Abstract
Background
Illegal gold miners are currently key hosts for malaria in French Guiana (FG), with a risk of emergence of resistance linked to improper use of artemisinin-based combination therapy (ACT). The remoteness of the mines and regulatory issues hinder their access to health care.
Methods
A quasi-experimental researched project (Malakit) implemented in FG borders with Brazil and Suriname aimed at determining the effectiveness of distributed kits for self-diagnosis and self-treatment to illegal gold miners, after training, at strategic border staging areas. Evaluation relied on questionnaires at inclusion and follow-up visits, and pre/post intervention surveys. The primary outcome was the proportion of persons reporting a use of certified ACT after a positive malaria diagnosis. The secondary outcomes assessed antimalarial adherence, kit use and impact on malaria epidemiology.
Findings
The proportion of patients reporting a use of certified ACT after a positive diagnosis increased after the intervention (OR 1.8, 95%CI [1.1-3.0]). From April 2018 to March 2020, 3,733 persons participated in the intervention. The kit was used correctly by 71.7% [65.8-77.7] of the 223 persons reporting having used a malakit during the follow-up visits. No serious adverse events related to the misuse of malakit have been reported. The intervention appears to have accelerated the decline in malaria incidence in the region by 42.9%.
Interpretation
This innovative international project showed that people with low education can correctly self-manage their malaria symptoms. This strategy could be integrated in the malaria control programs of the countries involved and considered in other regions with residual malaria in remote areas.
Funding
This project was funded by the European Union, the Global Fund, Brazil MoH, Cayenne Hospital and FG Health Regional Agency.
Editor's note
This translation in French was submitted by the authors and we reproduce it as supplied. It has not been peer reviewed. Our editorial processes have only been applied to the original abstract in English, which should serve as reference for this manuscript. The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Contexte
Les chercheurs d'or illégaux sont actuellement un réservoir clé du paludisme en Guyane, avec un risque d'émergence de résistance lié à une mauvaise utilisation des combinaisons thérapeutiques à base d'artémisinine (ACT). L'isolement de ces sites miniers clandestins et des contraintes règlementaires entravent leur accès aux soins.
Méthodes
Un projet de recherche opérationnelle quasi-expérimental (Malakit) a été mis en œuvre aux frontières de la Guyane avec le Brésil et le Suriname. Il visait à déterminer l'efficacité de la distribution de kits d'autodiagnostic et d'autotraitement à des orpailleurs illégaux, après une formation adaptée, dans des zones stratégiques transfrontalières. L'évaluation s'est appuyée sur des questionnaires lors des visites d'inclusion et de suivi, et sur des enquêtes pré/post intervention. L'indicateur principal était la proportion de personnes déclarant avoir utilisé une ACT certifiée après un diagnostic positif de paludisme. Les indicateurs secondaires reposaient sur l'adhérence aux traitements antipaludiques, l'utilisation des kits et l'impact sur l'épidémiologie du paludisme.
Résultats
La proportion de patients déclarant une utilisation d'ACT certifiée après un diagnostic positif a augmenté après l'intervention (OR 1,8, 95%CI [1,1-3,0]). D'avril 2018 à mars 2020, 3 733 personnes ont participé à l'intervention. Le kit a été utilisé correctement par 71,7% [65,8-77,7] des 223 personnes revues en visites de suivi ayant déclaré avoir utilisé un malakit. Aucun événement indésirable grave lié à une mauvaise utilisation du malakit n'a été signalé. L'intervention semble avoir accéléré la diminution de l'incidence du paludisme dans la région de 42,9%.
Interprétation
Ce projet international innovant a montré que les personnes ayant un faible niveau d'éducation peuvent se prendre en charge par eux-mêmes pour des symptômes de paludisme. Cette stratégie pourrait être intégrée dans les programmes de lutte contre le paludisme des pays impliqués et envisagée dans d'autres régions où du paludisme résiduel persiste dans des zones isolées.
Financement
Ce projet a été financé par l'Union Européenne, le Fonds Mondial, le Ministère de la santé du Brésil, le Centre Hospitalier de Cayenne et l'Agence Régionale de Santé de Guyane.
Keywords: mobile population, malaria control, self-diagnosis, self-treatment, quasi-experimental design, interventional research, Amazon forest, Americas, vulnerable population
Research in context.
Evidence before study
Previous studies showed that illegal gold miners in French Guiana are key hosts for malaria. To propose an adapted response, we searched PubMed, Scopus and Google Scholar from 2000 to 2016 for interventional research on malaria control and/or elimination strategies in remote settings. We used the terms “malaria”, “control strategies”, “elimination strategies”, “vulnerable population”, “mobile population”, “remote areas”, “hard-to-reach population”. We read recommendations for malaria control and elimination from WHO/PAHO. We found that the malaria control strategies recommended by WHO or specific interventions tested for residual malaria described in the literature could not be implemented within the context of illegal gold miners in the Amazon forest of French Guiana due to regulatory, security and geographical reasons. One study in 2008 assessed self-diagnosis and self-treatment among expatriates being more than 24h from a medical center. The good results of this study concerning employees of an oilfield company with telephone medical assistance 7/7 could not be extrapolated to our study population which is administratively and socially precarious, low-educated, and very isolated. We decided to implement a strategy called Malakit based on the distribution of kits for self-diagnosis and self-treatment for malaria, with an adapted training relying on drawings and videos specifically developed for the population of illegal gold miners working in FG.
Added value of the study
This study was the first one assessing the use of self-diagnosis and self-treatment among a mobile, difficult-to-reach, and low-educated population in a cross-border area shared by three countries. It shows that this strategy is effective even in this challenging context of the Amazon forest and vulnerable population. The kits are reportedly well-used, with an impact on changing behavior in case of malaria symptoms and on malaria incidence in the region.
Implications of all the available evidence
These results showed that such a strategy challenges the health worker-patient paradigm. This could be adapted for use in other settings facing uncontrolled or residual malaria in mobile and difficult-to-reach populations. It could be a new tool in the box of malaria control strategies for specific residual malaria and thus reach the goal advocated by WHO to reduce incidence and mortality by 90% in 2030.
Alt-text: Unlabelled box
1. Introduction
The ten thousand or so illegal gold miners — mostly garimpeiros from Brazil — working in the French Guianese Amazon forest live in difficult conditions and face numerous health hazards [1]. Practicing an illegal activity, in a protected territory, without legal status, in remote areas and targeted by concomitant military operations in this French territory, access to care is difficult for them. Malaria is highly prevalent and, in this high transmission context, often asymptomatic [2,3]. The large use of under-the-counter (UTC) drugs (52%) has raised concerns about the risk of emergence of artemisinin-resistant P. falciparum which would compromise malaria treatment options [4,5]. This population of cross-border migrants typically represents a classical obstacle to malaria elimination — the solution to avert the rise of artemisinin-resistance [6,7]. Furthermore, garimpeiros’ mobility increases the risk of propagating malaria in the region, with reintroduction or recurrence of epidemics in areas where malaria was controlled. The most recent World Health Organization Global technical strategy for Malaria aims to reduce incidence and mortality by 90% between 2016 and 2030 [8]. To do so, anyone at risk of malaria should have access to diagnosis and treatment within 48 hours. For mobile, isolated or cross-border populations, such as clandestine garimpeiros in French Guiana (FG), this is often a challenge because the mines are up to six days on foot or canoe from health centers. However, if we aim to eliminate malaria in the region, it is crucial to focus on this elusive population which perpetuates most of the malaria transmission.
Facing regulatory, geographical, political and security issues, management of malaria cases directly on mining sites through health professional or community health workers cannot be implemented in FG [7,9]. To escape this deadlock, numerous discussions among health institutions and scientific partners from FG, Brazil and Suriname have led to the Malakit project based on the distribution of kits for self-diagnosis and self-treatment of Plasmodium infections — a paradigm-shift from traditional passive detection and treatment. Since gold miners are a mobile population across the Guiana Shield, kit distribution sites were implemented in staging areas at the Brazil-FG and Suriname-FG borders. A strong partnership with Brazil and Suriname was developed involving scientists, non-profit organizations, and local and national malaria control programs [10].
This new strategy was implemented as an intervention research project in order to evaluate its effectiveness, participant's responsiveness and safety. This article details the main results of this two-year project and its relevance to other contexts.
2. Material and methods
2.1. Study design
Malakit is an international and multicentric interventional study sponsored by Cayenne Hospital with a quasi-experimental design, based on a single group intervention and an independent pre/post evaluation including participants regardless their participation or non participation in the malakit intervention [11]. These cross-sectional surveys before and after the Malakit intervention (“pre/post intervention surveys”) assessed behavior and malaria prevalence among gold miners sampled by snow-ball effect at the staging areas where garimpeiros entered French Guiana from Brazil and Suriname (Figure 1). Independently, inclusions in the Malakit intervention and follow-up visits were performed overall from April 2018 to March 2020, with a progressive roll-out in the five inclusion sites located at staging areas for gold miners. Table 1 describes the design, inclusion criteria, main outcomes and data collection; the methodology has been previously published [9,10,12] and further details are available at www.malakit-project.org.
Figure 1.
Inclusion sites for pre/post intervention surveys and malakit intervention, at the borders of French Guiana with Brazil and Suriname, 2015-2020
Table 1.
Design, main outcomes and inclusion criteria of Malakit intervention and pre/post intervention surveys, French Guiana –Brazil-Suriname, 2015-2020
| Pre intervention survey | Post intervention survey | Malakit intervention | |
|---|---|---|---|
| Aim | To evaluate the effectiveness of the Malakit intervention strategy | To assess the use of the kits by the study participants | |
| Inclusion sites | Gold miners staging areas* located along the Brazilian and Surinamese border of French Guiana | Five distributions sites located in the gold miners staging areas along the two borders and in Paramaribo (capital of Suriname) | |
| Investigating center | • Surinamese border: Centre d'Investigation Clinique (CIC) Antilles-Guyane, Inserm 1424, CH Cayenne, FG • Brazilian border: Foundation Oswaldo Cruz (Fiocruz), Rio de Janeiro, Brazil |
Sponsor: CIC Inserm 1424, CH Cayenne Principal Investigator (PI) in FG: Dr Douine (CIC) PI in Suriname: Dr Vreden (SWOS Foundation) PI in Brazil: Dr Suarez-Mutis (Fiocruz) |
|
| Data collectors | One physician, one nurse and one facilitator | Nine Malakit facilitators | |
| Roll-out | • Surinamese border: January to June 2015 • Brazilian border: May-June and October-November 2018 |
October-December 2019 | • Surinamese border: April 2018-March 2020 • Brazilian border: October 2018- March 2020 |
| Population | People that work on the illegal gold mining sites in French Guiana | ||
| Inclusion criteria | • Be 18 years old or more (16 on the Brazilian border) • Work or accompany someone on a clandestine gold mining site in French Guiana • Be out of the forest for less than 7 days • Give a written consent |
• Be 15 years old or more • Intend to work or accompany someone on a clandestine gold mining site in French Guiana |
|
| Types of data | Cross-sectional data |
Longitudinal data | |
| Initial data to estimate the indicators before Malakit | Final data to estimate the indicators after Malakit | Data collected at inclusion and follow-up visits as part of the monitoring of the intervention | |
| Data collection | Questionnaires were administered by the facilitators for socio-economic data and behavior during the last malaria episode. They were collected on paper or with the help of tablets that transferred the anonymized data to a secure online database, Clinsight. A venous blood sample was taken for each participant to perform a PCR-Plasmodium at the Pasteur Institute of FG. A RDT was performed on site and participants who tested positive were referred to the nearest health facility for confirmation by microscopy, notification and treatment. | During each visit, facilitators administered a questionnaire and filled out the electronic form with the open-source ODK Collect application on Android tablets. Each completed questionnaire generated a record that was immediately encrypted and sent to a server managed by Ona when an Internet connection was available. Data retrieval, decryption, and aggregation were performed using a specifically developed R package. The data collected by the facilitators was subjected to a real-time validation process by the sponsor's supervisory team to verify its quality. | |
| Main outcome | Difference between the proportion of participants who reported appropriate behavior (i.e., using a certified ACT after a positive malaria test by using a kit or turning to the health system) before/after the Malakit intervention. | ||
| Secondary outcomes | Coverage of the study population by the intervention • proportion of participants in the post intervention survey who were included in the Malakit intervention |
Number of kits distributed |
|
| Difference of treatment adherence before/after the intervention and according to the behavior • proportion of good treatment adherence in the pre/post intervention surveys assessed by questionnaire |
Proportion of the kit users included in the Malakit intervention, who used their kit correctly during the first episode of malaria symptoms reported on the last follow-up visit • defined as having taken the whole medication (Artemether-lumefantrine) in three days after a positive RDT or no antimalarial after a negative RDT |
||
| Ability to perform self-RDT and knowledge about malaria treatment for participants included in the Malakit intervention • realization of a RDT themselves in front of the facilitator • questionnaire about malaria treatment |
|||
| Modification of Plasmodium-PCR prevalence pre/post the Malakit intervention • assessed by multiplex real-time PCR derived from Shokoples et al. [14] |
Proportion of Malakit participants who acquired a kit before inclusion • assessed by questionnaire |
||
| Reported adverse events • notification detailed in Suppl. Mat. 2 |
|||
| Impact on malaria epidemiology in the region • modeling based on data from passive surveillance systems of Brazil and Suriname |
|||
| Ethics and regulation | • in Brazil: Approval from the Fiocruz Ethics Committee (Opinion Number 2.560.415) • in Suriname: Approval from the CMWO (Commissie voor Mensgebonden Wetenschappelijk Onderzoek) (Opinion Number VG10-14) • in France: Approval from INSERM Ethics Evaluation Committee (No. 14-187 of 09.12.2014) |
• in Brazil: Approval from the Fiocruz Ethics Committee (Opinion Number 2.560.415) • in Suriname: Approval from the CMWO (Opinion Number DVG-738) |
• in Brazil: Approval from the Fiocruz Ethics Committee (Opinion Number 2.831.534) • in Suriname: Approval from the CMWO (Opinion Number VG 25-17) |
* staging areas are specific neighborhoods in border towns or small informal settlements located on border rivers where gold miners come to rest, buy supplies or sell their gold.
2.2. Study population
The study population consisted of individuals working in illegal gold mines in French Guiana regardless of the nature of their activity (seller, cook, gold miner…) estimated at 10,000 persons [13].
Each stage of the project (pre-intervention survey / intervention / post-intervention survey) included independent samples from the same study population.
2.3. The malakit and its associated-training
The kits contained three rapid diagnostic tests (RDT) CareStart™ Malaria pLDH(Pan) (detecting the four species without distinction) with one complete treatment consisting of artemether-lumefantrine 20mg/120mg (AL) and a single dose of primaquine (15 mg). In the region, AL treatment is efficient on both P. falciparum malaria and P. vivax malaria attacks. The single dose of primaquine was added to decrease the transmission of P. falciparum, the predominant Plasmodium species at the time of Malakit implementation [2]. This RDT was chosen because of its stability at up to 40°C given that the average temperature range in the Amazon is 25-27°C [10]. The kit was given to participants after they gave written informed consent and received forty-minutes training to ensure that they understood how to use the kit and how to make a RDT that they had to do by themselves in front of the facilitator. They were also informed about the two endemic Plasmodium species in FG and of the possibility of relapses in the case of P. vivax infection. Training tools such as videos, drawings (printed directly on the kit's plastic pouch), and a smartphone application were developed to improve the proper use of the kits by the participants [10,14]. Passive follow-up was then conducted, with participants returning at their convenience after using, losing or donating the kit to obtain a new one [10]. During these follow-up visits, questionnaires assessed the correct use of the kit (handling, RDT performed before taking the treatment, RDT result interpretation…).
2.4. Objectives and evaluation criteria
The first objective of the project was to evaluate if the strategy led to an increase of a reported appropriate behavior in case of malaria symptoms, defined as using a certified ACT after a positive malaria test by using a kit or turning to the health system. It was assessed by the pre/post intervention surveys.
-
•
The last malaria episodes, before or after the Malakit implementation, were classified according to Suppl. Mat. 1.
-
•
Data on the behavior during the last malaria episode was derived from the question "what did you do during your last episode of malaria symptoms?". Given the mixed care pathways, we took into consideration the first action taken. Health-seeking behavior was thus classified into four groups,: i) use of self-medication with UTC drugs; ii) care sought in a health center/hospital (in any country); iii) use of a malakit; iv) other: traditional plant-based remedies, treatment of symptoms only, or no memory about the behavior.
Secondary objectives (detailed in Table 1) were to assess intervention coverage, changes in adherence to antimalarial, knowledge and practice of kit use, impact on malaria epidemiology (prevalence and incidence), and participant safety.
-
•
Good treatment adherence was assessed by the pre/post intervention surveys and was defined as having taken the whole antimalarial course received.
-
•
Knowledge of kit use was assessed by asking Malakit participants included in the post-intervention surveys to redo a RDT in front of the interviewer and to explain how to follow the treatment.
-
•
A correct malakit use was defined as having taken the whole medication in three days after a positive RDT or no antimalarial after a negative RDT according to data obtained during follow-up visits of participants to the Malakit intervention. The malaria prevalence in the pre/post surveys was assessed by multiplex real-time PCR derived from Shokoples et al. [15], to take into account the submicroscopic carriers, which were predominant in the pre-intervention surveys [2]. The detection threshold was of one parasite/µl of blood for the five species of malaria, after DNA extraction of 200µl of whole blood with QIAamp® DNA kit (Qiagen).
-
•
The impact on malaria incidence in the region was assessed by using data from the surveillance systems of Brazil and Suriname.
-
•
Safety follow-up was implemented to monitor potential adverse events (data collection process presented in Suppl. Mat. 2).
An independent Data Safety Monitoring Board (DSMB) was created to advise the sponsor on safety of the intervention during the project. The four international malaria experts gathered once a year to assess the data and the reports produced by the project coordination team.
2.5. Analyses
We presented categorial variables as frequencies and proportions, and continuous variables as median and interquartile range. Comparisons used chi2 or student tests, respectively.
Longitudinal data collected at follow-up visits during the intervention was used to assess appropriate kit use. Some participants reported several kit use events (i.e. performing an RDT and/or using AL from a kit), the indicator of correct kit use was thus calculated by participant and by kit use event. For each participant, the first kit use event of the most recent visit was selected to ensure that the participant had a complete kit before use. Three levels of analysis were conducted, in order of thoroughness: raw analysis, intermediate analysis, ‘per protocol’ analysis (Suppl. Mat. 3).
For cross-sectional data, the comparison of the main indicator before and after the intervention was based on the odds-ratio calculated by univariate unconditional logistic regression.
After collection of data from the surveillance systems of Brazil and Suriname for January 2015- March 2020, an interrupted time series (ITS) analysis was performed to evaluate the intervention's impact on malaria cases imported from French Guiana to Suriname and to Brazil during this period [16]. The monthly average temperature in Cayenne was used as a proxy to account for regional seasonality. The ITS model was constructed as a segmented linear regression before and after the Malakit intervention, without immediate effect of the intervention. Standard errors were adjusted for autocorrelation with a Heteroscedasticity and Autocorrelation Consistent Covariance Matrix Estimation.
Data were analyzed using Stata13 and R (v4.0.2) with RStudio (v1.3.1056-1). Two-sided p-values <5% defined statistical significance.
2.6. Ethics and regulation
Each participant gave a written consent after clear and appropriate information. Ethics approvals were obtained from countries where the project was implemented (Table 1). The project was the subject of a Normal CNIL Declaration on 24 May 2018 (Declaration Number 2188949 v 0) for data analysis according to the General Data Protection Regulation (European Union Regulation 2016/679).
2.7. Role of the funding sources
The funding sources did not have any role in the collection and analysis of the data, nor in the decision to submit the paper for publication.
3. Results
3.1. Study population
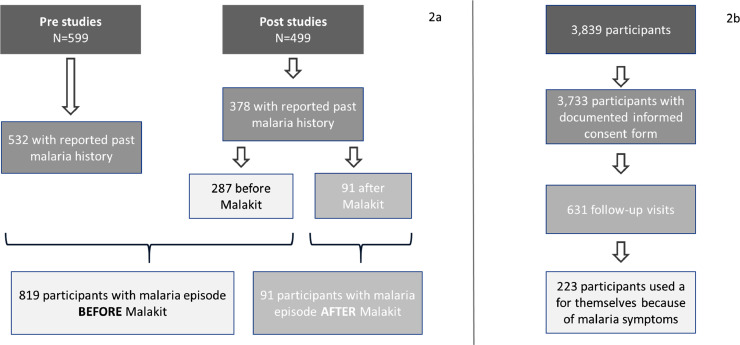
In total, 3,733 participants were included in the Malakit intervention and 1,098 in the pre/post intervention surveys (Figure 2). The samples were similar: participants were mainly from Brazil (96%), with a median age of 38 years old, working for a median of 10 years in gold mining (Table 2).
Figure 2.
Flow chart of participants to pre/post intervention surveys (2a) and to Malakit intervention (2b)
Table 2.
Socio-demographic characteristics and gold mining activity among participants in pre/post intervention surveys, in the Malakit intervention and those who returned for follow-up visit, French Guiana – Brazil – Suriname, 2015-2020
| Pre/post intervention surveys participants N=1,098 n (%) | Malakit intervention All participants N = 3,733 n (%) | Malakit intervention returned participants N = 631 n (%) | |||
|---|---|---|---|---|---|
| Socio-demographic data | |||||
| Age (years) | Median age [IQR] | 38 [31-47] | 38 [30-47] | 38 [30-47] | |
| <= 29 | 241 (22.0) | 932 (25.0) | 149 (23.6) | ||
| 30-44 | 513 (46.9) | 1651 (44.2) | 280 (44.4) | ||
| >= 45 | 340 (31.1) | 1150 (30.8) | 202 (32.0) | ||
| Sex | Female | 275 (25.1) | 1255 (33.6) | 251 (39.8) | |
| Male | 823 (74.9) | 2478 (66.4) | 380 (60.2) | ||
| Education level | None or primary | 554 (50.6) | 2244 (60.1) | 363 (57.5) | |
| Secondary or superior | 541 (49.4) | 1489 (39.9) | 268 (42.5) | ||
| Country of birth | Other than Brazil | 43 (3.9) | 87 (2.3) | 14 (2.2) | |
| Brazil | 1 055 (96.1) | 3646 (97.7) | 617 (97.8) | ||
| Maranhão | 575 (54.5) | 1920 (52.7) | 313 (50.7) | ||
| Para | 237 (22.5) | 907 (24.9) | 175 (28.4) | ||
| Amapa | 92 (8.7) | 363 (10.0) | 56 (9.1) | ||
| other | 149 (14.1) | 451 (12.4) | 73 (11.8) | ||
| missing data | 2 (0.2) | 5 (0.1) | 0 (0.0) | ||
| Inclusion site | Surinamese border | 801 (72.9) | 2377 (63.7) | 446 (70.7) | |
| Brazilian border | 297 (27.1) | 1356 (36.3) | 185 (29.3) | ||
| Gold mining activity | |||||
| Time in gold mining | no experience in gold mining | Exclusion criterion | 329 (8.8) | 25 (4.0) | |
| ≤ 5 years | 349 (31.9) | 1149 (30.8) | 198 (31.4) | ||
| 6-10 years | 276 (25.2) | 831 (22.3) | 150 (23.8) | ||
| 11-15 years | 184 (16.8) | 497 (13.3) | 107 (17.0) | ||
| > 15 years | 286 (26.1) | 785 (21.0) | 132 (20.9) | ||
| missing data | - | 142 (3.8) | 19 (3.0) | ||
| Time in the last mining site | Median time in years [IQR] | 0.5 [0.25-2] | 0.6 [0.25 - 2]* | 1 [0.25-2] | |
| Travel time to the gold mining site | <2 hours | 72 (6.6) | - | - | |
| 2 hours to half day | 260 (23.9) | - | - | ||
| 1 day | 285 (26.2) | - | - | ||
| > 1 day | 432 (39.6) | - | - | ||
| Do not know | 41 (3.8) | - | - | ||
| Main occupation | Gold miner | 578 (52.6) | 1860 (49.8) | - | |
| Trader | 188 (17.1) | 706 (18.9) | - | ||
| Cook/housekeeper | 153 (13.9) | 702 (18.8) | - | ||
| Carrier/boat driver | 73 (6.6) | 171 (4.6) | - | ||
| Machine owner | 45 (4.1) | 118 (3.2) | - | ||
| Shop/bar owner | 17 (1.5) | 37 (1.0) | - | ||
| Sex worker | 3 (0.3) | 44 (1.2) | - | ||
| Other/unemployed | 36 (3.3) | 75 (2.0) | - | ||
| Missing | 5 (0.5) | 20 (0.5) | - | ||
| Type of activity | Non-mobile activity | 825 (75.3) | 2836 (76.0) | 412 (65.3) | |
| Mobile activity | 268 (24.5) | 877 (23.5) | 217 (34.4) | ||
| Do not know | 2 (0.2) | 20 (0.5) | 2 (0.3) | ||
| Number of exits from mining site > 3 days during the last year | Median [IQR] | 3 [1-6] | 2 [1-3]* | 2 [1-4] | |
* among participants with past experience in gold mining
3.2. Pre/post intervention surveys: behavior change in case of malaria symptoms
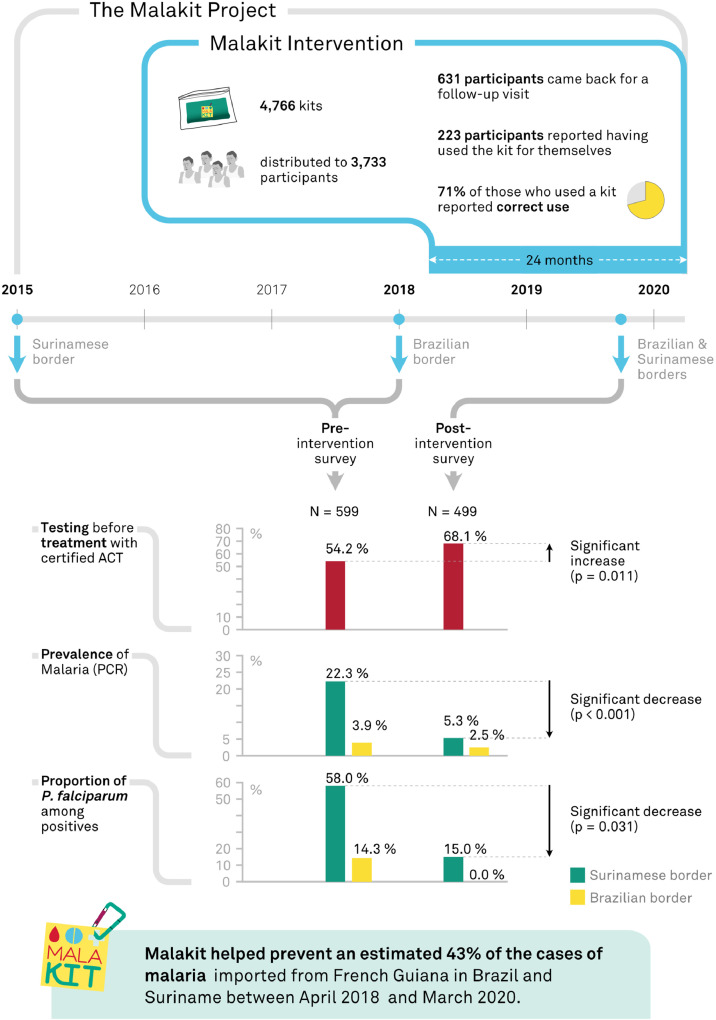
The reported appropriate behavior (using a malakit or turning to the healthcare system) in case of malaria symptoms increased from 54.2% (444/819) to 68.2% (62/91): OR=1.8 (95%CI [1.1-3.0]) (Figure 3). Males and those leaving the forest less often seemed most likely to self-medicate without diagnosis, but this failed to reach statistical significance (Table 3).
Figure 3.
Main outcomes from the Malakit project (Malakit intervention and pre/post intervention surveys), French Guiana – Brazil – Suriname, 2015-2020
Table 3.
Socio-demographic profile of participants reporting use of a certified ACT after a positive malaria test using a kit or turning to the health system during the last episode of malaria symptoms, French Guiana-Brazil-Suriname, 2015-2020
| Self-medication with UTC drugs n=27 | "Appropriate behavior" (using a malakit or turning to the healthcare system) n=62 | p | |||
|---|---|---|---|---|---|
| Socio-demographic data | |||||
| Age | <= 29 yo | 9 (36.0) | 16 (64.0) | 0.601 | |
| 30 - 44 yo | 10 (25.0) | 30 (75.0) | |||
| >= 45 yo | 7 (31.8) | 15 (68.2) | |||
| Sex | Female | 5 (17.9) | 23 (82.1) | 0.066 | |
| Male | 22 (36.1) | 39 (63.9) | |||
| Education level | None or primary | 14 (33.3) | 28 (66.7) | 0.363 | |
| Secondary or superior | 13 (27.7) | 34 (72.3) | |||
| Country of birth | Other than Brazil | 0 (0) | 0 (0) | / | |
| Brazil | 27 (30.3) | 62 (69.7) | |||
| Inclusion site | Surinamese border | 13 (27.7) | 34 (72.3) | 0.363 | |
| Brazilian border | 14 (33.3) | 28 (66.7) | |||
| Gold mining activity | |||||
| Time in gold mining | <= 10 years | 19 (30.2) | 44 (69.8) | 0.572 | |
| >10 years | 8 (30.8) | 18 (69.2) | |||
| Time in the last mining site | <= 6 months | 13 (26.5) | 36 (73.5) | 0.237 | |
| > 6 months | 14 (35.9) | 25 (64.1) | |||
| Travel time to the gold mining site | <=1 day | 7 (33.3) | 14 (66.7) | 0.928 | |
| > 1 day | 18 (26.0) | 44 (71.0) | |||
| dnk | 2 (33.3) | 4 (66.7) | |||
| Type of activity | Non-mobile activity | 20 (31.3) | 44 (68.7) | 0.489 | |
| Mobile activity | 7 (28.0) | 18 (72.0) | |||
| Number of mines they have worked at in the last 3 years | <=3 | 19 (31.7) | 41 (68.3) | 0.446 | |
| >3 | 8 (27.6) | 21 (72.4) | |||
| Number of exit from mining site > 3 days during the last year | <=4 | 21 (35.6) | 38 (64.4) | 0.103 | |
| >4 | 5 (19.2) | 21 (80.7) | |||
3.3. Kit distribution and coverage
During the two-year study period, 4,766 kits were distributed, with a median of 50 kits per distribution site per month. In the independent sample of the post-intervention survey, 64.8% [60.6-69.0] of the participants had already heard about the Malakit project, among whom 46.1% [40.6-51.6] had been included. Thus, we estimated that 29.7% [25.7-33.7] of the target population had been included before the end of 2019. The main reasons reported for not having been included were: not having the opportunity to go to a distribution site (40/135, 29.6%), lack of time to participate to inclusion questionnaire and training (30/135, 22.2%), or lack of interest (24/135, 17.8%).
3.4. Treatment adherence before/after the intervention and according to the behavior
Global antimalarial adherence seemed not different before/after the intervention (590/745=79.2% versus 67/82=81.7%, p=0.593). However, reported adherence to antimalarial treatment was similar between participants who sought care in a health center (397/434=91.5%) or who used a malakit (27/33=81.8%) (p=0.125), and it was lower when the participant used UTC medication (233/360=64.7%, p<0.001).
3.5. Malakits’ reported use during the intervention follow-up visits
Of the 631 participants in the Malakit intervention who returned for a follow-up visit, 223 reported using a kit for themselves at least once (Table 4). Among them, 71.7% [65.8-77.7] used the kit correctly: 71.1% [64.2-78.0] correctly took the treatment after a positive RDT and 79.2% [68.3-90.2] of persons with a negative RDT did not take the treatment (intermediate analysis). The different levels of analysis, by kit use event and by participants, showed comparable results (Suppl. Mat. 3). The overall good antimalarial adherence was 69.4% [62.5-76.3]. Perceived health condition after the use of a malakit was “much better” according to 89.2% of the participants who had reported a positive RDT, and 92.9% of those who had taken the treatment correctly.
Table 4.
Kit use by participants of the Malakit intervention, 2018-2020
 |
* AL from the kit taken completely for three days
** AL from the kit not taken in full and/or for a duration other than three days
*** no ACT taken
3.6. Kit use knowledge
In the post-intervention surveys, participants who previously took part in the Malakit intervention showed a good ability to redo and interpret the results of the RDTs: 85.1% were able to do it correctly by themselves (Table 5). However, their knowledge about the treatment was insufficient not as good: 53.4% of these participants were able to re-explain malaria treatment modalities accurately.
Table 5.
Knowledge on kit use among Malakit participants included in the post intervention surveys
| Items | Score | n (%) | Median age [IQR] | % of female | |
|---|---|---|---|---|---|
| Capacity to perform a RDT among the persons participating in Malakit included in the post intervention survey (N=107*) | |||||
| • put the blood in the right place on the cassette • put the reagent in the right place • use the right number of drops of the reagent • correct time to wait before looking at the result • interpret correctly the result |
score 5/5 | 45 (42.1) | 91 (85.1) | 35 [26-42] | 36.3% |
| score 4/5 | 30 (28) | ||||
| score 3/5 | 16 (15) | ||||
| score 2/5 | 5 (4.7) | 16 (14.9) | 46 [35-50.5] | 25% | |
| score 1/5 | 5 (4.7) | ||||
| score 0/5 | 6 (5.6) | ||||
| p-value | p=0.003 | p=0.382 | |||
| Capacity to explain the malaria treatment among the participants un Malakit included in the post intervention survey (N=88**) | |||||
| • taking the AM-LM after a positive malaria diagnosis test • taking the two primaquine tablets with the first AM-LM medication} • taking four AM-LM tablets twice a day • taking AM-LM tablets for three days • if the RDt is negative only paracetamol should be taken |
score 5/5 | 26 (29.6) | 47 (53.4) | 36 [27-47] | 45% |
| score 4/5 | 14 (15.9) | ||||
| score 3/5 | 7 (8.0) | ||||
| score 2/5 | 14 (15.9) | 41 (46.6) | 36 [31-43] | 29% | |
| score 1/5 | 19 (21.6) | ||||
| score 0/5 | 8 (9.1) | ||||
| p-value | p=0.817 | p=0.136 | |||
* evaluation carried out only on the Surinamese border and 10 refusals
** evaluation carried out only on the Surinamese border, 29 missing data
3.7. Impact on malaria epidemiology
The pre/post surveys showed that PCR-Plasmodium prevalence in garimpeiros decreased between 2015 and 2019 (22.3% to 5.3%) on the Maroni border and, less clearly, on the Oyapock border from 3.9% in 2018 to 2.5% in 2019 (Table 6). The decrease was also apparent for asymptomatic carriage. At the same time, the proportion of P. falciparum dropped on the two borders in favor of a large predominance of P. vivax.
Table 6.
PCR-Plasmodium prevalence among gold miners in pre/post intervention surveys
| Pre intervention survey |
Post intervention survey |
|||
|---|---|---|---|---|
| Surinamese border | Brazilian border | Surinamese border | Brazilian border | |
| Time period | Jan-Jun 2015 | May-Jun 2018 and Nov 2018 | Oct-Dec 2019 | Oct-Dec 2019 |
| N | 421 | 178 | 380 | 119 |
| Plasmodium-PCR positive (n) | 94 | 7 | 20 | 3 |
| Plasmodium-PCR prevalence % [95% CI] | 22.3 [18.3-26.3] |
3.9 [1.6-7.9] |
5.3 [3.0-7.5] |
2,5 [0.5-7.2] |
| Species | Pf=47.9% Pv=37.2% Pm=3.2% Pf+Pv=10.6% Pv+Pm=10.6% |
Pf=14.3% Pv=85.7% |
Pf=15.0% Pv=75.0% Pm=10.0% |
Pv=100% |
| Asymptomatics carriage* % [95% CI] | 18.7 [15.1-22.8] |
3.9 [1.6-7.9] |
4.5 [2.6-7.1] |
0.8 [0.02-4.6]] |
| p-value PCR prevalence pre/post | <0.001 | 0.745 | ||
| p-value asymptomatic carriage pre/post | <0.001 | 0.227 | ||
*definition on the Brazilian border = having fever at the time of inclusion, on the Surinamese border = reporting fever in the last 48 hours and/or having fever at the time of inclusion
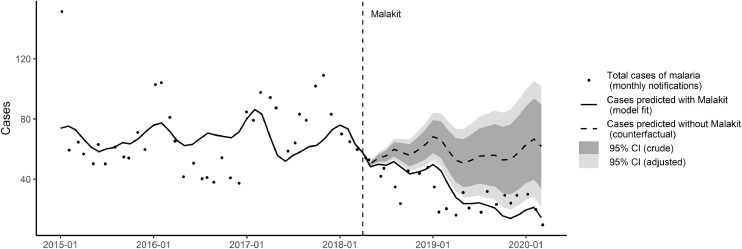
Between April 2018 and March 2020, a total of 695 incident malaria cases imported from French Guiana were notified to the Brazilian and Surinamese national surveillance systems. For the same period, the interrupted time series model predicted an estimated 758 cases notified with the Malakit intervention, and predicted 1,327 cases in the scenario without Malakit (crude 95%CI: 990-1,664; HAC-adjusted: 845-1,808). When comparing the predicted number of cases with and without Malakit, this corresponds to a prevention of 42.9% of malaria cases (crude 95%CI: 23.4 -54.4, HAC-adjusted: 10.3-58.1) (Figure 4, Table 7).
Figure 4.
Estimation of the impact of Malakit on the total number of malaria cases notified monthly in Brazil and Suriname as imported from French Guiana between January 2015 and March 2020. Interrupted time series model: cases predicted with Malakit (model fit, solid line) vs. without (counterfactual, dashed line). Vertical dashed line: start of Malakit in April 2018.
Table 7.
Interrupted time series model of the impact of Malakit intervention (April 2018 – March 2020) on cases of malaria from French Guiana, notified monthly in Suriname and Brazil as imported from French Guiana: estimates of model coefficients.
| Coefficient estimate | p-value (crude) | p-value (adjusted) | |
|---|---|---|---|
| Time (months) | -0.26 | 0.280 | 0.412 |
| Time since Malakit start (months) | 2.06 | 0.001 | 0.021 |
| Mean temperature (3-month lag,°C) | 17.19 | 0.006 | <0.001 |
| Constant | -396.42 | 0.018 | 0.003 |
3.8. Safety data
No serious adverse events were reported by participants, facilitators or health centers (Suppl. Mat. 4). Treatment interruption for adverse effects was rare (1.0%).
The circulation of kits outside the Malakit study was limited. Very few people (7/631) attended follow-up visits to get a new kit over five times. Among Malakit participants, 1.1% had already acquired a kit before inclusion. The reported cost on the black-market was stable throughout the project (on average 2.6 g of gold (about 80 USD) for a complete malakit).
4. Discussion
This study shows that, for specific populations living in very isolated areas that are not reachable by health care services, self-diagnosis and self-treatment of malaria is a feasible solution: if associated with an adapted training and free-of-charge tests and medication distribution, it allows an improvement in malaria symptoms management. This strategy increased by 25.8% the overall diagnosis of malaria in case of symptoms (by using a malakit or by going to a health center). Even with a low educational level, the participants could use the malakits correctly, i.e. perform a RDT and use ACT properly. The intervention was safe and participated in the reduction in malaria incidence in the region.
4.1. Some limitations for the interpretation of the study
The primary outcome, behavioral change in case of malaria symptoms, and secondary outcomes, reported treatment adherence and use of malakit, were declarative and subject to bias: (i) expected response bias, with underreporting of kit sales or misuse; (ii) overrepresentation of health-conscious persons; and (iii) memory bias regarding behavior during the last episode of malaria, particularly regarding treatment adherence. Adverse events may have been under-reported by health centers, facilitators and participants. Since biases were considered to be identical before and after the implementation of the strategy, it was legitimate to interpret the difference. Strict definitions were used in order to counterbalance potential biases.
4.2. But a successful strategy
4.2.1. An adapted design with rigorous data collection
In isolated areas or among mobile populations, randomized studies are hardly feasible. Moreover, Malakit was a population intervention with risks of inter-individual contamination and individual randomization would not have been suitable. Cluster randomization would have been limited to a low number of clusters and complicated by the mobility of the individuals [17]. Other regions of the world adopted pragmatic designs to evaluate interventions, as in Cambodia [18], Myanmar [19] or Mozambique [20], designs which have the advantage of being feasible and adapted to particular contexts, albeit with a lower level of evidence. To counterbalance these limitations, the Malakit project benefited from innovative data collection tools adapted to the Amazon context, a strong monitoring and diverse and rigorous data collection sources from facilitators and pre/post surveys [12], but also from external qualitative assessment [21] and on-field investigation (personal data). The consistency of the results of the different analyses reinforces their robustness through a convergence of evidence.
4.2.2. A good participant responsiveness
The participation of almost a third of the study population in the Malakit intervention suggests that this strategy corresponds to a real need together with an appropriate solution. Indeed, gold miners are people living in precarious and hostile conditions, but have a strong desire to be empowered in managing their health [13]. The fact that the facilitators belonged to the same community enhanced the participants’ trust for training and data collection [21].
4.2.3. A correct kit use
Despite the low level of education of the gold miners (50% of them have never been to school or stopped at primary level [1]), the creation of specific training tools using a participatory approach [10,14] and participant training by facilitators in their own language proved to be very effective: the proportion of correct kit use was 71.7% with a strict definition. Although overall treatment adherence was not significantly better after the intervention, it was higher when the participant used a malakit or went to a health care facility. The proportion of good adherence appears consistent with the literature since 2000 which shows that adherence tends to be higher when informed consent was collected at the time of obtaining the drug, when patient consultations were directly observed by research staff, and when a diagnostic test was obtained [22], all the factors that come together in the Malakit strategy.
4.3. Impact of the intervention on malaria epidemiology
The incidence and prevalence of malaria decreased significantly during the Malakit intervention in FG and in the surrounding territories (Suriname, Amapá), in illegal garimpeiros as well as in local inhabitants and so did the number of malaria cases imported from French Guiana to Suriname or Brazil [23], [24], [25], [26]. This decrease observed in the post-intervention cross-sectional survey must be interpreted with caution in the context of limited possibility of causal inference due to the quasi-experimental design, the confounding factors (climatic and seasonal variations, military operations), and the limitations of the study (different duration of pre and post-intervention surveys, different seasonality). Nevertheless this observation is consistent with the decrease described in surveillance data and is strengthened by the interrupted time series analysis showing a drop in exported cases number after the intervention's initiation, which are significantly lower than expected on the bases of preexisting trends and seasonality. Further mathematical modeling with additional sources of data is underway to further refine this analysis using a mathematical SIS model. Furthermore, the significant decrease of asymptomatic carriers and the inversion of the proportion of P. falciparum and P. vivax are typical of malaria elimination contexts [27,28]. We can also expect a spillover of the strategy: i) with a reduction in transmission by people better treated for malaria; ii) by the ‘pro-active case detection’ through the systematic self-RDT performed during training and followed by treatment when positive; iii) and by more appropriate behaviors through the person-to-person dissemination of the information delivered during Malakit training sessions.
4.4. An essential and fruitful subnational collaboration
The project rested on constructive international cooperation, facilitated by the support of the health institutions of the involved countries, and efficient communication between the project partners [10]. This was crucial because the intervention targeted mobile populations between three countries and was implemented at the border staging sites. Despite political, regulatory, geographic or language constraints, this sub-national collaboration has been fruitful and essential to the success of the project.
4.5. Self-diagnosis and self-treatment of malaria: a solution for particular situations
This is the first time that a strategy based on self-diagnosis and self-treatment was implemented on such a large scale, i.e. on a population of approximately 10,000 people, including more than 3,700 participants. Similar strategies have been evaluated in travelers or workers in isolated areas, with stand-by emergency treatment, with or without prior RDT diagnosis, and only three evaluated the use of a self-RDT prior to self-treatment [29,30]. In these, 84% of the RDTs were performed correctly. The proportion was higher when persons had received a pre-training (97%) than without pre-training (90% and 68%) [29]. This was one of the main concerns of our study: to make the training tools understandable and adapted to the gold miner's population. The training lasted an average of 40 minutes, and instructions for using the kit were in the form of videos, drawings and a smartphone application, so that it could be used even by people with little education.
Usually, medical care is based on the relationship between a “knowing” health care professional and the patient, “lay people”, in search of answers and information. The Malakit strategy shifted this paradigm by giving participants the opportunity to be responsible for their own health, i.e. managing the symptoms of malaria. In fact, in the context of gold miners, this was already the case in some ways, with a heavy reliance on UTC drugs. Thus, rather than going against this behavior, it seemed preferable to accompany it and make it more appropriate by providing people with the knowledge and means to do it properly. Hence, Malakit was as a population-based risk-reduction strategy.
The combination of i) the desire of the target population to be as autonomous as possible in their lifestyle; ii) the fact that healthcare cannot be set up closer to this population, and iii) the mobility of the target population passing through strategic points where they can be reached, are the right circumstances in which this self-diagnosis and self-treatment approach may be useful. We believe that populations in other places in the world, such as illegal loggers or other isolated miners with similar characteristics, could benefit from such a strategy, and perhaps also with other diseases, although this strategy cannot replace a medical consultation if it is accessible.
4.6. Next steps
The strategy is now being pursued in Suriname outside the framework of research, carried out by the Ministry of Health. Discussions are underway for the integration in current malaria program tool-box also in France and Brazil. An evolution of the strategy with the addition of a second intervention offering radical treatment of P. vivax for persons at high risk of carrying hypnozoites is being considered to reach the goal of eliminating malaria in the region.
5. Conclusion
RDTs and ACT are key tools to control malaria, and are internationally validated by the WHO but their use in this particular self-diagnosis and self-treatment strategy is unprecedented. With an adapted packaging, relevant training tools, trusted health-mediators and strategic sites to reach the study population, it has shown its value and its potential transferability.
Contributors
MDo, MG, YL, MSM, SV, MN, AA, HH, CP, PM and AS conceived the study. MDo, MG, YL, MSM and SV wrote the protocol. MDo, MG, YL, MSM, LM, SV, JBM and HC implemented the study. MDo performed the analysis, YL and AS verified the underlying data. LM, YL and MDe performed biological exams. MDo, YL and AS wrote the first draft. All authors read and approved the final manuscript.
The authors confirm they had full access to the data in the study and accept responsibility to submit for publication.
Declaration of interests
Any authors declare to have no conflict of interest.
Acknowledgments
Funding
The CHC, as sponsor, directly managed most of the project funds. Half of the funding was by the European Regional Development Fund (FEDER) via the Interregional Amazon Cooperation Program (IACP) 2014-2020 (N° Presage 3949), supplemented with self-funding from the CHC, funds from the French Guiana Regional Health Agency and contributions in kind from the (Global Fund to Fight AIDs, Tuberculosis and Malaria) and the Ministry of Health of Brazil.
The funding bodies have no role in the implementation and analysis of the project.
External Reference
ClinicalTrials.gov
Registration number: NCT03695770
Data sharing
Anonymized data may be shared after a duly justified request to the corresponding author (MDo), given the particularly sensitive nature of these data concerning a population carrying out an activity punishable by law. The study protocol, statistical analysis plan, and informed consent forms are also available from MDo.
Acknowledgments
The authors thank sincerely all the facilitators who patiently and professionally worked in this project, the Centre de Ressources Biologiques Amazonie and the support team of the Centre d'Investigation Clinique. They also thank P. Massat and L. Schmatz from Mavromatika.com for Figures 1 and 3.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lana.2021.100047.
Appendix. Supplementary materials
References
- 1.Douine M, Mosnier E, Le Hingrat Q, Charpentier C, Corlin F, Hureau L, et al. Vol. 18. BMC Public Health; 2017. (Illegal gold miners in French Guiana: a neglected population with poor health). Available from http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4557-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Douine M, Musset L, Corlin F, Pelleau S, Pasquier J, Mutricy L, et al. Prevalence of Plasmodium spp. in illegal gold miners in French Guiana in 2015: a hidden but critical malaria reservoir. Malar J. 2016;15:315. doi: 10.1186/s12936-016-1367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pommier de Santi V, Djossou F, Barthes N, Bogreau H, Hyvert G, Nguyen C, et al. Malaria hyperendemicity and risk for artemisinin resistance among illegal gold miners, French Guiana. Emerg Infect Dis. 2016;22(5):903–906. doi: 10.3201/eid2205.151957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Douine M, Lazrek Y, Blanchet D, Pelleau S, Chanlin R, Corlin F, et al. Predictors of antimalarial self-medication in illegal gold miners in French Guiana: a pathway towards artemisinin resistance. J Antimicrob Chemother. 2018;73(1):231–239. doi: 10.1093/jac/dkx343. [DOI] [PubMed] [Google Scholar]
- 5.Mathieu L, Singh P, Monteiro WM, Magris M, Cox H, Lazrek Y, et al. Kelch13 mutations in Plasmodium falciparum and risk for spreading in Amazon basin countries. J Antimicrob Chemother. 2021 doi: 10.1093/jac/dkab264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wangdi K, Gatton ML, Kelly GC, Clements AC. Cross-border malaria: a major obstacle for malaria elimination. Adv Parasitol. 2015;89:79–107. doi: 10.1016/bs.apar.2015.04.002. Jun. [DOI] [PubMed] [Google Scholar]
- 7.Guyant P, Corbel V, Guérin PJ, Lautissier A, Nosten F, Boyer S, et al. Past and new challenges for malaria control and elimination: the role of operational research for innovation in designing interventions. Malar J. 2015;14 doi: 10.1186/s12936-015-0802-4. Jul 17. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4504133/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. WHO | Global Technical Strategy for Malaria 2016-2030. 2016. Available from: http://www.who.int/malaria/areas/global_technical_strategy/en/
- 9.Douine M, Sanna A, Galindo M, Musset L, Pommier de Santi V, Marchesini P, et al. Malakit: an innovative pilot project to self-diagnose and self-treat malaria among illegal gold miners in the Guiana Shield. Malar J. 2018;17(1):158. doi: 10.1186/s12936-018-2306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galindo MS, Lambert Y, Mutricy L, Garancher L, Bordalo Miller J, Gomes JH, et al. Setting-up a cross-border action-research project to control malaria in remote areas of the Amazon: describing the birth and milestones of a complex international project (Malakit) Malar J. 2021;20(1):216. doi: 10.1186/s12936-021-03748-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ip S, Paulus JK, Balk EM, Dahabreh IJ, Avendano EE, Lau J. Agency for Healthcare Research and Quality (US); 2013. Role of single group studies in agency for healthcare research and quality comparative effectiveness reviews. Available from https://www.ncbi.nlm.nih.gov/books/NBK121317/ [PubMed] [Google Scholar]
- 12.Lambert Y, Galindo MS, Suarez-Mutis MC, Mutricy L, Sanna A, Garancher L, et al. Tailoring Mobile Data collection for intervention research in a challenging context: development and implementation in the Malakit study. JMIR Prepr. Available from: https://preprints.jmir.org/preprint/29856 [DOI] [PMC free article] [PubMed]
- 13.Le Tourneau F-M. CNRS Editions; 2020. Chercheurs d'or - L'orpaillage clandestin en Guyane française.https://livre.fnac.com/a14373370/FRANCOIS-MICHEL-LE-TOURNEAU-Chercheurs-d-or-L-orpaillage-clandestin-en-Guyane-francaise 426 p. Available from. [Google Scholar]
- 14.Mosnier E, Garancher L, Galindo M, Djossou F, Moriceau O, Mutricy L, et al. Paludisme en Guyane: des projets de recherche opérationnelle originaux s'appuyant sur la santé communautaire. Lett Infect. 2020;35(2):50–78. [Google Scholar]
- 15.Shokoples SE, Ndao M, Kowalewska-Grochowska K, Yanow SK. Multiplexed real-time PCR assay for discrimination of Plasmodium species with improved sensitivity for mixed infections. J Clin Microbiol. 2009;47(4):975–980. doi: 10.1128/JCM.01858-08. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haute Autorité de santé . Haute Autorité de Santé; 2007. Méthodes quantitatives pour évaluer les interventions visant à améliorer les pratiques. [Google Scholar]
- 18.Sandfort M, Vantaux A, Kim S, Obadia T, Pepey A, Gardais S, et al. Forest malaria in Cambodia: the occupational and spatial clustering of Plasmodium vivax and Plasmodium falciparum infection risk in a cross-sectional survey in Mondulkiri province. Cambodia. Malar J. 2020;19(1):413. doi: 10.1186/s12936-020-03482-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Landier J, Parker DM, Thu AM, Lwin KM, Delmas G, Nosten FH, et al. Effect of generalised access to early diagnosis and treatment and targeted mass drug administration on Plasmodium falciparum malaria in Eastern Myanmar: an observational study of a regional elimination programme. The Lancet. 2018;391(10133):1916–1926. doi: 10.1016/S0140-6736(18)30792-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galatas B, Saúte F, Martí-Soler H, Guinovart C, Nhamussua L, Simone W, Ashley EA, et al. A multiphase program for malaria elimination in southern Mozambique (the Magude project): A before-after study. PLOS Med. 2020;17(8) doi: 10.1371/journal.pmed.1003227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parent A-A, Galindo MS, Lambert Y, Douine M. Maliqua: A study within Malakit, a project on malaria and gold miners in French Guiana. medRxiv. 2021 2021.05.16.21257287. [Google Scholar]
- 22.Bruxvoort K, Goodman C, Kachur SP, Schellenberg D. How Patients Take Malaria Treatment: A Systematic Review of the Literature on Adherence to Antimalarial Drugs. PLOS ONE. 2014;9(1):e84555. doi: 10.1371/journal.pone.0084555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hiwat H, Martínez-López B, Cairo H, Hardjopawiro L, Boerleider A, Duarte EC, et al. Malaria epidemiology in Suriname from 2000 to 2016: trends, opportunities and challenges for elimination. Malar J. 2018;17(1):418. doi: 10.1186/s12936-018-2570-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Malaria Programme of Suriname. Cases by transmission area and malaria type. Suriname. 2020 [Google Scholar]
- 25.Ministério da Saude. Brasilia: Secretaria de Vigilância en Saude -SVS; 2019. Malária nas fronteiras e importada de outros países [Internet] Available fromhttps://public.tableau.com/profile/mal.ria.brasil#!/vizhome/Mini_fronteira_1719/Painelpas. [Google Scholar]
- 26.da Cruz Franco V, Peiter PC, Carvajal-Cortés JJ, Dos Santos Pereira R, Mendonça Gomes M, Suárez-Mutis M. Complex malaria epidemiology in an international border area between Brazil and French Guiana: challenges for elimination. Trop Med Health. 2019;47 doi: 10.1186/s41182-019-0150-0. 24–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lover AA, Baird JK, Gosling R, Price RN. Malaria Elimination: Time to Target All Species. Am J Trop Med Hyg. 2018;99(1):17–23. doi: 10.4269/ajtmh.17-0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chhim S, Piola P, Housen T, Herbreteau V, Tol B. Malaria in Cambodia: A Retrospective Analysis of a Changing Epidemiology. Int J Environ Res Public Health. 2021;18(4) doi: 10.3390/ijerph18041960. 2006-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Utzinger KS, Held U, Hanscheid T, Gültekin N, Fehr J, Grobusch MP, et al. Self-diagnosis and self-treatment of Plasmodium spp. infection by travellers (1989–2019): A systematic review and meta-analysis. Travel Med Infect Dis. 2020;38 doi: 10.1016/j.tmaid.2020.101902. [DOI] [PubMed] [Google Scholar]
- 30.Roukens AH, Berg J, Barbey A, Visser LG. Performance of self-diagnosis and standby treatment of malaria in international oilfield service employees in the field. Malar J. 2008 Jul 14;7(1):128. doi: 10.1186/1475-2875-7-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.