Abstract
The fragment of inferior alveolar nerve (IAN) existing anterior to the mental foramen (MF), before dividing the canal, is known as the “Anterior Loop of the IAN”. The presence of anterior loop (AL) is important when placing the implant in inter foraminal area of the mandible or during any other surgical procedure. It is imperative to precisely determine the position and dimensions of these anatomical variations on a cone-beam CT (CBCT) scan. To estimate the prevalence and pattern of anterior loop of IAN and establish any corelation between dimension of the MF with length and angulation of the AL of the IAN. Total 178 CBCT samples were collected fulfilling the inclusion criteria from a private diagnostic centre in Bhubaneswar, Odisha. The greatest diameter of the mental foramen was measured along with anterior loop length and angulation in the panoramic section of the CBCT scan. The angulation formed and the length was corelated with the greatest diameter of the mental foramen and analysed. Our study reveals that the AL was more frequently seen among males, predominantly on the left side of the mandible. The relationship between length of the anterior loop and diameter of the mental foramen demonstrated a mild negative corelation. There was no possible corelation present between angle formed by anterior loop with inferior alveolar canal and diameter of mental foramen. A small positive corelation was established between length of anterior loop and angle formed by the anterior loop with inferior alveolar canal. CBCT scans should be recommended for pre-surgical evaluation of anatomical variations in the mandibular region. Also, a safe margin of 3–4 mm anterior to mental foramen should be maintained while working in the premolar area.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-021-02691-w.
Keywords: Anterior Loop, Cone Beam Computed Tomography, Inferior alveolar nerve, Mental Foramen
Introduction
Cone Beam Computed Tomography (CBCT) also known as “C-Arm Computed Tomography, Cone Bean Volume Computed Tomography or Flat Panel Computed Tomography” is the most recent advancement in the field of diagnostic imaging in dentistry. It helps in acquiring data volumetrically and provides 3D radiographic images for assessment of dental and maxillofacial complex facilitating appropriate diagnosis and treatment. In human anatomy, the head and neck region have the most complex anatomical structures. [1] Accurate location and dimensions of anatomical landmarks should essentially be considered during surgical interventions. The mandibular canal/inferior alveolar nerve (IAN) canal is a significant mandibular anatomical structure and harbours the clinically distinctive neurovascular bundles. [2] The mandibular nerve gains entry in the mandible through the mandibular foramen located on the medial aspect of the mandibular ramus, and after its passage through the mandibular foramen, it is referred to as inferior alveolar nerve (IAN). [3] The terminating fragment of the IAN may occasionally pass below the inferior border and the anterior wall of the mental foramen (MF). After giving forth the minor mandibular incisive branch, the main branch arc back to re-enter the foramen and emanate to the soft tissues as the mental nerve. In mandibular canal, the Inferior alveolar nerve (IAN) travels “forward, outward, upward and backward” to emerge at the mental foramen (MF) and forms the anterior loop (AL). [4]
Bavitz and Misch precisely elucidated the anterior loop as “The structure where the mental neurovascular bundle crosses inferior and anterior to the mental foramen then doubles or loops back to depart the mental foramen” [5, 6]. Published literature has reported range of disparities related with the AL. Solar et al., characterized AL into three dissimilar types: Type I, Type II, and Type III. In Type I, the AL is indistinct, with a Y-shaped anatomy. The mental branch exists the IAN posterior to the opening of the mental foramen. In Type II, the AL is absent, with a T-shaped anatomy. The incisive branch runs perpendicular to the main nerve trunk, and the mental branch passes into the mental foramen in a perpendicular pattern. In Type III, the AL is distinct, and the anatomy is Y-shaped. [7] (Fig. 1).
Fig. 1.
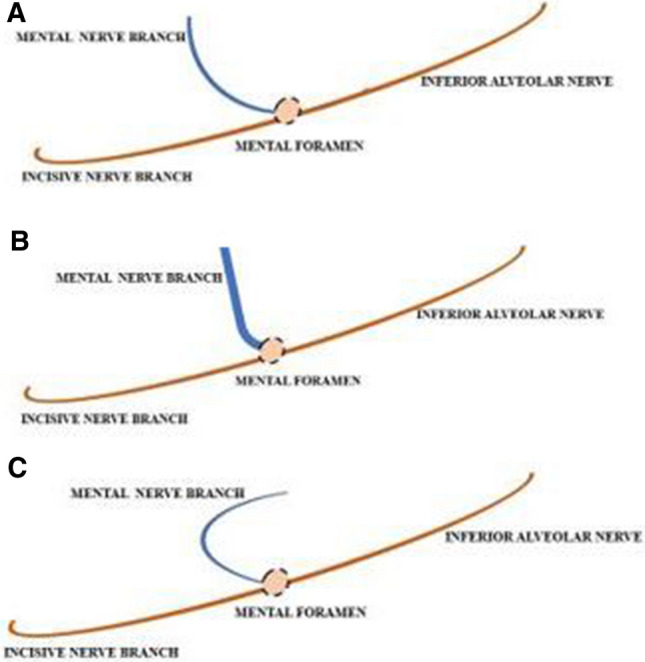
Schematic representation of the types of Anterior loop of Inferior alveolar nerve (IAN)
Any surgical intervention (principally dental implants) warrants a scrupulous and detailed delineation of AL, not only to avert the potential iatrogenic complications, but also to augment the surgical outcomes. [8] Despite the proposed recommendations to intercept the complications, (such as a 5 mm safe distance to the most distal fixture from the AL and a 5 mm distance from the MF), the precise identification of the AL is still imperative, as this distance might exhibit variation in different individuals and ethnic groups. [9]
Clinical determination of the AL (probing) fails to distinguish between the anterior loop and the incisive canal. [9, 10] Accurate determination of the AL is also not achievable with two-dimensional radiographic procedures. [11–13] 3-dimensional radiographic procedures, such as cone-beam computed tomography (CBCT) provide excellent delineation of the anterior loop. However, due to the high cost and radiation exposure by CBCT, many skilled surgeons still prefers panoramic radiographs for mandibular implant placements. [14–17] Although panoramic radiographs may accurately demonstrate the mental foramen, [17] it fails to identify the anterior loop as precisely as the CBCT. [9, 11–13, 15]
Tomographic procedures help to elucidate a detailed overview of the dimensions of the mandibular interforaminal areas. Additionally, a 3-dimensional precision, the optimal image quality, the excellent geometric accuracy, reduced radiation doses as compared to CT, along with easy manoeuvre enables cone-beam computed tomography (CBCT) as an excellent approach for mandibular anterior region implant insertions. [18]
Published studies have provided debatable observations in terms of AL length and even its existence. [9, 15, 19–21] Hence, it is imperative to assess the prevalence of AL and demarcate a precise, safe distance from the mental foramen for mandibular implant procedures.
With this background, a CBCT based retrospective study was conducted to evaluate the Prevalence, Patterns and Variations of Anterior Loop of Inferior Alveolar Nerve in a South Indian population.
Material and Methods
A retrospective study was carried out for a period of six months (August to February) in the Outpatient Department of Oral Medicine and Radiology, Institute of Dental Sciences, Siksha ‘O’ Anusandhan University, Orissa, where a total 178 Mandibular CBCT scans taken from a private diagnostic centre in Bhubaneswar, Odisha for various clinical indications such as implant placement, were evaluated for the measurements of the anterior loop of IAN. The study was conducted after obtaining ethical approval from the Institutional Ethics Committee (IEC), Institute of Medical Sciences and SUM Hospital DRI/IMS.SU/SOA 18/26/2020 [Appendix 1]. Written consent from the patients was obtained prior so that their scans could also be utilised for research purposes. CBCT scans were performed with Orthophos SL at resolution of 80 micron (Dentsply Sirona) with the following exposure parameters- 85 kv, 10 mA and 14.2 s. Software used to interpretation and measurement of the variables in a CBCT scan was 3D Diagnostics, Galileos Viewer.
Proper diagnostic quality Mandibular CBCT scans with complete patient files and records, patients of both genders in the age range of 20–70 years, patients with a negative history of trauma to mandible, previous orthognathic surgery or operated cyst and tumour, and patients without any systemic disease affecting growth and development were included in the study. However, CBCT scans with less diagnostic quality and artefacts, mixed dentition CBCT scans, scans showing any supernumerary or impacted tooth in the premolar area, and patients with developmental anomalies were considered in the exclusion criteria.
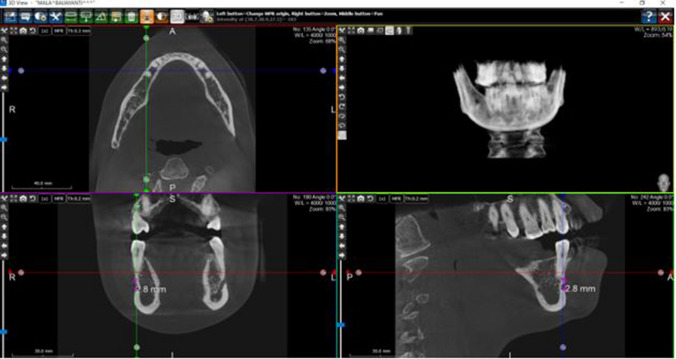
The greatest diameter of the MF was measured in the coronal and sagittal section by the length measuring tool of the software. Anterior loop was traced in the panoramic section in the CBCT scan. The length of the AL was measured from the most anterior part of the nerve till the distal part of the mental foramen. The angle formed by the AL with the inferior alveolar canal was assessed and measured. CBCT scans were analysed and the measurements were recorded in the master table for the statistical analysis. (Fig. 2).
Fig. 2.
Showing coronal, sagittal, and axial window with measured greatest diameter of the mental foramen
Distribution of different patterns of AL, diameter of MF and dimensions of the AL were reported as mean and standard deviation. The categorical variables under the study were reported as frequency (%). Prevalence of presence of AL among the population was reported as percentage with 95% confidence interval. Pearson’s correlation was run to assess the relationship between length of AL and diameter of MF, angle formed by the AL with IAN canal and diameter of MF, length of AL and angle formed by the anterior loop with inferior alveolar canal in 53 patients where presence of anterior loop was seen. General guidelines provided by Cohen [22] were used to interpret the strength of associations. The output of the correlation was presented as correlation coefficient (r) and level of significance (p-value). The significance level was set at p-value = 0.05. Statistical analysis was performed using STATA 15.1 software”.
Results
The mean age of the population was found to be 47 years and around 59% of the participants were males and 41% were females. Our results showed 3 patterns of AL among all the participants. In 106 participants, no AL was seen in the CBCT images. AL was seen among 53 patients and 19 participants showed nerve forming right angle with the IAC. The average diameter of the MF assessed is around 3.45 mm ± 0.92. (Fig. 3 and Table 1).
Fig. 3.
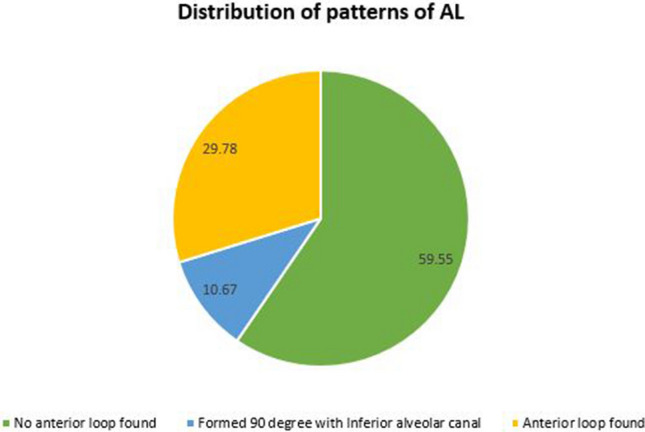
Shows the distribution of anterior loop among the study population
Table 1.
Descriptive characteristics of the population
| Participant’s Characteristics (N = 178) | Mean ± SD / n (%) |
|---|---|
| Age (In years) | 47.3 ± 15.6 |
| Gender | |
| Male | 105 (58.99) |
| Female | 73 (41.01) |
| Pattern | |
| TYPE I -No anterior loop found | 106 (59.55) |
| TYPE II- Formed 90 degree with Inferior alveolar canal | 19 (10.67) |
| TYPE III—Anterior loop found | 53 (29.78) |
| Diameter of mental foramen (In mm) | 3.45 ± 0.92 |
N Total population; SD Standard deviation; n (%) Frequency (%))
Among all the participants, nearly 30% of the population presented the presence of AL. The prevalence of presence of AL in the study population was found to be 30% with 95% confidence interval of 23–37%.
Out of the 53 participants with presence of AL, 64.15% were males, the mean age of this group was found to be 47.9 ± 16.91 years and majority of ALs were found to be present on the left side. The average length of the AL was reported to be 2.04 ± 0.47 cm and the average angulation formed by the AL with the IAN canal was reported as 32.69 ± 9.83 degrees. (Table 2).
Table 2.
Descriptive characteristics of the population (With presence of anterior loop)
| Participant’s characteristics (With presence of anterior loop) | Mean ± SD / n (%) |
|---|---|
| Age (In years) | 47.9 ± 16.91 |
| Gender | |
| Male | 34 (64.15) |
| Female | 19 (35.85) |
| Presence side | |
| Right | 17 (32.08) |
| Left | 21 (39.62) |
| Both | 15 (28.30) |
| Diameter of mental foramen (In mm) | 3.55 ± 0.88 |
| Length of anterior loop (In cm) | 2.04 ± 0.47 |
| Angle formed by anterior loop with Inferior alveolar canal (In degree) | 32.69 ± 9.83 |
N Total population; SD Standard deviation; n (%) Frequency (%)
Although a small negative correlation (r = 0.1007) between length of AL and diameter of MF and a small positive correlation (r = 0.1714) between length of AL and angle formed by the AL with IAN canal was found on Pearson’s correlation test, none of them were statistically significant. No correlation was found between the angle formed by the anterior loop with IANC and diameter of MF. (Table 3).
Table 3.
Pearson’s correlation exploring relationships between dimensions
| Parameters N = 53 | Correlation coefficient (|r|) | Level of statistical significance (p-value) |
|---|---|---|
| Length of AL and diameter of MF | 0.1007 | 0.4733 |
| Angle formed by AL with inferior alveolar canal and diameter of mental foramen | 0.0686 | 0.6253 |
| Length of anterior loop and angle formed by AL with inferior alveolar canal | 0.1714 | 0.2198 |
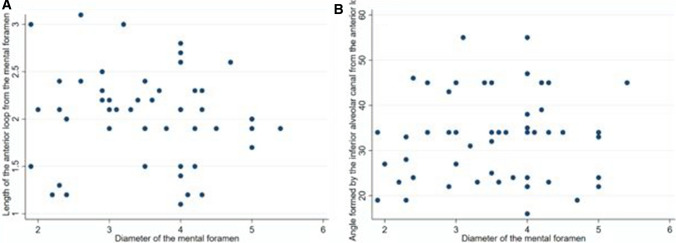
Figure 4a and b shows the scatter plot eliciting the relationship between the diameter of MF across the length of the AL and the relationship of the MF across the length of the AL. It presents no linear corelation between the variable under comparison, which also aligns with our finding from Pearson’s corelation coefficients
Fig. 4.
a Shows corelation between Diameter of MF across changing length of AL. 4b shows corelation of diameter of MF across different angle formed by AL with IAN canal
Discussion
The comprehensive understanding of anatomical structures of inter-foraminal region and its variations is imperative to avert damage to the neurovascular bundles. Anterior loop (AL) of the mandibular canal is an important anatomic variation in the inter-foraminal area. [21] AL injury has been reported as a cause for pain, altered sensations, and haemorrhagic events post implant placement in these regions. [18, 23]
Several studies have aimed to ascertain the length of the AL of the IAN employing various approaches (anatomical, radiographical and combined). [10, 24, 25] Several studies to demonstrate the AL on panoramic radiographs have yielded inconsistent results, primarily due to the cervical vertebrae superimposition and the orientation of the X-ray beam in relation to the trajectory of the canals. Whereas, there are a smaller number of studies to determine this parameter on the CT scan and further less on CBCT. [26, 27] Thus, it is essential to perform a thorough pre-surgical assessment of IAN trajectory, frequency and extension of the IAN loop, and position of the mental foramen.
In the present study, the mean age of the population was 47.3 ± 15.6 years. Males and females attributed to 59% & 41% of the study population respectively. Similar findings were observed in the studies conducted by Do Nascimanto et al., [14] and Torres et al., [28] where the mean age of the study population was 51.4 ± 15.3 & 48.57 years respectively. However, contrasting findings were reported regarding the gender distribution in other studies. [4, 9, 14, 29–32]
Mental Foramen
One of the most common complications during mandibular surgical procedures is the mental nerve injury at the time of flap release. Mental foramen exhibits variation in the dimensions and position in different individuals and ethnic groups. Hence, it is essential to demonstrate the precise position and dimensions of MF and AL prior to various surgical procedures.
According to the studies by Panjnoush et al. [32], Mahalawy et al., [33] Alfaleh et al., [34] and Shalash et al., [35] the most common location of mental foramen was along the second premolar. Mental foramen located between the first and second premolars were observed in the other studies. [28, 31, 36–38] According to a study by Von Arx et al., [38] the mean size of the MF showed a height of 3.0 mm and a length of 3.2 mm. The mean size of MF (in the sagittal sections) was found to be 3.36 mm in height and 2.54 mm in length in a study by Chappidi et al. Most of the mental foramen were oval (69.2%) followed by round shape. [39]
In our study, most common location of mental foramen was along the second premolar region, oval shaped, with the mean dimension as 3.45 ± 0.92 mm.
Anterior Loop
Before performing any surgical procedure in the proximity of the mental foramen, not only its location is important, but also the trajectory of the mental nerve as it emerges from the mandibular bone.
The prevalence of anterior loop of mental nerve exhibits a wide variation, ranging from 0%, [40] to as high as 88%, [31] and 100%. [26]
In our study, the prevalence of AL was reported to be 30% with 95% confidence interval. This was in close coherence to the study findings of Ngeow et al. (34%), [13] Oliveira-Santos et al. (22–28%), [30] Smriti et al. (27.8%), [37] Sahman et al. (28.5%), [41] and Kheir et al. (32.8%) [42]. Our study findings were in contrast to the study findings by Apostolakis et al. (48%) [9], Do Nascimento et al. (41.6), [14] Parnia et al. (84.4%), [18] Torres et al. (58.8%), [28] Mahalawy et al. (15.2%), [33] Shalash et al. (55%), [35] and Zeba et al. (37.3%). [43]
In our study, the mean age of subjects with anterior loop was found to be 47.6 ± 16.91 years which is in pact with the study conducted by Smriti et al. [37] Studies by Do Nascimento et al., [14] Lu CI et al., [20] and Abhijeet et al. [39] found that the anterior loop was mostly frequently encountered in younger age group. However, a decreasing frequency of the AL with increasing age was reported by Ngeow et al., [13] Torres et al., [28] and Kastala et al. [45] Decreased corticalization quality of the bone and slower remodelling may be the most common attributes to a decrease in the prevalence of AL with increasing age.
The present study revealed that most of the AL were seen on the left side (39.62%), followed by right side (32.08%), and bilateral AL (28.30%). This was in coherence to the study findings by Zeba et al. (52.7%) [43] However, bilateral AL were reported in the studies by Apostolakis et al. (57%) [9], Do Nascimento et al. (54%), [14] Panjnoush et al. (39%), [32] and Sahman et al. (54%). [41] A higher prevalence of AL on the right side were documented in the studies by Torres et al. (60.23%), [28] and Smriti et al. (37.11%). [37]
In the present study, the occurrence of AL was seen more common in males (64.15%). A higher prevalence of AL among males was also reported by other studies. [13, 14, 29, 32, 37, 41]
The average range of AL length exhibits a wide variation, ranging between 0.4 to 6 mm, with maximum lengths up to 9 or even 11 mm. [9, 14, 15, 19, 20, 25, 31, 41] The average length of the AL recorded in our study was 2.04 ± 0.47 mm. Our study findings were in coherence with the other study findings. [15, 37, 41, 46]
Our study demonstrated that Type I AL was the commonest (59.55%), followed by Type III (29.78) and Type II (10.67%). However, our findings contrasted with the other study findings. [47, 48]
The average angulation of the AL established in the present study is 32.69 ± 9.83 degree. However, to the best of our knowledge, there is no similar study conducted to support the concluded data about the average angulation.
There was no specific corelation found between the diameter of the mental foramen with variable length and angulation of the AL.
Limitation of the Study
Age and sex ratio found in the study corresponds merely to the sample population. Hence, it cannot be generalized that the presence of anterior loop of IAN has an age/gender predilection. A hospital or clinic-based study is not sufficient to conclude about these demographic parameters. Therefore, population-based studies with a larger sample size will be required for this.
Conclusion
CBCT should be recommended by all clinicians while diagnosis, treatment planning and assessment of AL while implant planning, fracture reduction, and any other operative procedures in the mandibular region. It is advisable to maintain a safe margin of 3–4 mm anterior to mental foramen while working in the premolar area.
Supplementary Information
Below is the link to the electronic supplementary material.
Declaration
Conflicts of interest
The author declares that they have no conflict of interest.
Human Participants and/or Animals
The patient and the attendants were informed about the nature of disease and treatment protocol.
Informed Consent
The patients were informed about the nature of disease and treatment protocol. Written informed consent was taken from patient.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Suvranita Jena, Email: suvranitajena9@gmail.com.
Rajat Panigrahi, Email: drrajat@gmail.com.
Abhishek Ranjan Pati, Email: patiabhi@gmail.com.
Shamimul Hasan, Email: shasan1@jmi.ac.in.
References
- 1.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dento Maxillo Facial Radiol. 1999;28(4):245–248. doi: 10.1038/sj/dmfr/4600448. [DOI] [PubMed] [Google Scholar]
- 2.Shaban B, Khajavi A, Khaki N, Mohiti Y, Mehri T, Kermani H. Assessment of the anterior loop of the inferior alveolar nerve via cone-beam computed tomography. J Korean Assoc Oral Maxillofac Surg. 2017;43(6):395–400. doi: 10.5125/jkaoms.2017.43.6.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Makris N, Stamatakis H, Syriopoulos K, Tsiklakis K, Van der Stelt PF. Evaluation of the visibility and the course of the mandibular incisive canal and the lingual foramen using cone-beam computed tomography. Clin Oral Implants Res. 2010;21(7):766–771. doi: 10.1111/j.1600-0501.2009.01903.x. [DOI] [PubMed] [Google Scholar]
- 4.Kaya Y, Sencimen M, Sahin S, Okcu KM, Dogan N, Bahcecitapar M. Retrospective radiographic evaluation of the anterior loop of the mental nerve: comparison between panoramic radiography and spiral computerized tomography. Int J Oral Maxillofac Implants. 2008;23:919–925. [PubMed] [Google Scholar]
- 5.Bavitz JB, Harn SD, Hansen CA, Lang M. An anatomical study of mental neurovascular bundle - implant relationship. Int J Oral Maxillofac Implants. 1993;8:563–567. [PubMed] [Google Scholar]
- 6.Misch CE. Root form surgery in the edentulous mandible: Stage I implant insertion. In: Misch CE, editor. Implant Dentistry. 2. St. Louis: The CV Mosby Company; 1999. pp. 347–370. [Google Scholar]
- 7.Solar P, Ulm C, Frey G, Matejka M. A classification of the intraosseous paths of the mental nerve. Int J Oral Maxillofac Implant. 1994;9:339–344. [Google Scholar]
- 8.Roshene R, Jayanth KV. Radiological study on the anterior loop of inferior alveolar nerve. Indian J Public Health Res Develop. 2019;10(11):595–599. [Google Scholar]
- 9.Apostolakis D, Brown JE. The anterior loop of the inferior alveolar nerve: Prevalence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implants Res. 2012;23:1022–1030. doi: 10.1111/j.1600-0501.2011.02261.x. [DOI] [PubMed] [Google Scholar]
- 10.Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol. 2006;77:1933–1943. doi: 10.1902/jop.2006.060197. [DOI] [PubMed] [Google Scholar]
- 11.Mraiwa N, Jacobs R, Moerman P, Lambrichts I, van Steenberghe D, Quirynen M. Presence and course of the incisive canal in the human mandibular interforaminal region: two-dimensional imaging versus anatomical observations. Surg Radiol Anat. 2003;25:416–423. doi: 10.1007/s00276-003-0152-8. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs R, Mraiwa N, Van Steenberghe D, Sanderink G, Quirynen M. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat. 2004;26:329–333. doi: 10.1007/s00276-004-0242-2. [DOI] [PubMed] [Google Scholar]
- 13.Ngeow WC, Dionysius DD, Ishak H, Nambiar P. A radiographic study on the visualization of the anterior loop in dentate subjects of different age groups. J Oral Sci. 2009;51:231–237. doi: 10.2334/josnusd.51.231. [DOI] [PubMed] [Google Scholar]
- 14.do Nascimento EHL, dos AnjosPontual ML, dos AnjosPontual A, da Cruz Perez DE, Figueiroa JN, Marco Antônio Gomes-Frazao MA, , et al. Assessment of the anterior loop of the mandibular canal: a study using cone-beam computed tomography. Imaging Sci Dent. 2016;46:69–75. doi: 10.5624/isd.2016.46.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vujanovic-Eskenazi A, Valero-James J-M, Sanchez-Garces M-A, Gay- EC. A retrospective radiographic evaluation of the anterior loop of the mental nerve: comparison between panoramic radiography and cone beam computerized tomography. Medicina Oral, Patologıa Oral y Cirugıa Bucal. 2015;20:239–245. doi: 10.4317/medoral.20026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zitzmann NU, Margolin MD, Filippi A, Weiger R, Krastl G. Patient assessment and diagnosis in implant treatment. Aust Dent J. 2008;53(1):3–10. doi: 10.1111/j.1834-7819.2008.00036.x. [DOI] [PubMed] [Google Scholar]
- 17.Vazquez L, Saulacic N, Belser U, Bernard JP. Efficacy of panoramic radiographs in the preoperative planning of posterior mandibular implants: a prospective clinical study of 1527 consecutively treated patients. Clin Oral Implants Res. 2008;19:81–85. doi: 10.1111/j.1600-0501.2007.01402.x. [DOI] [PubMed] [Google Scholar]
- 18.Parnia F, Moslehifard E, Hafezeqoran A, Mahboub F, Mojaver-Kahnamoui H. Characteristics of anatomical landmarks in the mandibular interforaminal region: a cone-beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2012;17(3):420–425. doi: 10.4317/medoral.17520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen Z, Chen D, Tang L, Wang F. Relationship between the position of the mental foramen and the anterior loop of the inferior alveolar nerve as determined by cone beam computed tomography combined with mimics. J Comput Assist Tomogr. 2015;39:86–93. doi: 10.1097/RCT.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 20.Lu CI, Won J, Al-Ardah A, Santana R, Rice D, Lozada J. Assessment of the anterior loop of the mental nerve using cone beam computerized tomography scan. J Oral Implantol. 2015;41:632–639. doi: 10.1563/aaid-joi-D-13-00346. [DOI] [PubMed] [Google Scholar]
- 21.Rosenquist B. Is there an anterior loop of the inferior alveolar nerve? Int J Periodontics Restorative Dent. 1996;16:40–45. [PubMed] [Google Scholar]
- 22.Cohen J. Set correlation and contingency tables. Appl Psychol Meas. 1988;12(4):425–434. [Google Scholar]
- 23.Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol. 2004;75(5):631–645. doi: 10.1902/jop.2004.75.5.631. [DOI] [PubMed] [Google Scholar]
- 24.Uchida Y, Yamashita Y, Goto M, Hanihara T. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region. J Oral Maxillofac Surg. 2007;65:1772–1779. doi: 10.1016/j.joms.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 25.Uchida Y, Noguchi N, Goto M, Yamashita Y, Hanihara T, Takamori H, Sato I, Kawai T, Yosue T. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: a second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67:744–750. doi: 10.1016/j.joms.2008.05.352. [DOI] [PubMed] [Google Scholar]
- 26.Arzouman MJ, Otis L, Kipnis V, Levine D. Observations of the anterior loop of the inferior alveolar canal. Int J Oral Maxillofac Implants. 1993;8(3):295–300. [PubMed] [Google Scholar]
- 27.Yonchak T, Reader A, Beck M, Meyers WJ. Anaesthetic efficacy of unilateral and bilateral inferior alveolar nerve blocks to determine cross innervation in anterior teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(2):132–135. doi: 10.1067/moe.2001.115720. [DOI] [PubMed] [Google Scholar]
- 28.Velasco-Torres M, Padial-Molina M, Avila-Ortiz G, García-Delgado R, Catena A, Galindo-Moreno P. Inferior alveolar nerve trajectory, mental foramen location and incidence of mental nerve anterior loop. Med Oral Patol Oral Cir Bucal. 2017;22(5):630–635. doi: 10.4317/medoral.21905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosa MB, Sotto-Maior BS, Machado Vde C, Francischone CE. Retrospective study of the anterior loop of the inferior alveolar nerve and the incisive canal using cone beam computed tomography. Int J Oral Maxillofac Implants. 2003;28:388–392. doi: 10.11607/jomi.2648. [DOI] [PubMed] [Google Scholar]
- 30.de Oliveira-Santos C, Souza PH, de Azambuja B-C, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16(2):387–393. doi: 10.1007/s00784-011-0544-9. [DOI] [PubMed] [Google Scholar]
- 31.Neiva RF, Gapski R, Wang HL. Morphometric analysis of implant-related anatomy in Caucasian skulls. J Periodontol. 2004;75(8):1061–1067. doi: 10.1902/jop.2004.75.8.1061. [DOI] [PubMed] [Google Scholar]
- 32.Panjnoush M, Rabiee ZS, Kheirandish Y. Assessment of location and anatomical characteristics of mental foramen, anterior loop and mandibular incisive canal using cone beam computed tomography. J Dent (Tehran) 2016;13(2):126–132. [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Mahalawy H, Al-Aithan H, Al-Kari B, Al-Jandan B, Shujaat S. Determination of the position of mental foramen and frequency of anterior loop in Saudi population. A retrospective CBCT study. Saudi Dent J. 2017;29(1):29–35. doi: 10.1016/j.sdentj.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alfaleh WM. Location of the mental foramen using volumetrically rendered CBCT images. J Pak Dent Assoc. 2020;29(1):19–23. [Google Scholar]
- 35.Shalash M, Khallaf ME, Ali AR. Position and dimensions of the mental foramen and presence of the anterior loop in the Egyptian population: a retrospective CBCT study. Bull Natl Res Cent. 2020;44(1):110. doi: 10.1186/s42269-020-00364-2. [DOI] [Google Scholar]
- 36.Khojastepour L, Mirbeigi S, Mirhadi S, Safaee A. Location of mental foramen in a selected iranian population: A CBCT assessment. Iran Endod J. 2015;10(2):117–121. [PMC free article] [PubMed] [Google Scholar]
- 37.Sinha S, Kandula S, Sangamesh NC, Rout P, Mishra S, Bajoria AA. Assessment of the anterior loop of the mandibular canal using cone-beam computed tomography in Eastern India: a record-based study. J Int Soc Prev Community Dent. 2019;9(3):290–295. doi: 10.4103/jispcd.JISPCD_83_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Von Arx T, Friedli M, Sendi P, Lozanoff S, Bornstein MM. Location and dimensions of the mental foramen: a radiographic analysis by using cone-beam computed tomography. J Endod. 2013;39(12):1522–1528. doi: 10.1016/j.joen.2013.07.033. [DOI] [PubMed] [Google Scholar]
- 39.Chappidi V, Swapna LA, Dheeraj V, Nikitha GR, Kanakagiri M. Evaluation of morphometric variations in mental foramen and prevalence of anterior loop in South Indian population – A CBCT study. J Indian Acad Oral Med Radiol. 2019;31:134–139. [Google Scholar]
- 40.Kieser J, Kuzmanovic D, Payne A, Dennison J, Herbison P. Patterns of emergence of the human mental nerve. Arch Oral Biol. 2002;47:743–747. doi: 10.1016/s0003-9969(02)00067-5. [DOI] [PubMed] [Google Scholar]
- 41.Sahman H, Sisman Y. Anterior loop of the inferior alveolar canal: a cone-beam computerized tomography study of 494 cases. J Oral Implantol. 2016;42(4):333–336. doi: 10.1563/aaid-joi-D-15-00038. [DOI] [PubMed] [Google Scholar]
- 42.Kheir MK, Sheikhi M. Assessment of the anterior loop of mental nerve in an Iranian population using cone beam computed tomography scan. Dent Res J. 2017;14:418–422. doi: 10.4103/1735-3327.218566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siddiqui Z, Rai S, Ranjan V. Efficacy and evaluation of cone beam computed tomography in determining the prevalence and length of anterior loop of inferior alveolar nerve in North Indian population. J Indian Acad Oral Med Radiol. 2018;30:32–37. [Google Scholar]
- 44.Alok A, Singh S, Bhattacharya PT, Kishore M, Piyush K, Shukla AK. A radiographic study on the visualization of the anterior loop in Darbhanga population. Int J Contemp Med Res. 2019;6(5):11–14. [Google Scholar]
- 45.Kastala RK, David CM, Jayapal N. Momentousness of the mental loop: a comparative study. Contemp Clin Dent. 2017;10:86–92. doi: 10.4103/ccd.ccd_391_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Moghddam MR, Davoudmanesh Z, Azizi N, Rakhshan V, Shariati M. Prevalence and length of the anterior loop of the inferior alveolar nerve in Iranians. J Oral Implantol. 2017;43(5):333–336. doi: 10.1563/aaid-joi-D-16-00212. [DOI] [PubMed] [Google Scholar]
- 47.Prakash O, Srivastava PK, Jyoti B, Mushtaq R, Vyas T, Usha P. Radiographic evaluation of anterior loop of inferior alveolar nerve: a cone-beam computer tomography study. Niger J Surg. 2018;24:90–94. doi: 10.4103/njs.NJS_1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Demir A, Izgi E, Pekiner FN. Anterior loop of the mental foramen in a Turkish subpopulation with dentate patients: a cone beam computed tomography study. J Marmara Univ Inst Health Sci. 2015;5:231–238. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.