediction of atherosclerotic cardiovascular disease by the PDAY risk score.
See the editorial comment for this article ‘Importance of traditional cardiovascular risk factors for identifying high-risk persons in early adulthood’, by Seamus P. Whelton and Wendy S. Post, https://doi.org/10.1093/eurheartj/ehac148.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) risk factors measured early in life have been linked consistently to atherosclerosis measured post-mortem and markers of subclinical atherosclerosis measured later in life; however, there are less data, linking early-life risk to hard ASCVD events.1–4 There is a growing body of literature demonstrating that early life and sustained exposures to elevated cholesterol and blood pressure levels contribute to ASCVD risk independently of risk exposure later in life.5,6 While ASCVD risk equations have been developed to predict the likelihood of developing ASCVD events among older adults, typically over a 10-year horizon, no validated risk estimating equation exists for those under age 40 years.
The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) risk score was developed from observations of the associations of cardiovascular risk factors, measured post-mortem in individuals aged 15–34 years dying by accident, to atherosclerosis measured in the coronary arteries and abdominal aorta.1,7 The risk equation has been applied to two longitudinal cohorts, the Cardiovascular Risk Development in Young Adults (CARDIA) study and the Cardiovascular Risk in Young Finns Study, and shown to predict the future development of subclinical atherosclerosis, measured either as coronary artery calcium (CAC) or carotid intima-media thickness.4,8,9 A key finding of these studies was that risk measured many years before subclinical atherosclerosis measurement was a better predictor of that measurement than risk measured concurrently. These findings suggested subclinical atherosclerosis measures were, in part, a measure of chronic risk exposure.
The purpose of this study was to determine if the PDAY risk score in young adulthood predicted ASCVD events in the CARDIA cohort. We analysed the predictive ability of the score using risk factors measured up until the age of 40 years on future events to determine the value of risk assessment early in life at a single time point. We also looked separately at the added value of incorporating cumulative risk exposure over young adulthood and also including CAC, measured at 33–45 years of age, to determine if these additional factors improved the discrimination of the PDAY risk score.7
Methods
CARDIA is a longitudinal study of cardiovascular risk, initiated in 1985–86, to understand the evolution of cardiovascular risk beginning in young adulthood.4,8 The cohort includes Black and White men and women recruited at age 18–30 years in Chicago IL, Birmingham AL, Oakland CA, and Minneapolis MN. Recruitment was stratified by race, sex, and educational attainment (more or less/equal to a high school education). Examinations were conducted at years 0, 2, 5, 7, 10 and every 5 years thereafter for over 30 years of follow-up. Coronary artery calcium measurements were performed at year 15 (2000–01). Data used for this study included demographic data and cardiovascular risk factors needed to calculate risk equations, measured at all examinations up until year 15 (at which the mean age was 39 years). Research protocols were approved by local Institutional Review Boards and informed consent was obtained from all participants at each examination. A single coordinating centre at the University of Alabama, Birmingham supervised data collection.
The PDAY score was developed by gating risk factors measured post-mortem to the amount of advanced atherosclerosis (American Heart Association grade IV or higher) found in the coronary arteries and abdominal aorta in men and women dying accidentally.7 Each one-point increase in score is associated with the amount of increase in advanced atherosclerosis in PDAY in 1 year. The score includes eight risk factor components: age with four categories, sex with two categories, non-HDL cholesterol with five categories, HDL cholesterol with three categories, smoking with two categories, blood pressure with two categories, obesity with two categories, and hyperglycaemia with two categories. One point in the score is equivalent to 1 year of vascular aging. Supplementary material online, Table S1 shows the scores assigned to each risk factor. For example, the presence of hypertension, defined as an elevated renal arterial thickness, conveys a score of 4, or 4 years of vascular aging.
Data collection methods for this study have been previously described.4,8 Briefly, demographic data and tobacco use were obtained by questionnaire. Height and weight were measured according to standard procedures and body mass index was calculated. Lipid measurements were obtained in plasma after an overnight fast using standardized procedures at a central laboratory. Non-HDL and LDL cholesterol were calculated. Diabetes status was ascertained at each examination using American Diabetes Association criteria and available data, including fasting serum glucose measurements, medication history, and other data available at selected examinations (e.g. glucose tolerance testing, glycated haemoglobin). Blood pressure was measured three times after a brief (5 min) rest, using a random zero sphygmomanometer, the last two values were averaged. Coronary artery calcium score was measured from two sequential computed tomography scans performed using a standard protocol, with values averaged, using Agatston units.10 Presence of CAC was defined as having a CAC score >0.
Two physician members of the CARDIA Endpoints Surveillance and Adjudication Subcommittee independently adjudicated medical records for each potential event or underlying cause of death (details at http://www.cardia.dopm.uab.edu), with committee review in the case of disagreements. Atherosclerotic cardiovascular disease events were defined as hospitalization for myocardial infarction or acute coronary syndrome with increasing symptoms consistent with ischaemia but without infarction or coronary heart disease (CHD) death or coronary revascularization.11
Data analysis
In order to assess the change in PDAY score with age, a raw PDAY risk score excluding the points for the age component was computed for all CARDIA participants at each exam from year 0 to year 15 (Supplementary material online, Table S1).4,7,8 For each of the six exams, the time of horizon for prediction began with that exam and terminated with year 30. Participants were excluded from an analysis in a given year if they did not attend the examination or were missing data needed for computing the PDAY score. A cumulative PDAY risk score was computed from the repeated PDAY scores from year 0 to year 15 by summing average PDAY scores over time. The average scores were calculated by taking the mean of two consecutive PDAY scores and multiplying by the time interval in years between those two consecutive examinations. The PDAY score at each of the first six exams and the cumulative PDAY score were assessed for association with future CHD events using the Cox proportional hazards model. Hazard ratios (HRs) for each exam were computed for a 1 SD higher PDAY score using the exam-specific standard deviation.
To assess discrimination, the c-statistic was computed for all models and areas under the curves were calculated. Values >0.7 are considered good discrimination and above 0.8 excellent. For each model, the predicted risk for each participant was computed and the set of predicted risks was classified into deciles of risk.12 The mean predicted risk in each decile was determined and plotted against the observed risk for each decile, providing an assessment of calibration. Greenwood-Nam-D’Agostino (GND) χ2 was calculated to examine the calibration of the models. To appraise whether adding the presence of year 15 CAC as a factor to the risk model improved the discrimination, the event and non-event components of the continuous net reclassification index (NRI) were calculated. The event NRI is the net percentage of persons with the event correctly assigned a higher predicted risk [=P(up/event) − P(down/event)]. In a like manner, the non-event NRI is the net percentage of persons without the event correctly assigned a lower predicted risk [=P(down/non-event) − P(up/non-event)].13 Both the event NRI and the non-event NRI can be interpreted as a percentage with a range of 0–100%.14 SAS programmes available at www.crcpress.com/product/isbn/9781439839706 and ncook.bwh.harvard.edu/sas-macros.html were used for analysis. Because the PDAY score does not include race, an interaction with race was tested and was negative; therefore, results are reported for the whole cohort.
Results
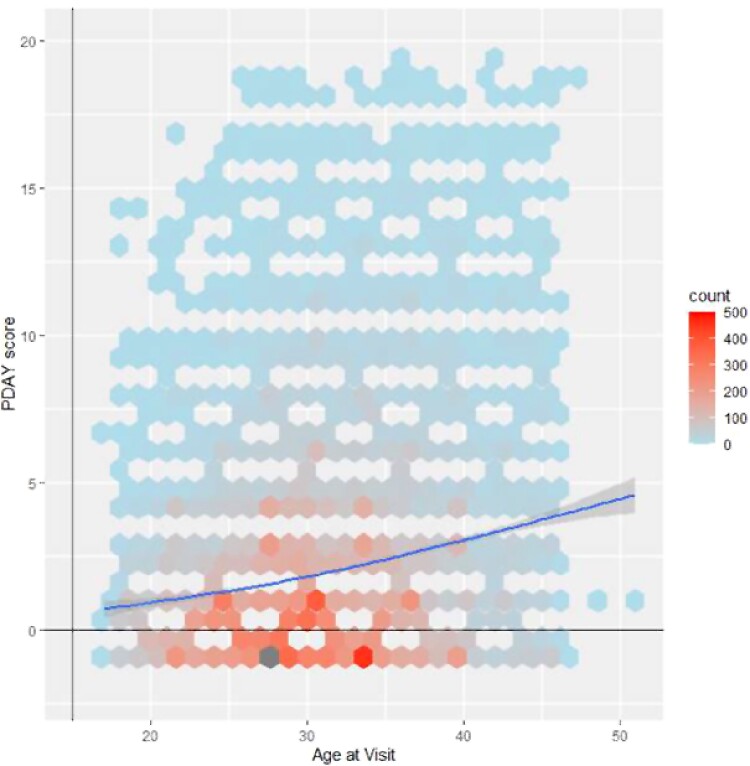
The CARDIA cohort used for this analysis included 5004 Black and White men and women examined at age 18–30 years in 1985–86. Analyses for subsequent examinations included all available participants in whom complete data were present. Table 1 shows risk factor data for the cohort used to calculate the PDAY score with age excluded at baseline and the year 15 exam. Participants who returned for the year 15 exam (n = 3558) had similar demographic and clinical characteristics as the total sample at baseline. Figure 1 shows the raw PDAY score by age to show the increase in score with age and demonstrating an increasing risk factor burden. Among the participants with year 15 exam data, risk factor burden increased over time resulting in an increase of PDAY score of 2 points from baseline to year 15 (Table 1). Raw PDAY risk scores had a wide distribution in young adulthood and variability increased with age.
Table 1.
Risk factor levels used to calculate the PDAY score, by PDAY age group
| Total sample | Participants who returned for year 15 exam | ||
|---|---|---|---|
| Baseline data | Baseline data | Year 15 data | |
| N | 5004 | 3558 | |
| Male sex, n (%) | 2275 (45.5) | 1591 (44.7) | |
| Black, n (%) | 2568 (51.3) | 1671 (47.0) | |
| Non-HDL-C (mg/dL), mean (SD) | 123 (34) | 124 (34) | 134 (38) |
| HDL-C (mg/dL), mean (SD) | 53 (13) | 53 (13) | 51 (15) |
| SBP (mmHg), mean (SD) | 110 (11) | 110 (11) | 113 (15) |
| DBP (mmHg), mean (SD) | 69 (10) | 69 (9) | 75 (12) |
| Hypertension, n (%) | 399 (8.0) | 287 (8.1) | 852 (24.0) |
| DM, n (%) | 33 (0.7) | 19 (0.5) | 180 (5.1) |
| Tobacco use, n (%) | 1522 (30.4) | 963 (27.2) | 785 (22.1) |
| BMI ≥ 30 kg/m2, n (%, males only), mean (SD) | 580 (11.6) | 410 (11.6) | 1213 (34.1) |
| PDAY score, mean (SD) | 1.35 (3.04) | 1.30 (3.04) | 3.34 (4.69) |
SD, standard deviation; PDAY, Pathobiological Determinants of Atherosclerosis in Youth; HDL-C, high-density lipoprotein cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure; DM, diabetes mellitus; BMI, body mass index.
Figure 1.
The relationship of PDAY risk score to age is shown. Frequency of cases is reflected by the colour density. Scores increase over time, however, the range of the score at each age is broad showing the long-term risk exposure for a significant portion of the cohort. As there were several examinations, the data points with overlapping ages, some of the data points are more intense.
In order to examine the association of the PDAY score at each exam year, we show the HRs for a 1 SD higher exam-specific PDAY score related to future ASCVD by age and the c-statistic for the value of the score in event prediction (Table 2). The PDAY risk score is a strong predictor of events at all ages with significant HRs increasing from 1.74 [95% confidence interval (CI) 1.60–1.90] at baseline to 2.04 (95% CI 1.78–2.33) at year 15, although CIs overlapped. For the c-statistic, values vary over time from 0.771 to 0.794, with overlapping CIs at all assessments suggesting a relatively constant ability to predict future events across all examinations. The receiver operating characteristic curves for selected models are shown in Figure 2. The cumulative PDAY score has a similar effect size and c-statistic as those for single examinations. Measures of absolute risk are also included in Table 2.
Table 2.
Hazard ratios and c-statistic with 95% confidence intervals for coronary heart diseasea events predicted by the PDAY scoreb
| Exam | N/events | Unadjusted rate/10 000 person-years by quartiles of PDAY score | Hazard ratio per 1 SD PDAY score (95% CI) | C statistic (95% CI) | |||
|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||||
| Year 0 | 5004/178 | 2 | 4 | 12 | 27 | 1.74 (1.60, 1.90) | 0.775 (0.738, 0.812) |
| Year 2 | 4398/160 | 3 | 6 | 8 | 29 | 1.77 (1.61,1.95) | 0.771 (0.732, 0.811) |
| Year 5 | 4159/153 | 3 | 8 | 14 | 34 | 1.82 (1.64, 2.01) | 0.775 (0.737, 0.813) |
| Year 7 | 3901/137 | 1 | 4 | 14 | 37 | 1.86 (1.68, 2.06) | 0.794 (0.758, 0.829) |
| Year 10 | 3795/145 | 3 | 8 | 19 | 42 | 1.91 (1.71, 2.13) | 0.779 (0.743, 0.815) |
| Year 15 | 3558/122 | 4 | 8 | 18 | 46 | 2.04 (1.78 2.33) | 0.787 (0.747, 0.826) |
| Cumulative PDAY to year 15 | 3478/119 | 3 | 6 | 18 | 49 | 1.96 (1.74, 2.21) | 0.798 (0.762, 0.835) |
| Include year 15 CAC in the models | |||||||
| Year 15c | 2979/97 | 10 | 14 | 28 | 55 | 1.79 (1.53, 2.10) | 0.822 (0.773, 0.871) |
| Cumulative PDAY to year 15c | 2917/94 | 7 | 12 | 27 | 56 | 1.80 (1.55, 2.09) | 0.839 (0.797, 0.881) |
Include: ST-elevation myocardial infarction, non-ST-elevation acute coronary syndrome (previously termed ‘unstable angina’), coronary revascularization during this episode of care, and atherosclerotic coronary heart disease.
Age is excluded from PDAY score but is adjusted for in the prediction model.
Year 15 presence of CAC is added to the model.
CI, confidence interval; PDAY, Pathobiological Determinants of Atherosclerosis in Youth; CAC, coronary artery calcium; SD, standard deviation.
Figure 2.
Receiver operating characteristic curves are shown for four models.
The bottom rows of Table 2 show HRs and c-statistic for the PDAY score after presence of CAC is added to the model. At year 15, in the group of participants without CAC, the median PDAY score was three points lower and cumulative PDAY score was 44 cumulative points lower (P < 0.0001) demonstrating the lower risk factor burden among individuals without CAC by middle age. The addition of CAC to the models already including PDAY score and age did not alter the association with ASCVD events nor improve risk prediction markedly. The HRs overlapped with models without CAC and the c-statistic for the models including CAC were higher by 0.04 from the models not including CAC. For all the results presented in Table 2, adjustment for lipid-lowering use (n = 11 subjects) during the CARDIA study did not impact findings (results not shown).
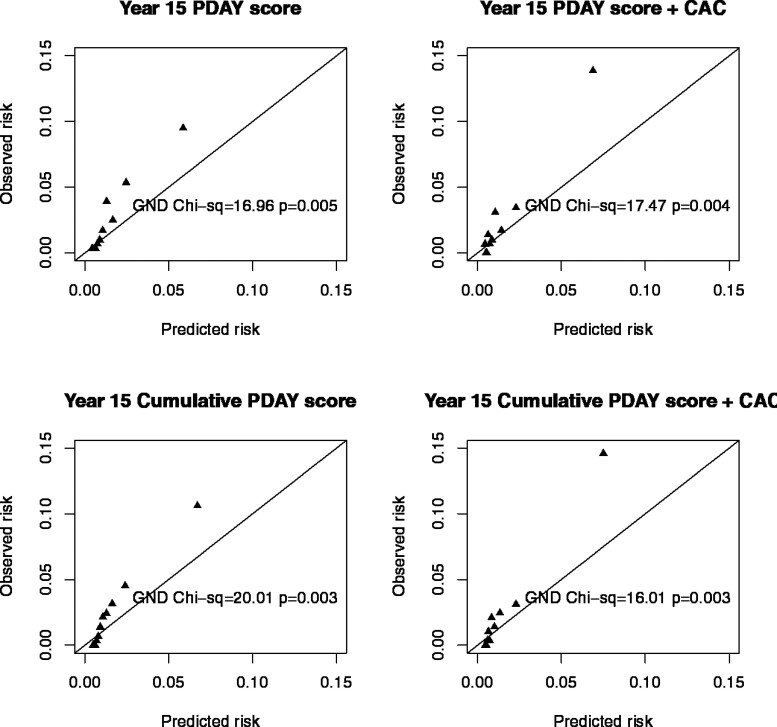
Figure 3 displays an assessment of calibration for each of the four models by comparing the predicted vs. observed risk by deciles of predicted risk. At lower predicted deciles of risk, the model fits reasonably well; however, at the highest deciles of predicted risk, the PDAY score underestimates the observed risk as is highlighted by the significant GND χ2 statistics.
Figure 3.
The relationship between observed and predicted risk is shown for four models. PDAY score underestimates risk in those in the highest deciles of risk.
In order to determine whether the addition of CAC improved the discrimination of the PDAY risk score, we calculated the continuous NRI and compared this to the PDAY risk score without CAC. Table 3 shows the event and non-event components of the continuous NRI for the year 15 PDAY risk score and the cumulative PDAY risk score. Discordant findings were present for those with and without events. With CAC added to the models, the event NRIs were –15.5% and –17.0%, respectively, for the year 15 PDAY score and for the cumulative PDAY score. However, the non-event NRIs were substantial at 59.1% and 69.0%, respectively. Thus, the predicted probability of a future event was lowered for persons without events when CAC, particularly the absence of CAC, was included in the risk model, but, in contrast, it was actually higher for those who went on to have events. When CAC was added as a prediction tool at year 15, there was an improvement in c-statistic from 0.787 to 0.822 (Table 2).
Table 3.
Frequencies for computing continuous net reclassification index for prediction models
| Year 15 PDAY score with vs. without CAC | Cumulative PDAY score to year 15 with vs. without CAC | |||||
|---|---|---|---|---|---|---|
| No. of participants with PM1+ > PM1 | No. of participants with PM1+ < PM1 | Continuous NRI components | No. of participants with PM2+ > PM2 | No. of participants with PM2+ < PM2 | Continuous NRI components | |
| No CHD event | 590 | 2292 | 0.591a | 438 | 2385 | 0.690 |
| CHD event | 41 | 56 | –0.155b | 39 | 55 | –0.170 |
P M1 represents the predicted probability computed from the model consisting of two variables: year 15 age and year 15 PDAY score without the age component.
P M1+ represents the predicted probability computed from the model consisting of three variables: year 15 age, the year 15 PDAY score without the age component, and presence of year 15 CAC.
P M2 represents the predicted probability computed from the model consisting of two variables: year 15 age and cumulative PDAY score to year 15 PDAY score without the age component.
P M2+ represents the predicted probability computed from the model consisting of three variables: year 15 age and cumulative PDAY score to year 15 PDAY score without the age component and presence of year 15 CAC.
Non-event NRI = (2292 − 590)/(2292 + 590) = 0.591.
Event NRI = (41 − 56)/(41 + 56) = –0.155.
PDAY, Pathobiological Determinants of Atherosclerosis in Youth; CAC, coronary artery calcium; CHD, coronary heart disease; NRI, net reclassification index.
Discussion
We have shown, for the first time, that the PDAY score, developed, and applied in young adults, is highly predictive of ASCVD experienced later in life. PDAY scores based on risk factors, measured in the third and fourth decades of life, already identify high-risk individuals likely to go on to have future ASCVD events in later life (Structured Graphical abstract). A single risk factor assessment was almost as accurate as a cumulative score from multiple visits. Based on the continuous non-event NRI, use of a cumulative score, or incorporating CAC measured at age 33–45 years, improved prediction only in those with a CAC score of 0 Agatston units.11 The PDAY score under-estimated risk in those in the highest decile for the score. This underestimation may be secondary to risk exposure prior to the first CARDIA examination that is prior to 18–30 years of age, data not available for this analysis. On the basis of these data, we suggest other longitudinal cohorts consider using this score to predict events in their cohorts to assess validity.
The PDAY risk score was developed to identify risk for advanced atherosclerosis at a young age. A mathematical model was constructed from observed relationships of advanced atherosclerosis in the coronary arteries and abdominal aorta (American Heart Association grade 4 and higher) to cardiovascular risk factors measured post-mortem.1,7 Limitations of the score relate to the fact that blood was collected post-mortem and hypertension diagnosis was based on the measurement of renal arterial muscle thickness so blood pressure could not be assessed as a continuous variable. Thus, the points for lipids were based on non-HDL cholesterol and relationships for this variable may be attenuated.7,15 Neither family history information nor genetic information could be included in the score. Race was not a predictor of atherosclerosis in PDAY. Future studies should look at score refinements such as increasing points for LDL cholesterol as there is error introduced by post-mortem measurement, graded points for levels of blood pressure, and identifying additional variables such as family history and genetic information.
We have previously shown strong relationships between the PDAY risk score and subclinical atherosclerosis in two cohorts, the CARDIA study (for CAC), and the Cardiovascular Risk in Young Finns Study (for carotid intima-media thickness).4,8,9 A consistent finding in both cohorts was that risk measured many years before the subclinical atherosclerosis measurement (15–25 years) was a stronger predictor of subclinical atherosclerosis than risk measured at the time of the atherosclerosis assessment. This finding has been confirmed by assessments of the value of risk measured early in these two studies on later subclinical atherosclerosis outcomes.16–18 The Bogalusa Heart Study has shown that risk factors measured pre-mortem are strongly associated with atherosclerosis assessed after accidental death.2
The Pooled Cohort equation is used for risk stratification in current hypertension and lipid control guidelines, but can only be applied to individuals over 40 years of age.19 In this study, we were unable to compare this equation, applied at age 40 years in the CARDIA cohort, to the PDAY risk score because of the small number of events in those with a calculable Pooled Cohort score. However, the c-statistic from the PDAY score (measured under age 40) is comparable or higher than published results for the Pooled Cohort equation (0.771–0.794 for a single point estimate of the PDAY risk score at a CARDIA examination vs. 0.72 for the Pooled Cohort equation), albeit over a longer time frame than the 10-year risk estimated by the latter equation.
Coronary artery calcium has been shown to add important predictive value and risk reclassification to cardiovascular risk assessment in older adults and those with intermediate risk.20,21 In the CARDIA study, Carr et al.11 have shown that CAC measured at year 15 of the study was highly predictive of future ASCVD and all-cause cardiovascular disease. The CARDIA variables that predicted CAC in that study had significant overlap with the PDAY score, as would be expected.11
In this study, we have shown that much of the predictive ability of CAC relates to its absence. Overall, CAC resulted in an improvement in model discrimination by c-statistic and there was a large reclassification value for those with a low CAC score. The reason for this improvement in classification likely relates to the fact that, in the derivation of the PDAY score, about 40–50% of those with high scores did not have advanced atherosclerosis.7 Those with a low CAC likely belong to a group which, despite the presence of risk factors, develops atherosclerosis more slowly. These findings provide pathophysiologic support for the notion that a CAC score of zero is associated with low likelihood of an ASCVD event, in the next 15 years, as demonstrated in older cohorts.22
In contrast, the presence of significant risk in young adulthood, as reflected in a high PDAY score, suggests a higher likelihood of premature ASCVD than might be at first thought because of a young age. Familial hypercholesterolaemia provides a natural model where lifelong risk exposure leads to premature ASCVD.23 Trajectory analyses, a statistical tool introduced in the late 20th century that allows incorporation of multiple measures over time in longitudinal cohorts, have shown the importance of longitudinal risk factors patterns and cumulative exposure in refining risk prediction. For example, in the CARDIA study, Allen et al.24 showed greater risk for future CAC in individuals, with both higher baseline blood pressure, and a steeper rise in blood pressure trajectory over time. In the International Childhood Cardiovascular Cohort study, children were followed until young adulthood, with carotid intima-media thickness measured as adults. Those with better baseline cardiovascular health and less increase in risk over time had a lower frequency of high carotid intima-media thickness.25 Zhang et al.6 have shown that elevated cholesterol in youth and young adulthood is a predictor of future ASCVD, independent of older adult levels. Two studies have used trajectory analyses incorporating adult lipid data and ASCVD outcomes to show that age 20–40 years may be a vulnerable time for atherosclerosis development.26,27 A Scandinavian study showed that 50% of early ASCVD events (by age 50 years) could be predicted by risk measured 20 years earlier as trajectory of risk related to cholesterol and blood sugar persisted during follow-up.28 These results are consistent with the finding that high ASCVD lifetime risk is a result of lifetime risk factor patterns, many of which emerge at a young age. This study suggests that single measures of risk early in life identify those at high risk for ASCVD and that incorporating risk factor longitudinal measurements adds some refinement of risk prediction.
There is a paucity of ASCVD prevention trials in young adults and thus no high-quality evidence for guidelines for ASCVD prevention beginning at a young age.29 Robinson et al. reviewed the evidence for designing trials to regress atherosclerosis earlier in the life course as the most efficient way to prevent future cardiovascular disease.5,30 Longitudinal studies of adolescents, treated for familial hypercholesterolaemia for over 20 years show dramatic reductions in ASCVD events.23 The best use of the PDAY risk score may be to identify those adolescents and young adults, beyond those with familial hypercholesterolaemia, at highest risk for premature atherosclerosis who could be enrolled in young adult-onset prevention trials.7
Strengths of this study include the excellent phenotyping of the CARDIA cohort, long follow-up with vital data on over 90% of the cohort, and high-quality risk factor data collection. The CARDIA cohort also provides an important external validation to a score developed on measures taken post-mortem. While CARDIA has excellent retention compared with other longitudinal cohorts, missing data for measurements exist, secondary to overall participation rates of about 70–75% of the cohort at any of the individual examinations.
Limitations of the PDAY score include potential underestimation of the impact of blood pressure and lipids on risk due to post-mortem measurement of risk, lack of information on family history, and newer risk tools such as polygenic scores.1,15 Statin use was not highly prevalent at CARDIA year 15 (n = 11) so the impact of early lipid-lowering therapy could not be estimated.
In summary, this study confirms that risk measured early in life is strongly associated with future ASCVD. Given that most ASCVD events occur before age 65 years and that atherosclerosis begins in childhood, there is a strong need to develop prevention strategies beginning early in life.5,29,30 The PDAY score provides a valuable tool to make early-life risk assessment for atherosclerosis likelihood a reality.
Supplementary Material
Contributor Information
Samuel S Gidding, Geisinger Genomic Medicine Institute, Geisinger, Danville, PA, USA; 1631 Hale Hollow Road, Bridgewater Corners, VT, USA.
Laura A Colangelo, Department of Preventive Medicine, Feinberg Medical School, Northwestern University, Chicago, IL, USA.
Chike C Nwabuo, Ronin Institute, Montclair, NJ, USA.
Cora E Lewis, Division of Preventive Medicine, Department of Medicine, University of Alabama at Birmingham, Birmingham, AL, USA.
David R Jacobs, Jr, Division of Epidemiology and Public Health, University of Minnesota, Minneapolis, MN, USA.
Pamela J Schreiner, Division of Epidemiology and Public Health, University of Minnesota, Minneapolis, MN, USA.
Joao A C Lima, School of Medicine, Johns Hopkins University, Baltimore, MD, USA.
Norrina B Allen, Department of Preventive Medicine, Feinberg Medical School, Northwestern University, Chicago, IL, USA.
Funding
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I and HHSN268201800007I), Northwestern University (HHSN268201800003I), University of Minnesota (HHSN268201800006I), and Kaiser Foundation Research Institute (HHSN268201800004I). This manuscript has been reviewed by CARDIA for scientific content.
References
- 1. McGill HC Jr, McMahan CA, Gidding SS. Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study. Circulation 2008;117:1216–1227. [DOI] [PubMed] [Google Scholar]
- 2. Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 1998;338:1650–1656. [DOI] [PubMed] [Google Scholar]
- 3. Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1876–1885. [DOI] [PubMed] [Google Scholar]
- 4. Gidding SS, Rana JS, Prendergast C, McGill H, Carr JJ, Liu K, et al. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) risk score in young adults predicts coronary artery and abdominal aorta calcium in middle age: the CARDIA Study. Circulation 2016;133:139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gidding SS, Robinson J. It is now time to focus on risk before age 40. J Am Coll Cardiol 2019;74:342–345. [DOI] [PubMed] [Google Scholar]
- 6. Zhang Y, Vittinghoff E, Pletcher MJ, Allen NB, Zeki Al Hazzouri A, Yaffe K, et al. Associations of blood pressure and cholesterol levels during young adulthood with later cardiovascular events. J Am Coll Cardiol 2019;74:330–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McMahan CA, Gidding SS, Fayad ZA, Zieske AW, Malcom GT, Tracy RE,et al. Risk scores predict atherosclerotic lesions in young people. Arch Intern Med 2005;165:883–890. [DOI] [PubMed] [Google Scholar]
- 8. Gidding SS, McMahan CA, McGill HC, Colangelo LA, Schreiner PJ, Williams OD,et al. Prediction of coronary artery calcium in young adults using the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) risk score: the CARDIA study. Arch Intern Med 2006;166:2341–2347. [DOI] [PubMed] [Google Scholar]
- 9. McMahan CA, Gidding SS, Viikari JS, Juonala M, Kahonen M, Hutri-Kahonen N, et al. Association of Pathobiologic Determinants of Atherosclerosis in Youth risk score and 15-year change in risk score with carotid artery intima-media thickness in young adults (from the Cardiovascular Risk in Young Finns Study). Am J Cardiol 2007;100:1124–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs JD Jr, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology 2005;234:35–43. [DOI] [PubMed] [Google Scholar]
- 11. Carr JJ, Jacobs JD Jr, Terry JG, Shay CM, Sidney S, Liu K, et al. Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol 2017;2:391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination is survival analysis: model specific population value and confidence interval estimation. Stat Med 2004;23:2109–2123. [DOI] [PubMed] [Google Scholar]
- 13. Pencina MJ, D’Agostino RB Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 2011;30:11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Leening MJ, Vedder MM, Witteman JC, Pencina MJ, Steyerberg EW. Net reclassification improvement: computation, interpretation, and controversies: a literature review and clinician’s guide. Ann Intern Med 2014;160:122–131. [DOI] [PubMed] [Google Scholar]
- 15. McMahan CA, Gidding SS, Malcom GT, Schreiner PJ, Strong JP, Tracy RE, et al. Comparison of coronary heart disease risk factors in autopsied young adults from the PDAY Study with living young adults from the CARDIA study. Cardiovasc Pathol 2007;16:151–158. [DOI] [PubMed] [Google Scholar]
- 16. Pletcher MJ, Bibbins-Domingo K, Lewis CE, Wei GS, Sidney S, Carr JJ, et al. Prehypertension during young adulthood and coronary calcium later in life. Ann Intern Med 2008;149:91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Koskinen JS, Kytö V, Juonala M, Viikari JSA, Nevalainen J, Kähönen M, et al. Childhood risk factors and carotid atherosclerotic plaque in adulthood: the Cardiovascular Risk in Young Finns Study. Atherosclerosis 2020;293:18–25. [DOI] [PubMed] [Google Scholar]
- 18. Loria CM, Liu K, Lewis CE, Hulley SB, Sidney S, Schreiner PJ, et al. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol 2007;49:2013–2020. [DOI] [PubMed] [Google Scholar]
- 19. Muntner P, Colantonio LD, Cushman M, Goff DC Jr, Howard G, Howard VJ, et al. Validation of the atherosclerotic cardiovascular disease Pooled Cohort risk equations. JAMA 2014;311:1406–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lloyd-Jones DM, Braun LT, Ndumele CE, Smith SC Jr, Sperling LS, Virani SS, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology. Circulation 2019;139:e1162–e1177. [DOI] [PubMed] [Google Scholar]
- 21. Lin JS, Evans CV, Johnson E, Redmond N, Coppola EL, Smith N. Nontraditional risk factors in cardiovascular disease risk assessment: updated evidence report and systematic review for the US preventive services task force. JAMA 2018;320:281–297. [DOI] [PubMed] [Google Scholar]
- 22. Blaha MJ, Cainzos-Achirica M, Greenland P, McEvoy JW, Blankstein R, Budoff MJ, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2016;133:849–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Luirink IK, Wiegman A, Kusters DM, Hof MH, Groothoff JW, de Groot E, et al. 20-Year follow-up of statins in children with familial hypercholesterolemia. N Engl J Med 2019;381:1547–1556. [DOI] [PubMed] [Google Scholar]
- 24. Allen NB, Siddique J, Wilkins JT, Shay C, Lewis CE, Goff DC, et al. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA 2014;311:490–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Allen NB, Krefman AE, Labarthe D, Greenland P, Juonala M, Kähönen M, et al. Cardiovascular health trajectories from childhood through middle age and their association with subclinical atherosclerosis. JAMA Cardiol 2020;5:557–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dayimu A, Wang C, Li J, Fan B, Ji X, Zhang T, et al. Trajectories of lipids profile and incident cardiovascular disease risk: a longitudinal cohort study. J Am Heart Assoc 2019;8:e013479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pencina KM, Thanassoulis G, Wilkins JT, Vasan RS, Navar AM, Peterson ED, et al. Trajectories of non-HDL cholesterol across midlife: implications for cardiovascular prevention. J Am Coll Cardiol 2019;74:70–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ivert T, Malmström H, Hammar N, Carlsson AC, Wändell PE, Holzmann MJ, et al. Cardiovascular events in patients under age fifty with early findings of elevated lipid and glucose levels—the AMORIS study. PLoS One 2018;13:e0201972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gooding HC, Gidding SS, Moran AE, Redmond N, Allen NB, Bacha F, et al. Challenges and opportunities for the prevention and treatment of cardiovascular disease among young adults: report from a National Heart, Lung, and Blood Institute Working Group. J Am Heart Assoc 2020;9:e016115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Robinson JG, Williams KJ, Gidding S, Boren J, Tabas I, Fisher EA, et al. Eradicating the burden of atherosclerotic cardiovascular disease by lowering apolipoprotein B lipoproteins earlier in life. J Am Heart Assoc 2018;7:e009778. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.