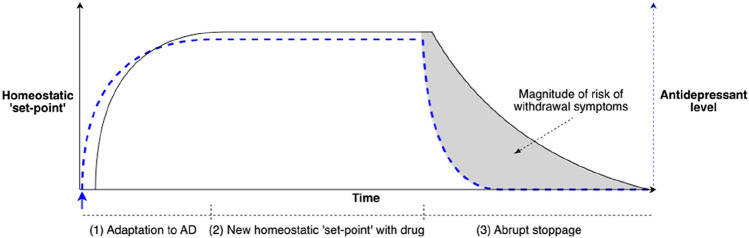
Fig. 1.
Conceptual model of the neurobiology of antidepressant withdrawal. In this diagram, the homeostatic ‘set-point’ is shown in black and antidepressant (AD) drug concentrations are shown in blue dotted lines [77]. (1) The system is at baseline. At the blue arrow, an antidepressant is administered; drug plasma concentrations increase. Physiological adaptations of the system to the presence of the drug begin (which may be the period for which ‘start-up side effects’ are most pronounced). (2) At the plateau, drug plasma concentrations (and target receptor activation) have reached a steady state with a new homeostatic set-point of the system established (‘start-up side effects’ may reduce). (3) The antidepressant is abruptly ceased and plasma drug concentrations drop to zero (exponentially, according to the elimination half-life of the drug). This difference between the homeostatic set point (the ‘expectations’ of the system) and the concentration of drug in the system (dotted blue line) is experienced as withdrawal symptoms. The duration of withdrawal symptoms is largely determined by the time required for adaptations to the drug to resolve. Hence, withdrawal symptoms may worsen or peak even long after the drug has been eliminated from the system. The shaded area under the curve, representing the difference between the homeostatic set-point and the concentration of the drug, indicates the degree of risk of withdrawal symptoms: the larger the area the greater the risk. The greater the departure of drug concentration from the homeostatic set-point, the greater the risk.
Adapted, with permission, from [77]