Abstract
Introduction
Tracheostomy is a very common procedure performed in ICU as it offers significant advantages over prolonged endotracheal intubation. It facilitates weaning by decreasing the work of breathing in patients with limited reserve by decreasing the dead space area, decreases the requirement for sedation, and may allow for earlier patient mobilization, feeding, and physical and occupational therapy as compared to prolonged intubation along with lesser oral and oropharyngeal ulcerations, improves pulmonary toileting, and lowers incidence of pulmonary infections. Tracheostomy, however, is not devoid of risks. Complications may include hemorrhage, stoma infections and granulations, pneumothorax, subcutaneous emphysema, tracheal stenosis, tracheomalacia, and rarely death. Hence, performance of tracheostomy should be considerate to outweigh benefit-risk ratio.
Aims and objectives
To evaluate the early versus late tracheostomy for reduction of the length of ICU stay, incidence of nosocomial pneumonias, risk of laryngeal injury and mortality of mechanically ventilated patients.
Materials and methods
We conducted a retrospective study from May, 2019 to April, 2021 of patients being tracheostomized in medical ICU at Civil Hospital, Ahmedabad, who were previously intubated endotracheally and were on mechanical ventilation. The decision to tracheostomize would be taken by physicians in their routine rounds in ICU.
Results
Incidence of endolaryngeal complications like laryngotracheal stenosis, stomal granulations, fistula as well as nosocomial infections have lower incidence in early tracheostomy as compared to with late. Mortality remains same in both the groups as well as hospital and ICU stay.
Keywords: Tracheostomy, Mechanical ventilation, Nosocomial pneumonia, Laryngeal injury
Introduction
Tracheostomy is a very common procedure performed in ICU as it offers significant advantages over prolonged endotracheal intubation. It facilitates weaning by decreasing the work of breathing in patients with limited reserve by decreasing the dead space area [1, 2], decreases the requirement for sedation [3], and may allow for earlier patient mobilization, feeding, and physical and occupational therapy as compared to prolonged intubation. Recent studies have suggested that tracheostomy results in lesser oral and oropharyngeal ulcerations, improves pulmonary toileting, and lowers incidence of pulmonary infections [4].
Tracheostomy, however, is not devoid of risks. Complications may include hemorrhage, stoma infections and granulations, pneumothorax, subcutaneous emphysema, tracheal stenosis, tracheomalacia, and rarely death. Hence, performance of tracheostomy should be considered to outweigh benefit-risk ratio.
The timing of tracheostomy has always been a topic of debate since years. The American National Association of Medical Directors of Respiratory Care in 1989 stated that tracheostomy is indicated if mechanical ventilation is to be continued for more than 21 days while patients requiring mechanical ventilation for less than 10 days are candidates for endotracheal intubation[5]. There have been studies demonstrating the positive implications of tracheostomy done within 2–10 days of intubation(early), i.e. decrease in the length of ICU stay, decrease in incidence of nosocomial pneumonia, use of sedatives, and mortality[6, 7]. Whereas a recent randomized control trial done in 2014 (the TracMan trial) did not support the evidence of benefit of early tracheostomy in decreasing mortality and length of ICU stay.[8].
Another proposed advantage of tracheostomy is that there is a lower risk of laryngeal injury. Rates of early laryngeal injury following endotracheal intubation have been reported to be as high as 94%.[9] Long-term sequelae such as granulomas and laryngeal stenosis range from 5 to 12%, with increased length of endotracheal intubation associated with a higher incidence of stenosis.[10] Laryngeal injury, however, remains an important risk as the course of intubation lengthens.
Owing to the disparity in studies, we have decided to determine the effect of timing of tracheostomy on the morbidity of mechanically ventilated patients. We hypothesize that early tracheostomy reduces the length of ICU stay, incidence of nosocomial pneumonias, risk of laryngeal injury and mortality. We will also take into consideration the complications occurring due to tracheostomy and implications of any comorbid conditions in mechanically ventilated patients.
Objectives:
To evaluate the early versus late tracheostomy for reduction of the need for mechanical ventilation post tracheostomy,
length of ICU stay,
incidence of nosocomial pneumonias,
risk of laryngeal injury and.
mortality of mechanically ventilated patients.
Materials & Methods
Study Design
We conducted a retrospective study from May,2019 to April,2021 of patients being tracheostomized in medical and surgical ICU at Civil Hospital, Ahmedabad, who were previously intubated endotracheally and were on mechanical ventilation. The decision to tracheostomize was taken by intensivist in their routine rounds in ICU.
With respect to indications for tracheostomy, the following criteria or their combination were used:
subjects without any provision of liberation from MV,
prolonged MV, and.
weaning failure.
Exclusion criteria included.
patients < 12 years age.
pre-existent tracheostomy done at another hospital..
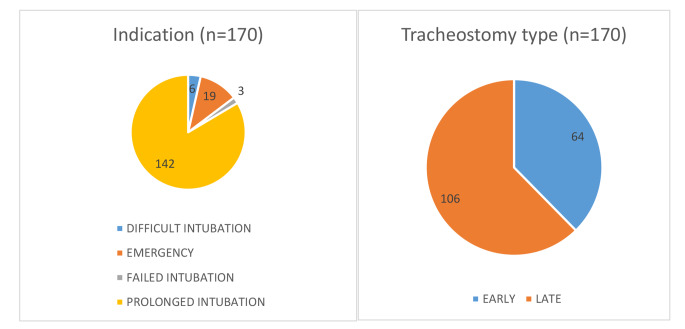
We divided patients mainly into two categories- the ones who were tracheostomized before 7 days(Early) and the ones after 7 days of endotracheal intubation(Late). Total 170 patients who fit in the criteria were included in the study, out of which 64 patients fell into the group of early tracheostomy i.e. within 7 days of intubation. 106 patients fell into the late tracheostomy group i.e. tracheostomy done after 7 days of intubation.
Data collected included Age, gender, cause and duration of mechanical ventilation, related co-morbid conditions, timing of tracheostomy, untoward incidents or complications during the tracheostomy. Medical records were analysed for length of ICU stay, duration of mechanical ventilation, incidence of nosocomial infections and mortalities. Nosocomial pneumonia was defined according to the Centers for Disease Control and Prevention (CDC) criteria [11]. The laryngeal injuries post tracheostomy like tracheal stenosis, stomal granulations, persistent tracheal fistula etc.were taken into consideration and compared in the early v/s late groups. Statistical analyses were performed with SPSS software for Windows (Statistical Product and Service Solutions, version 25.0.0, SSPS Inc, Chicago, IL, USA).
Results
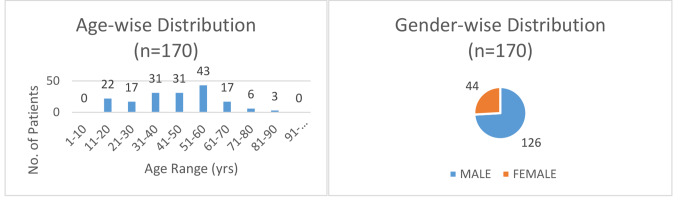
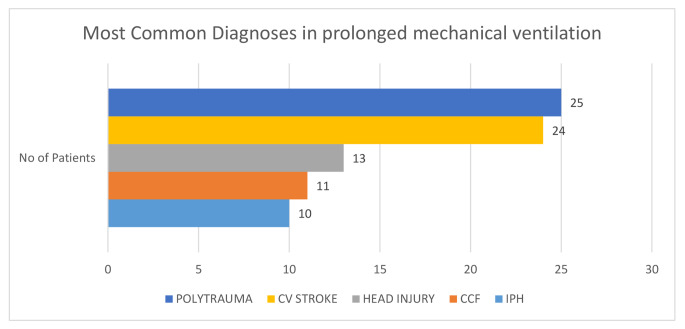
170 patients(126 males, 44 females) with different morbidities have been included in the study( 100 from medical ICU and 70 from the surgical ICU). 64 patients fell into the early tracheostomy group which is counted as tracheostomy done at or within 7 days of intubation amongst patients on mechanical ventilation. 106 patients fell into the late tracheostomy group, counted as tracheostomy done after 7 days of tracheostomy. Tracheostomy was performed 5.7 days (interquartile range (IQR) [5.0-6.2]) after intubation in the Early Tracheostomy group. In the Late Tracheostomy group, patients were tracheostomized after 11.4 days (IQR [11.0–12.0]). The most common indication for tracheostomy in prolonged intubation was found to be polytrauma(25) followed by CV Stroke(24).
Subjects who underwent early tracheostomy received mechanical ventilation for a mean days of 6.59 ± 2.49 compared to the late tracheostomy group which received mechanical ventilation for a mean days of 6.24 ± 2.003.(p value = 0.3168) which is not significant, proving no significant difference in early and late tracheostomy groups.
Similarly the duration of ICU stay was found to be 8.02 ± 2.952 days in early tracheostomy group compared to 7.57 ± 2.375 for late tracheostomy(p value = 0.277), again not significant. The incidence of nosocomial pneumonia calculated according to the criteria defined by Centers for Disease Control and Prevention (CDC) criteria was found to be 7.8% in early tracheostomy group compared to 15.1% in late tracheostomy group.
The incidence of tracheal stenosis post tracheostomy was found to be significantly high in late tracheostomy group (p value = 0.04) being 1.6% in early tracheostomy and 10.4% in late tracheostomy group. The incidence of stomal granulations was found to be 4.7% in early tracheostomy compared to 10.4% in late tracheostomy group. Persistent tracheal fistula incidence was 3.1% in early tracheostomy group compared to 4.7% in late tracheostomy group. Hospital mortality was the endpoint of this study. The incidence of mortality in early tracheostomy groups was 18.8% compared to 18.9% in late tracheostomy groups which is again not significant(p value = 1.000).
Fig. 1.
Graph 1 and 2 showing age and gender wise distribution of patients included in our study.
Fig. 2.
Graph 3 depicting diagnosis of patients in our study requiring prolonged mechanical ventilation and thus tracheostomy.
Fig. 3.
Graph 4 and 5 showing indications for tracheostomy and early v/s late tracheostomy.
Discussion
Despite its long history and widespread use in the critical care setting, tracheostomy continues to be considered a procedure of last resort to be used only when a prolonged trial of translaryngeal intubation fails. Early tracheostomy placement may lead to a markedly reduced duration of ventilation and shorter stays in critical care units in artificially ventilated, critically ill adult patients. However, the limited numbers of studies and patients available for analysis leave some doubt as to the accuracy of the result.
As concluded from our study incidence of nosocomial infections is almost double in patients of late tracheostomy contrary to the study done by Griffiths et al. which showed that the risk of developing hospital acquired pneumonia was unchanged by tracheostomy timing[12]. In a case control study of 185 patients who underwent a surgical tracheotomy, the rate of ventilator associated pneumonia was significantly lower when tracheotomy was performed within 7 days after admission to the ICU[13].
Optimal timing for tracheotomy remains a subject of debate and continued investigation. Despite earlier studies suggesting benefits from early tracheotomy (within 2 to 10 days after intubation) [14, 15], a recent randomized trial did not find any mortality benefit from such a practice[16] which is same result as in our study. Most recently, Brook et al., in an analysis of a cohort of 90 patients who had a tracheostomy, found that patients with an early tracheostomy (performed by day 10 of mechanical ventilation) had a mean duration of mechanical ventilation lower than patients with a late tracheostomy (performed after day 10 of mechanical ventilation), but the timing of tracheostomy was not associated with hospital mortality. One similar study by Griffiths et al. showed the same results that he timing of tracheostomy did not alter mortality significantly.[12].
The incidence of laryngotracheal stenosis was 8.9% (range, 0-20.8%), with a mean incidence of 8.1% in early tracheostomy groups and 10.9% in late tracheostomy in a study done by Curry et al. [17] which is persistent with findings in our study. Possible limitations of this study is that there is no defined criteria for early or late tracheostomy as different study groups tend to compare results based on their clinical interests.
Conclusions
From our study we concluded that the morbidity rate of tracheostomy is low and equivalent to that of translaryngeal intubation. The timing of tracheostomy has no effect on patient’s total days on the ventilator, intensive care unit days, and hospital stay. Where as, the incidence of pneumonia or other nosocomial infections is decreased if tracheostomy is performed within 7 days. There is no significant difference in mortality too in prolonged mechanically ventilated patients requiring tracheostomy whether we do it before or after 7 days. Laryngeal complications like laryngotracheal stenosis, stomal granulations and tracheal fistulas have higher incidence in late tracheostomy group as compared to patients in whom tracheostomy was done before 7 days.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Davis K, Jr, Campbell RS, Johannigman JA, Valente JF, Branson RD. Changes in respiratory mechanics after tracheostomy. Arch Surg. 1999;134(1):59–62. doi: 10.1001/archsurg.134.1.59. [DOI] [PubMed] [Google Scholar]
- 2.Diehl J-L, El Atrous S, Touchard D, Lemaire F, Brochard L. Changes in the work of breathing induced by tracheotomy in ventilator-dependent patients. Am J Respiratory Crit Care Med. 1999;159(2):383–388. doi: 10.1164/ajrccm.159.2.9707046. [DOI] [PubMed] [Google Scholar]
- 3.Nieszkowska A, Combes A, Luyt CE, et al. Impact of tracheotomy on sedative administration, sedation level, and comfort ofmechanically ventilated intensive care unit patients. Crit Care Med. 2005;33(11):2527–2533. doi: 10.1097/01.CCM.0000186898.58709.AA. [DOI] [PubMed] [Google Scholar]
- 4.Freeman BD, Morris PE. Tracheostomy practice in adults with acute respiratory failure. Crit CareMedicine. 2012;40(10):2890–2896. doi: 10.1097/CCM.0b013e31825bc948. [DOI] [PubMed] [Google Scholar]
- 5.Plummer A, Gracey D (1989) Consensus conference on artificial airways in patients receiving mechanical ventilation. Chest 96(1):178–1780 [DOI] [PubMed]
- 6.Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit CareMedicine. 2004;32(8):1689–1694. doi: 10.1097/01.ccm.0000134835.05161.b6. [DOI] [PubMed] [Google Scholar]
- 7.Scales DC, Thiruchelvam D, Kiss A, Redelmeier DA. The effect of tracheostomy timing during critical illness on long-term survival. Crit Care Med. 2008;36(9):2547–2557. doi: 10.1097/CCM.0b013e31818444a5. [DOI] [PubMed] [Google Scholar]
- 8.Young D, Harrison DA, Cuthbertson BH. Rowan,“Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: The TracMan randomized trial. J AmericanMedical Association. 2013;309(20):2121–2129. doi: 10.1001/jama.2013.5154. [DOI] [PubMed] [Google Scholar]
- 9.Colice GL, Stukel TA, Dain B. Laryngeal complications of prolonged intubation. Chest. 1989;96:877–884. doi: 10.1378/chest.96.4.877. [DOI] [PubMed] [Google Scholar]
- 10.Whited RE. A prospective study of laryngotracheal sequelae in long-term intubation. Laryngoscope. 1984;94:367–377. doi: 10.1288/00005537-198403000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Horan TCG, Gaynes RP (2004) “Surveillance of nosocomial infections,” in Hospital Epidemiology and Infection Control, C. G.Mayhall, Ed., pp. 1659–1702, LippincottWilliams &Wilkins, Philadelphia, Pa, USA, 3rd edition,
- 12.BMJ, doi:10.1136/bmj.38467.485671.E0 (published 23 May 2005) Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation.John Griffiths, Vicki S, Barber, Lesley Morgan, J Duncan Young [DOI] [PMC free article] [PubMed]
- 13.M¨oller MG, Slaikeu JD, Bonelli P, Davis AT, Hoogeboom JE, Bonnell BW. Early tracheostomy versus late tracheostomy in the surgical intensive care unit. Am J Surg. 2005;189(3):293–296. doi: 10.1016/j.amjsurg.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med. 2004;32(8):1689–1694. doi: 10.1097/01.CCM.0000134835.05161.B6. [DOI] [PubMed] [Google Scholar]
- 15.[14] DC, Scales D, Thiruchelvam A, Kiss, Redelmeier DA (2008) The effect of tracheostomy timing during critical illness on long-term survival. Crit Care Med 36(9):2547–2557 [DOI] [PubMed]
- 16.Young D, Harrison DA, Cuthbertson BH, Rowan K. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: The TracMan randomized trial. JAMA. 2013;309(20):2121–2129. doi: 10.1001/jama.2013.5154. [DOI] [PubMed] [Google Scholar]
- 17.Curry SD, Rowan PJ (2020 Feb) Laryngotracheal stenosis in early vs late tracheostomy: a systematic review. Otolaryngology–Head and Neck Surgery 162(2):160–167 [DOI] [PubMed]