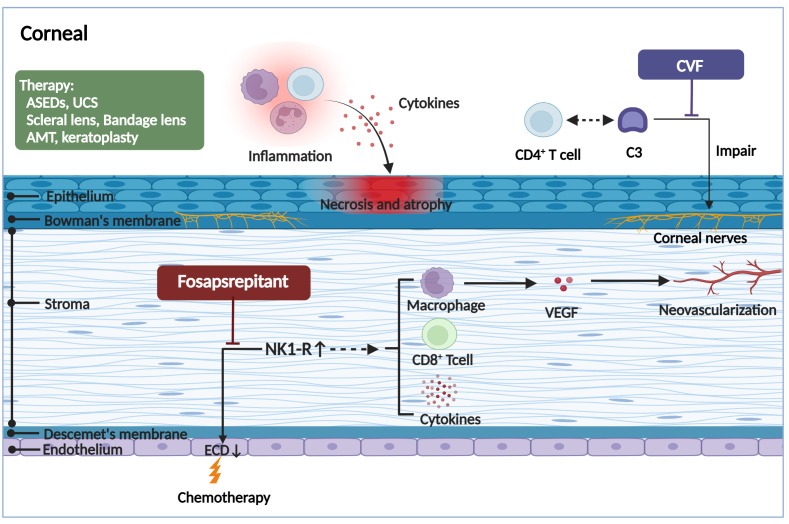
Figure 3.
The pathogenic mechanism in the corneal of ocular GVHD and treatment. The corneal may appear the corneal epithelial impairment, a lower endothelial cell density, hemangiogenesis, and corneal neurosensory abnormalities in ocular GVHD. The corneal epithelial impairment including atrophy and necrosis, the vacuolization of epithelial basal cells, and stromal edema, all of which are likely associated with the infiltration of immune cells and the stimulation of inflammatory cytokines. The reduction of the corneal endothelial cells and formation of neovascularization might be associated with increased expression of the proinflammatory marker NK1R. Fosaprepitant, the inhibition of the SP-NKR1 axis, through topically applied substantially ameliorated the clinical manifestations of ocular GVHD. In addition, the aberrant complement C3/CD4+ T-cell axis activation might coordinate corneal nerve damage. However, the specific mechanism needs to be further investigated. By forming a biochemically stable convertase to rapidly hydrolyze mammalian C3, localized cobra venom factor prevents corneal sensation loss in ocular GVHD. In addition, the therapies for ocular GVHD patients with severe corneal impairment include serum eye drops, umbilical cord serum, scleral lenses, bandage soft contact lenses, amniotic membrane grafts, and keratoplasty. ASEDs, autologous serum eye drops; UCS, umbilical cord serum; AMT, amniotic membrane graft; CVF, cobra venom factor; ECD, endothelial cell density; NK1R, neurokinin-1 receptor; VEGF, vascular endothelial growth factor. (Created with BioRender.com).