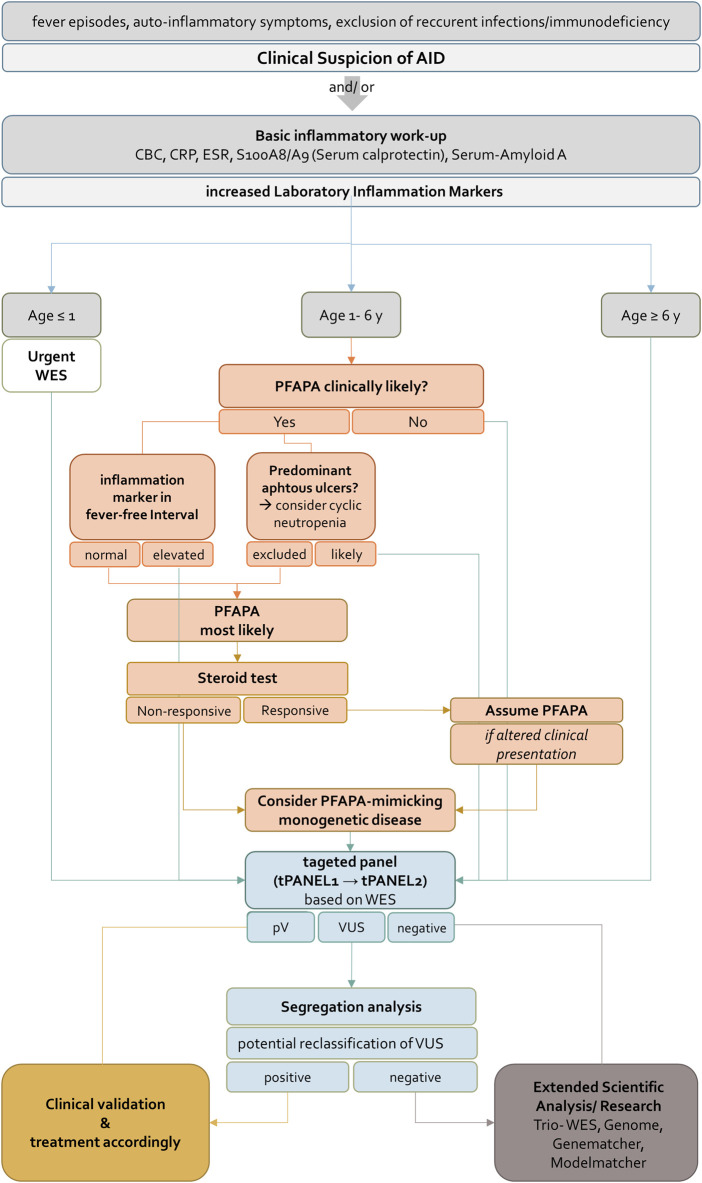
FIGURE 5.
Flowchart for diagnosis, treatment and genetic evaluation of patients with suspected AID. AID should be suspected if patients present with fever episodes and auto-inflammatory signs and symptoms. If CBC, CRP, ESR, S100A8/A9 (Serum calprotectin) and Serum-Amyloid A are increased the further approach depends on the age of the patient. For patients younger than 1 year or older than 6 years WES should be requested immediately. According to clinical guidelines patients between one and 6 years PFAPA syndrome should be ruled out in a first step. If inflammation markers in fever-free intervals are not elevated and cyclic neutropenia is excluded in patients with oral ulcers, PFAPA syndrome is most likely. A response to a steroid test confirms the diagnosis. A non-responsive steroid test indicates a PFAPA-mimicking monogenetic disease and WES should be performed. For all children identification of pathogenic variant(s) in tPANEL entails clinical validation and treatment according to the disease. For negative sequencing results an extended scientific analysis (e.g. Trio- WES, Genome, analysis of genes of uncertain significance) is recommended. Variants of unknown significance can be further evaluated by segregation analysis. Confirmation of variants as having arisen de novo may result in reclassification under ACMG guidelines. AID, autoinflammatory disease, CBC, complete blood count, CRP, C-reactive protein, ESR, erythrocyte sedimentation rate, WES, whole exome sequencing, PFAPA, Periodic Fever, Aphthous Stomatitis, Pharyngitis, Adenitis, pV, pathogenic variant, VUS, Variant of unknown significance.