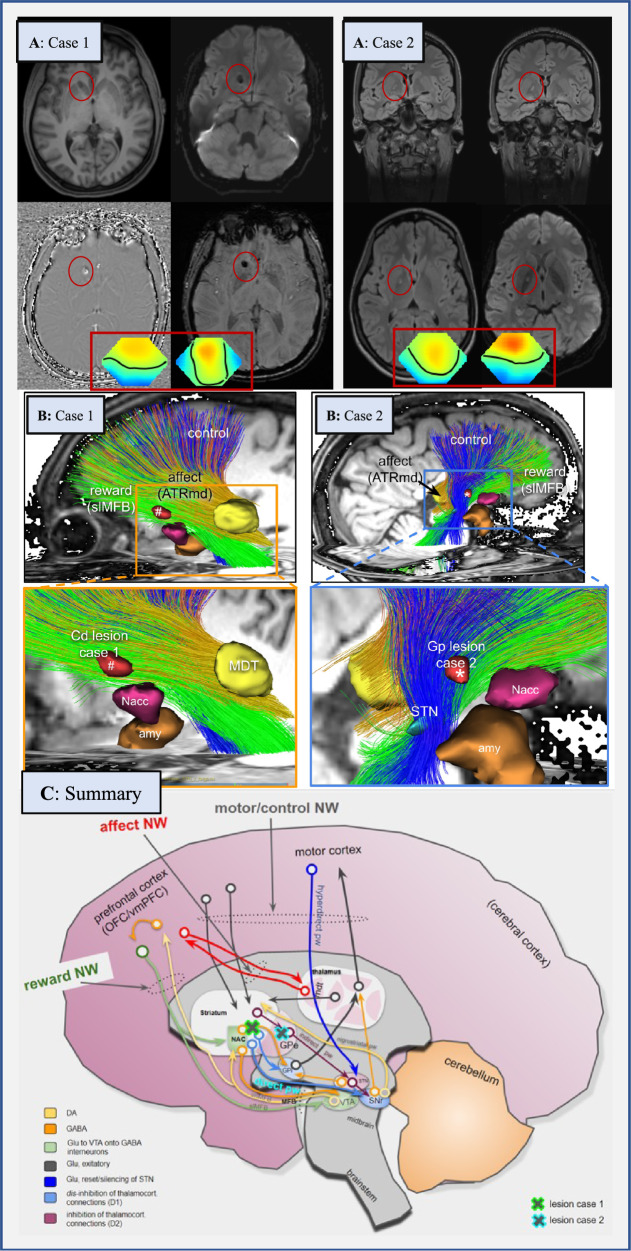
Fig. 1. Neuroimaging findings in both patients (A, B) and conceptual considerations (C).
A: Case 1 shows a lesion in the right caudate nucleus with a size of 8.9 × 5 mm. The lesion was classified as a probable microbleeding, but calcification as a late consequence of microbleeding could not be definitively ruled out. Case 2 presents with a FLAIR-hyperintense lesion in the globus pallidus on the right (defect with a gliotic rim in the direction of a lenticulostriate vessel). Because Case 2 had febrile seizures during her first decade, and since then chronic obsessive-compulsive disorder (OCD), a post-inflammatory origin could be plausible. Framed below in red are the topographies of the prominent theta electroencephalography (EEG) components for the two patients. In both cases the pronounced frontocentral theta activity is suggestive of sleepiness. Topographies are against common average reference with standard orientation (top = front), positive excursions in red, negative in blue. Zero potential is indicated by a black line. Spontaneous EEG was recorded during a 12-minute series of standard maneuvers (eyes open, eyes closed, and hyperventilation) according to the 10–20 system (21 head channels), leading to 21 independent component analysis (ICA) components. Artifact-free sections across the whole recording length were submitted to ICA training. ICA maps as well as associated EEG time courses were reviewed and components classified by their topography, reaction to the maneuvers, and spectrum. Additionally, intermittent rhythmic delta/theta activity was detected in the artifact-free sections using an automated algorithm. The software used for these analyses is a combination of the EEG data processor “avg_q” (https://github.com/berndf/avg_q) and custom python scripts. B: Case 1 has tractographic rendition of streamlines involved in strategic unilateral lesions in the inferior and anterior caudate nucleus (nucleus accumbens spared) (#, right side). Tractographic analysis of Case 2 shows a pallidal lesion (*) involving the “motor-control network” (blue fibers). C: Interplay of three involved networks (“affect, control, and reward network”) within the whole “OCD framework” (existing of the “affect, control, reward, and default-mode network” [2, 13]) at distinct network hubs (taken and altered from [13]). The locations of lesions in Cases 1 and 2 are shown as green/blue crosses. Abbreviations: Amy amygdala, ATR anterior thalamic radiation, ATRmd anterior thalamic radiation from dorsomedial thalamus, BNST bed nucleus of stria terminalis, Cd caudate nucleus, DA dopamine, EEG electroencephalography, GABA gamma-aminobutyric acid, GPe globus pallidus externus, GPi globus pallidus internus, Glu glutamate, imMFB infero-medial MFB, ICA independent component analysis, MDT mediodorsal thalamus, MFB medial forebrain bundle, NAC/Nacc nucleus accumbens, NW network, OCD obsessive-compulsive disorder, OFC orbitofrontal cortex, pw pathway, slMFB superolateral branch of the medial forebrain bundleMFB, SNr substantia nigra, STN subthalamic nucleus, VTA ventral tegmental area, vmPFC ventromedial prefrontal cortex.