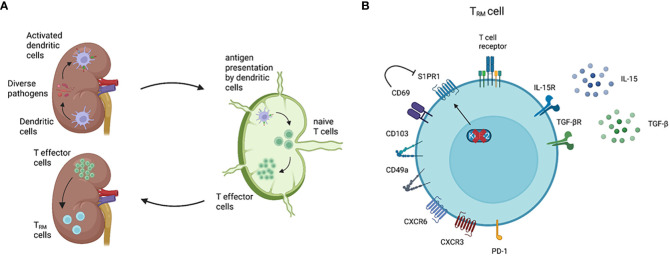
Figure 1.
General features of TRM cells. Renal TRM cell development and phenotype. (A) As classical antigen-presenting cells (APC), dendritic cells (DCs) constantly surveil their microenvironment for pathogens and microbes. Once DCs in the kidney are activated, these cells migrate to the renal draining lymph nodes to present the processed antigen via the major histocompatibility complex (MHC) to naïve T cells (3). Upon activation, naïve T cells become effector T cells and migrate to the inflamed kidney via a chemokine gradient (4). While most of the effector T cells undergo apoptosis following the resolution of inflammation, a small subset of the effector T cells become TRM cells. TRM cells are the most abundant immune cell population in the healthy human kidney (5). (B) A TRM cell marker CD69 downregulates the expression of S1PR1, which is a receptor required for tissue egress. The expression of transcription factor KLF-2, which upregulates S1PR1 expression, is downregulated in TRM cells (6). CD103 and CD49a are parts of the integrins αEβ7 and α1β1, respectively. CD103 interacts with E-cadherin on epithelial cells, whereas CD49a binds to collagen IV (2, 7). Almost all renal TRM cells express the chemokine receptor CXCR3 and, to a lower degree, CXCR6 (8). Inhibitory receptors, especially PD-1, are commonly expressed on TRM cells compared with circulating memory T cells. IL-15 and TGF-β are required to induce and maintain renal TRM cells in mice (9, 10). Created with BioRender.com