Abstract
Aim
The aim of the study was to develop an evidence‐based care bundle protocol for preventing falls in hospitalized children.
Design
Delphi method.
Methods
Based on the four basic concepts of nursing, the theoretical dimension and item pool of the care bundle first draft were constructed by searching evidence and referring to the care bundle for preventing inpatient fall issues by the China Nursing Quality Promotion Alliance. The Delphi method and trial tests were used to select and adjust items of the care bundle to form the care bundle protocol for preventing falls in hospitalized children.
Results
The first draft care bundle for preventing falls in hospitalized children included 4 dimensions and 21 items. In the 2‐round Delphi study, one item was removed, and three items were adjusted. One item was adjusted by trial test. Finally, the care bundle protocol for preventing falls in hospitalized children consisted of 4 dimensions and 20 items.
Keywords: care bundle, Delphi study, fall prevention, paediatrics
1. INTRODUCTION
Falls are the most common type of adverse events reported for hospitalized children (Alemdaroglu et al., 2017; Fujita et al., 2013; Lee et al., 2013), which can cause serious harm to paediatric patients (AlSowailmi et al., 2018; Feuerlicht et al., 2020; Kim & Lee, 2021), and increase the length of stay (Almis et al., 2017). As a result, falls of inpatient children are an important issue as part of initiatives to prevent inpatient safety accidents (Kim, Lim, et al., 2021).
There is no unified nursing practice standard for preventing falls in hospitalized children in China. In September 2018, the China Nursing Quality Promotion Alliance (CNQPA) (2018) issued a care bundle to prevent falls in hospitalized patients. However, the care bundle is mainly for adults and is not applicable to hospitalized children. Although a large number of studies on the prevention of falls in hospitalized children have been reported in China, and strategies such as the PDCA cycle model and multimodal health education have been used to reduce the fall rate, the relevant strategies have only been implemented in the investigator′s hospital, and the accuracy of the results remains to be considered (Guo et al., 2020). Furthermore, many nursing practices are not based on the best evidence but on clinical experience (Long, 2018). There are few researches on care bundles for preventing falls in hospitalized children in China (He et al., 2016), and there are some problems, such as misunderstandings of comprehensive nursing measures for care bundles, failing to explain whether the intervention measures are derived from evidence and neglecting that the care bundle should be based on evidence‐based essence (Liu & Shang, 2021; Wu & Hu, 2013; Xiao et al., 2021). “The kit: Closing the gap: from evidence to action,” published by ICN in 2012 (International Council of Nurses, 2012) pointed out that clinical decision‐making not based on the best evidence may introduce variability into nursing practice, leading to inefficient and ineffective nursing practice.
Therefore, the purpose of this study is to develop an evidence‐based care bundle protocol for preventing falls in hospitalized children, which would provide practice standards for nurses to implement nursing practice of preventing falls in hospitalized children and would provide a basis for nursing quality management to prevent falls in hospitalized children.
2. BACKGROUND
A fall is “a sudden, unintentional descent, with or without injury to the patient that results in the patient coming to rest on the floor, on or against some other surface, on another person, or an object” (National Database of Nursing Quality Indicators (NDNQI), 2020). Studies have shown that the risk factors for falls in hospitalized children are multifaceted (AlSowailmi et al., 2018; Parker et al., 2020; Kim & Lee, 2021) and comprehensive multifaceted intervention measures should be taken (Liu & Shang, 2021; Sheppard‐Law et al., 2022). At present, the nursing measures to prevent falls in hospitalized children mainly include fall risk assessment, using the high‐risk sign/sticker, close observation, assistance during children′s ambulation, family and staff education, composition of a safe environment and never leaving the child alone (Kim, Kim, & Lim, 2021).
Evidence‐based fall prevention care for hospitalized children is constantly updated in practice. Murray et al. (2016) implemented an evidence‐based fall prevention nursing intervention strategy for hospitalized children. The Intervention strategy included the use of a validated fall risk assessment tool, family and patient education, signs identifying that patient as high risk for falls, orientation to the unit, environmental safety, patient rounding hourly (if high risk). During the 6‐month intervention period, the incidence of falls per 1,000 days in the hospital decreased from 4.5% to 0%. An interprofessional team (Benning & Webb, 2019) designed and implemented a SPS evidence‐based falls bundle, which included selection and implementation of a fall risk assessment tool, implementation of fall bundle elements and implementation of fall prevention education to patients and families. After implementation, the falls bundle, fall bundle compliance increased from 27% to 88%, and there were zero patient falls in five out of the 6 months. In addition, the JBI Nursing Evidence Network released a recommended practice (The Joanna Briggs Institute (JBI), 2017) and a summary of evidence on preventing falls in paediatric patients (Obeid, 2017) in 2017. The evidence summary was based on a structured search of the literature and selected evidence‐based healthcare databases. Both the recommended practice and the evidence summary summarized the best available evidence for fall prevention in children, including assessment, risk factors and interventions/preventive measures. Related research on fall prevention nursing by foreign scholars can provide a good reference for nurses to carry out nursing intervention research on preventing falls in hospitalized children in China. However, due to the large differences in the medical environment and cultural concepts at home and abroad, whether it is applicable to China requires further exploration by researchers.
Research on care bundles for preventing falls in hospitalized children in China is in the exploratory stage. Some studies (Ding, 2016; Yi et al., 2018) have tried to use care bundles to prevent falls in hospitalized children but have failed to explain and demonstrate the basis of the measures (Wu & Hu, 2013), have ignored the essence of evidence‐based construction of care bundles, and have mistaken the “summary of nursing measures” for care bundles (Liu & Shang, 2021; Xiao et al., 2021). Therefore, the question to be explored in this study is: What is included in the evidence‐based care bundle for preventing falls in hospitalized children suitable for the Chinese nursing situation? Is it scientific and feasible?
3. METHOD
3.1. Design
The care bundle protocol for preventing falls of hospitalized children was formed by searching the evidence, developing a theoretical framework, the Delphi method and a trial test. The first phase combined the latest evidence on the prevention of falls in hospitalized children, obtained from the evidence search, with the care bundle for preventing falls in hospitalized patients (CNQPA, 2018), based on the item pool of the four basic nursing conceptual framework (Fawcett, 1984), the first draft of the care bundle for preventing falls in hospitalized children was formed. The second phase used two‐round Delphi study to collect expert opinions and revise the items to form the care bundle review draft for preventing falls of hospitalized children. The third phase conducted a trial test to adjust the items, forming a care bundle protocol for preventing falls in hospitalized children.
The Delphi method was used as a method for consensus‐building in this study (Humphrey‐Murto et al., 2017). It is an iterative process using a number of surveys, in which researchers seek expert consensus to answer a question (McPherson et al., 2018). A two‐round electronic Delphi method were used to access relevant experts across multiple regions of China to establish a consensus on the prevention of falls in hospitalized children. This study complied with the Conducting and Reporting DElphi Studies (CREDES) checklist.
3.2. Evidence search
The searched databases included Cochrane, OVID, PubMed, JBI, RNAO and NGC, and the search terms were “fall OR falls OR falling OR tumble OR tumbling OR tumbles” AND “pediatrics OR kids OR child OR children.” Subject terms were used to search and trace references when necessary. The inclusion criteria were (1) hospitalized children; (2) studies written in English; (3) studies published within 5 years; and (4) literature types included systematic reviews, practice guidelines and summaries of evidence. Through the search, we obtained one recommended practice recommendation for preventing falls in paediatric patients (JBI, 2017) and one summary of evidence to prevent falls in paediatric patients (Obeid, 2017), published by JBI in 2017.
3.3. Theoretical framework
Nursing′s metaparadigm defines the basis of nursing′s work as focused on the human, environment, health and care (Fawcett, 1984). Over the years, the interrelations among the four basic concepts endure as a guiding framework for nursing practice and research (Bender, 2018). Scholars also suggested that Fawcett (1984) metaparadigm of nursing should be used as the foundation for nursing and the multidisciplinary team identification and prevention for falls (Guillaume et al., 2016).
In this study, taking the four basic concepts of nursing (Fawcett, 1984)—human, environment, health and care—as the theoretical framework, a four‐dimensional candidate item pool was formed, combined with the searched evidence on preventing falls in hospitalized children and the care bundle to prevent falls in inpatients (CNQPA, 2018). Till then, the first care bundle draft for preventing falls in hospitalized children was formed.
3.4. Delphi study
The Delphi study was used to select and adjust items of the first care bundle draft between November and December 2018. The inclusion criteria of consulting experts were as follows: more than 10 years of experience in paediatric clinical nursing, paediatric nursing education or nursing management; bachelor′s degree or above; intermediate professional titles or above; and willingness to participate in this study. The number of experts and survey rounds can vary according to the purpose of the study (McPherson et al., 2018). Generally, it is advisable to be around 8–20 experts (Xu, 2016). A total of 19 experts from 13 tertiary grade A hospitals in seven province regions of Beijing, Shanghai, Shandong, Shaanxi, Chongqing, Anhui and Fujian were recruited for this study.
The Delphi consulting questionnaire includes 4 parts. (1) Foreword: introduce the background, purpose and content of the research, the questionnaire completion instructions and the response time of the questionnaire. (2) Main body: the first draft of the care bundle for preventing falls in hospitalized children. The experts were asked to rate scores for the importance and feasibility of each item using the Likert 5‐level scoring method (1‐Not important to 5‐very important, 1‐Not feasible to 5‐very feasible). “Supplement and Modification Opinions” were also included so that experts could write their suggestions and opinions about the care bundle. (3) Basic information of experts: including age, major, working years, education background and professional title. (4) Experts' familiarity and judgement basis questionnaire: Experts were asked to evaluate their familiarity using a 5‐point Likert scale of 0.2, 0.4, 0.6, 0.8 and 1.0 (0.2‐Not familiar to 1.0‐Very familiar). The judgement basis includes four aspects: theoretical analysis, working experience, peer understanding and self‐intuition. The criteria′s influence degrees and score assignments include theoretical analysis (great‐0.3; medium‐0.2; small‐0.1), working experience (great‐0.5, medium‐0.4, small‐0.3), peer understanding (great‐0.1, medium‐0.1, small‐0.05) and self‐intuition (great‐0.1, medium‐0.1, small‐0.05). The consulting questionnaires were sent via e‐mail. Before the next round, some items were revised based on the opinions and scores of the experts in the first round. In the next round, updated consulting questionnaires were sent to the experts. The consultation was repeated until the opinions of experts were essentially consistent, and the care bundle review draft for preventing falls in hospitalized children was formed.
3.5. Trial test
A trial test was conducted to initially assess the feasibility and acceptability of the care bundle review draft for preventing falls in hospitalized children in January 2019. A 26‐bed paediatric ward in a tertiary hospital in Fujian, China, was the setting for the trial test. After obtaining the consent of the hospital, the researchers contacted the director of the hospital′s nursing department and the head nurse of the paediatric ward to inform them about the study and obtain support for the trial test. The paediatric ward treats children aged 28 days to 14 years, with 100 inpatient admissions per month. Participants with <24 hr of admission or whose parents did not consent to participate in the study were excluded.
Nurses' inclusion criteria were as follows: (1) engaged in direct care, (2) certified as Registered Nurses, (3) volunteering to participate in the study. Excluded criteria were on leave or resigned during the study. There were 10 nurses working in the paediatric ward participated in this study. The nurses had more than 3 years of paediatric nursing experience, with an education level of college or above and research experience.
Ten Registered Nurses working in the ward were given special training about their knowledge of fall prevention. Two training sessions with the same content were held in 2 days for nurses to attend on their own schedule. The training took about 1 hr by holding department business learning lectures, using PPT to explain and pushing courseware to the WeChat (a social software widely used in China) group. The lectures covered topics from basic knowledge of falls in hospitalized children, risk factors of hospitalized children falling, the content and specific implementation methods of the review draft for preventing falls in hospitalized children, introduction and usage of fall assessment tool for hospitalized children. For item D1 in the bundle, in the current study we used a validated risk assessment tool: the Humpty Dumpty Falls Scale (HDFS), with the cut‐off score of 12 (Hill‐Rodriguez et al., 2009; Messmer et al., 2013). During the training, the nurses also shared their own experience and communicated with each other about the problems they might encounter in the practical process. If there are nurses who cannot fully understand the training content, we will plan to schedule additional small lectures. In fact, the lecture was very easy to digest by giving vivid examples to illustrate the key points of hospitalized children falling prevention. One week later after the training, all the nurses passed the written examination on knowledge about preventing falls in hospitalized children and then started the trial test.
The nurses used the care bundle checklist to implement and record the care bundle for preventing falls and incorporated the implementation status of the care bundle into the content of the shift. The head nurse used the care bundle checklist to supervise nurses' compliance with the care bundle twice a week to urge nurses to implement the care bundle in a standardized manner. The head nurse found the doubts and problems of the nurses in the implementation process in time through supervision, resolved them and summarized the feedback to the nurses through morning meetings and WeChat every week.
Researchers used care bundle checklists to evaluate nurses' compliance with the care bundle to prevent falls in hospitalized children. The care bundle checklist was developed by the researchers based on the review draft of the care bundle. After each measure, its completion was judged as yes or no, and the data on compliance with the care bundle were collected 24–72 hr after the trial test objects were admitted to the hospital. In addition, before the end of the trial, the researchers distributed opinion forms to nurses to collect their feedback and suggestions on the trial test.
3.6. Data analysis
The data were double‐entered and checked for consistency by EpiData3.1 first and were then analysed using SPSS V.25.0. Descriptive analysis of general data was represented by frequency and composition ratio; when describing statistical results, counting data are represented by percentage (%), and measurement data are represented by mean ± standard deviation (−X ± S). The representativeness and reliability of expert consultation are represented by coordination degree, concentration, coefficient of variation, effective response rate and authority coefficient.
3.7. Ethical consideration
This study was approved by the Ethics Committee of Fujian Provincial hospital (no.K2018‐12‐039). Data collection instruments for two rounds of the Delphi study included a statement describing the purpose of the research and that completing the questionnaire implied consent. The nurses did not sign an informed consent form due to the low‐risk nature of study. Also, verbal and written consent was obtained by providing information to patients' guardians about the purpose of the study.
4. RESULTS
4.1. Evidence search results
One piece of evidence summary on preventing paediatric patient falls was obtained through literature search, combined with the care bundle for preventing inpatient falls (CNQPA, 2018) and according to the four basic concepts of nursing (Fawcett, 1984), the care bundle first draft for preventing falls in hospitalized children with 4 dimensions and 21 items was formed, including 17 general preventive measures and 4 specific preventive measures for children at high risk of falls (Figure 1, Table 1).
FIGURE 1.
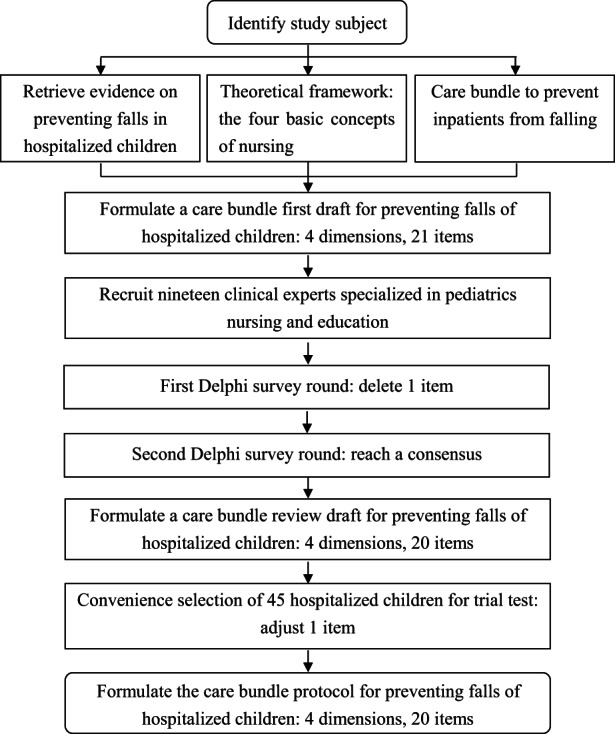
Flow chart of care bundle protocol construction
TABLE 1.
First draft of the care bundle for preventing falls in hospitalized children
| Dimensions | Items | Evidence level |
|---|---|---|
|
A Human |
|
IV |
|
IV | |
|
IV | |
|
IV | |
|
B Environment |
|
IV |
| IV | ||
|
IV | |
|
IV | |
|
IV | |
|
IV | |
|
IV | |
|
IV | |
|
C Health |
|
IV |
|
III | |
|
IV | |
|
D Care |
|
IV |
|
IV | |
|
IV | |
|
IV | |
|
IV | |
|
IV | |
|
IV |
Specific preventive measures for children at high risk of falling.
4.2. Delphi study results
4.2.1. Basic information of the experts
A total of 19 qualified experts from 13 tertiary A hospitals in seven provinces and cities in China were invited to participate in this study (Figure 1). Among them, there were 17 experts in paediatric nursing management, 1 expert in paediatric nursing education and 1 expert in paediatric clinical nursing. The oldest was 56 years old, the youngest 31 years old, and the average age was 46.5 years old. The longest working years of nursing was 37 years, while the shortest was 11 years, with an average of 25.5 years. All had a bachelor′s degree or above. Five experts had intermediate professional titles and 14 experts had senior professional titles.
4.2.2. Effective response rate, authority and coordination
Two rounds of the Delphi survey were conducted in this study, and the effective response rates of the Delphi survey rounds were 100%. In the first round, three experts put forward constructive opinions, accounting for 16%. The authority coefficients of the Delphi survey rounds were 0.891 and 0.877, respectively. In the first round, Kendall′s coefficients of concordance on the importance and feasibility were 0.287 (p < .01) and 0.269 (p < .01), respectively. Kendall′s coefficients of concordance on the importance and feasibility in the second round were 0.231 (p < .01) and 0.281 (p < .01), respectively (Table 2).
TABLE 2.
Coordination degrees of experts' opinions
| Importance | Feasibility | |||||||
|---|---|---|---|---|---|---|---|---|
| W | X 2 | df | p | W | X 2 | df | p | |
| 1st round | 0.287 | 108.940 | 20 | 0.000 | 0.269 | 102.116 | 20 | 0.000 |
| 2nd round | 0.231 | 83.266 | 19 | 0.000 | 0.281 | 101.538 | 19 | 0.000 |
4.2.3. Concentrations and coefficients of variation
In the first round, the mean values of the importance of experts' opinions ranged from 3.53–4.95, the coefficients of variation ranged from 0.05–0.28, the mean of feasibility evaluations ranged from 3.79–4.95, and the coefficients of variation ranged from 0.05–0.24 (Table 3). Item A2 was deleted because of great heterogeneity in experts' importance rate scores (CV > 0.25). Furthermore, some experts suggested that some items of the scale were unclear or difficult to implement. Therefore, some items were revised according to the experts' suggestions. Item A1 was revised to “Children at high risk are identified (label on ID bands, hang sign and so on).” Item B1 was revised to “Keep the door to the room open for children at high risk of falls when necessary.” Change item D3 to “Wards have nursing protocols for preventing hospitalized children from falling in place.” As a result, the revised consulting questionnaire contained 4 dimensions and 20 items before the second round (Figure 1).
TABLE 3.
Concentrations and coefficients of variation of experts' opinions in the 1st round
| Items | Importance | Feasibility | |||||
|---|---|---|---|---|---|---|---|
|
|
S | CV |
|
S | CV | ||
| A1 | 4.68 | 0.75 | 0.16 | 4.84 | 0.37 | 0.08 | |
| A2 a | 4.00 | 1.11 | 0.28 | 3.89 | 0.94 | 0.24 | |
| A3 | 4.95 | 0.23 | 0.05 | 4.95 | 0.23 | 0.05 | |
| A4 | 4.58 | 0.69 | 0.15 | 4.37 | 0.83 | 0.19 | |
| B1 | 3.53 | 0.84 | 0.24 | 3.79 | 0.92 | 0.24 | |
| B2 | 4.21 | 0.86 | 0.20 | 4.32 | 0.75 | 0.17 | |
| B3 | 4.42 | 0.61 | 0.14 | 4.00 | 0.75 | 0.19 | |
| B4 | 4.79 | 0.54 | 0.11 | 4.79 | 0.42 | 0.09 | |
| B5 | 4.89 | 0.32 | 0.06 | 4.58 | 0.69 | 0.15 | |
| B6 | 4.79 | 0.42 | 0.09 | 4.89 | 0.32 | 0.06 | |
| B7 | 4.79 | 0.42 | 0.09 | 4.63 | 0.50 | 0.11 | |
| C1 | 4.47 | 0.61 | 0.14 | 4.79 | 0.42 | 0.09 | |
| C2 | 4.89 | 0.32 | 0.06 | 4.74 | 0.56 | 0.12 | |
| C3 | 4.26 | 0.65 | 0.15 | 4.16 | 0.83 | 0.20 | |
| D1 | 4.63 | 0.60 | 0.13 | 4.74 | 0.56 | 0.12 | |
| D2 | 4.79 | 0.42 | 0.09 | 4.63 | 0.68 | 0.15 | |
| D3 | 4.84 | 0.38 | 0.08 | 4.63 | 0.50 | 0.11 | |
| D4 | 4.84 | 0.38 | 0.08 | 4.63 | 0.60 | 0.13 | |
| D5 | 4.63 | 0.68 | 0.15 | 4.05 | 0.97 | 0.24 | |
| D6 | 4.74 | 0.45 | 0.10 | 4.21 | 0.71 | 0.17 | |
| D7 | 4.68 | 0.48 | 0.10 | 4.63 | 0.60 | 0.13 | |
Indicators that do not meet the screening criteria.
In the second round, the mean values of the importance of experts' opinions ranged from 4.16–5.00, the coefficients of variation ranged from 0.00–0.20, the mean values of feasibility evaluation ranged from 3.74–4.95, and the coefficients of variation ranged from 0.05–0.25 (Table 4). There was no major difference in expert opinions, and the opinions were essentially consistent, forming a care bundle review draft for preventing hospitalized children from falling. There were a total of 20 items, including 17 general preventive measures and 3 specific preventive measures for children at high risk of falling (Figure 1, Table 5).
TABLE 4.
Concentrations and coefficients of variation of experts' opinions in the 2nd round
| Items | Importance | Feasibility | ||||
|---|---|---|---|---|---|---|
| − X | S | CV | − X | S | CV | |
| A1 | 4.53 | 0.77 | 0.17 | 4.84 | 0.37 | 0.08 |
| A3 | 5.00 | 0.00 | 0.00 | 4.95 | 0.23 | 0.05 |
| A4 | 4.37 | 0.68 | 0.16 | 4.37 | 0.83 | 0.19 |
| B1 | 4.16 | 0.83 | 0.20 | 3.74 | 0.93 | 0.25 |
| B2 | 4.47 | 0.61 | 0.14 | 4.26 | 0.73 | 0.17 |
| B3 | 4.16 | 0.76 | 0.18 | 3.95 | 0.91 | 0.23 |
| B4 | 4.79 | 0.54 | 0.11 | 4.84 | 0.37 | 0.08 |
| B5 | 4.89 | 0.32 | 0.06 | 4.63 | 0.68 | 0.15 |
| B6 | 4.74 | 0.45 | 0.10 | 4.84 | 0.37 | 0.08 |
| B7 | 4.68 | 0.48 | 0.10 | 4.58 | 0.51 | 0.11 |
| C1 | 4.42 | 0.69 | 0.16 | 4.89 | 0.32 | 0.06 |
| C2 | 4.95 | 0.23 | 0.05 | 4.68 | 0.67 | 0.14 |
| C3 | 4.42 | 0.51 | 0.11 | 4.11 | 0.81 | 0.20 |
| D1 | 4.74 | 0.45 | 0.10 | 4.68 | 0.67 | 0.14 |
| D2 | 4.74 | 0.45 | 0.10 | 4.58 | 0.77 | 0.17 |
| D3 | 4.74 | 0.45 | 0.10 | 4.68 | 0.48 | 0.10 |
| D4 | 4.84 | 0.37 | 0.08 | 4.68 | 0.48 | 0.10 |
| D5 | 4.84 | 0.37 | 0.08 | 4.16 | 0.83 | 0.20 |
| D6 | 4.84 | 0.50 | 0.10 | 4.16 | 0.76 | 0.18 |
| D7 | 4.79 | 0.54 | 0.11 | 4.68 | 0.48 | 0.10 |
TABLE 5.
Care bundle review draft for preventing falls in hospitalized children
| Dimensions | Items |
|---|---|
|
A Human |
1. Children at high risk are identified (label on ID bands, hang sign and so on). a |
| |
| |
|
B Environment |
|
| |
| |
| |
| |
| |
| |
|
C Health |
|
| |
| |
|
D Care |
|
| |
| |
| |
| 5. The children at high risk are monitored every hour. a | |
| |
|
Specific preventive measures for children at high risk of falling.
4.3. Results of the trial test
In the trial test, the measures were non‐invasive and beneficial to the safety of the children during hospitalization, so no guardian of the children refused to participate. But four participants were excluded because of discharge or transfer within 24 hr of hospitalization. Finally, a total of 45 hospitalized children were enrolled as trial test subjects.
Of the 45 hospitalized children, 73.3% (n = 33) were male, 26.7% (n = 12) were female, 68.9% (n = 31) were at high fall risk, and 31.1% (n = 14) were at low fall risk. The average age was 3 years old. Admission diagnoses included respiratory diagnoses (77.8%), digestive diagnoses (4.5%), urinary diagnoses (2.2%), immunologic diagnoses (6.7%), neurologic diagnoses (4.4%), infectious diagnoses (2.2%) and other diagnoses (2.2%).
Nurses' overall compliance with the care bundle review draft in the trial test was 92.3%, 10 items were 100% implemented, 2 items with compliance less than 80% were specific preventive measures, 64.5% (item A1) and 54.8% (item D5), respectively (Table 6).
TABLE 6.
Nurses' compliance with the care bundle review draft in the trial test
| Items | Compliance (n/N) | Proportion (%) |
|---|---|---|
| A1 Labelled high‐risk children a | 20/31 | 64.5 |
| A3 Caregiver is at bedside | 45/45 | 100 |
| A4 Wear non‐slip footwear | 38/45 | 84.4 |
| B1 Keep the door open a | 25/31 | 80.6 |
| B2 Keep beds in the lowest position | 45/45 | 100 |
| B3 Place personal articles within reach | 43/45 | 95.6 |
| B4 Use protective devices appropriately | 45/45 | 100 |
| B5 No fluid on the floors and surfaces | 41/45 | 91.1 |
| B6 Keep environment free of obstacles | 45/45 | 100 |
| B7 Adequate lighting is provided | 45/45 | 100 |
| C1 Set up the fall prevention posters | 45/45 | 100 |
| C2 Provide fall prevention education | 41/45 | 91.1 |
| C3 Choose appropriate exercise methods | 39/45 | 86.7 |
| D1 Use validated risk assessment tools | 45/45 | 100 |
| D2 Reassessment of risk when status changes | 36/45 | 80.0 |
| D3 Have nursing protocols for preventing falls | 45/45 | 100 |
| D4 Evaluate medication administration times | 42/45 | 93.3 |
| D5 Hourly rounds a | 17/31 | 54.8 |
| D6 Offer assistance when needed | 45/45 | 100 |
| D7 Provide ambulation assistance | 45/45 | 100 |
| overall compliance | 792/858 | 92.3 |
Specific preventive measures for children at high risk of falling.
In the feedback collected from nurses, they reported that the assessment screened too many children at high risk of falls, making item D5 (i.e. hourly rounds) difficult to complete on time. In addition, the high‐risk labels hanging at the bedside were often missing because children removed or grabbed, so that the compliance of item A1 (i.e. labelled high‐risk children) was low.
4.4. Form the care bundle protocol
In response to the results of the trial test and the nurses' feedback, the research team conducted a literature review and held a research group meeting. After discussion, we decided to use the research results of Pauley (Pauley et al., 2014) for reference to increase the cut‐off score of HDFS to be greater than or equal to 15 as a high risk of falling, and 20 items for the care bundle protocol for preventing falls in hospitalized children were formed, including 17 general preventive measures and 3 specific preventive measures for children at high risk of falling (Figure 1, Table 7).
TABLE 7.
Care bundle protocol for preventing falls in hospitalized children
| Dimensions | Items |
|---|---|
|
A Human |
|
| |
| |
|
B Environment |
|
| |
| |
| |
| |
| |
| |
|
C Health |
|
| |
| |
|
D Care |
|
| |
| |
| |
| |
| |
|
Specific preventive measures for children at high risk of falling.
5. DISCUSSION
The care bundle protocol for preventing falls in hospitalized children has clinical significance. There is no nursing practice standard for preventing falls in hospitalized children in China. In September 2018, the CNQPA (2018) issued a care bundle to prevent falls in hospitalized patients. However, the care bundle is mainly for adults and is not applicable to hospitalized children. Guo et al. (2020) noted that it is necessary to explore the best strategies for fall prevention, so as to effectively ensure the safety of hospitalized children. Therefore, the care bundle protocol for preventing falls in hospitalized children developed in this study would provide a reference basis and standards for clinical nursing practice for preventing falls in hospitalized children.
The development process of the care bundle protocol for preventing falls in hospitalized children is scientific. A care bundle is a set of evidence‐based or self‐evident good practice‐based interventions for a defined patient population and care setting (Chen et al., 2020). Researchers also recommended developing an evidence‐based fall prevention programme (Guo et al., 2020; Kim, Kim, & Lim, 2021). In this study, first, through evidence retrieval, the latest evidence for preventing falls in hospitalized children was obtained. Second, based on the four basic concepts of nursing (Fawcett, 1984), four dimensions of the care bundle were formed. Combined with the care bundle for preventing falls in hospitalized patients (CNQPA, 2018), the first draft of the care bundle for preventing falls in hospitalized children was formed. The Delphi method was used to collect and revise the first draft strictly and repeatedly. Through the trial test, adjustments were made based on clinical practice, and finally, a care bundle protocol for preventing falls in hospitalized children with 4 dimensions and 20 items was formed, so that the care bundle protocol has a strong scientific design. The formation of the care bundle was evidence‐based, it not only combined the best available evidence but also attached the importance to the individual clinical experience.
The developmental process of the care bundle protocol for preventing falls in hospitalized children is reliable. The Delphi method in this study selected experts according to the expert selection criteria. The 19 experts selected came from seven provinces and cities in China, which had good universality. Among the experts, 42% had a graduate degree, and 74% had a senior professional title, which was quite representative. The expert response rate of the Delphi survey rounds was 100%, >70% (Hayes et al., 2015), and 16% of the experts who put forward constructive opinions had good expert enthusiasm. The expert authority coefficients of the Delphi survey rounds were 0.891 and 0.877, respectively, which showed good expert authority (Chen et al., 2020). All mean scores for importance and feasibility on items were all equal to or above 3.50, and the coefficients of variation were all equal to or below 0.25 in the second round; Kendall′s coefficients of concordance of the importance in Delphi survey rounds were 0.287 and 0.231, respectively, and Kendall′s coefficients of concordance of the feasibility were 0.269 and 0.281, respectively, and the differences were statistically significant (p < .01), indicating that the opinions of experts were relatively concentrated, the coordination was good, and the research results were reliable.
The care bundle protocol developed for preventing falls in hospitalized children is comprehensive and feasible to some extent. The occurrence of falls in hospitalized children is the result of the accumulation of many factors (AlSowailmi et al., 2018; Parker et al., 2020; Kim & Lee, 2021). When formulating fall prevention measures, appropriate evaluation, environmental safety and health education for children, their families and nursing staff should be fully considered (Guo et al., 2020; Kim, Kim, & Lim, 2021). To this end, the care bundle protocol includes 4 dimensions and 20 items in this study. It provides a comprehensive fall intervention for hospitalized children from the four aspects of children and their caregivers, environmental facilities, health education and nursing. The results showed that all mean scores for importance and feasibility on items were all equal to or above 3.50, and coefficients of variation were all equal to or below 0.25 in the second round, indicating that experts believed that the feasibility of the care bundle protocol for preventing falls in hospitalized children was high. Most of the included items of the care bundle for preventing falls in hospitalized children are widely used in clinical practice, which is of great significance to the general applicability of the care bundle protocol to prevent falls in hospitalized children, and it also conforms to the basic principles of the care bundle (Chen, 2016).
The results of the trial test showed that 2 items with compliance <80% were specific preventive measures. As to low compliance (64.5%) of item A1 (i.e. labelled high‐risk children), nurses reported that the high‐risk labels hanging at the bedside were often missing due to children′s removal or grabbing. In this regard, we believe that the compliance can be improved by changing the hanging position of labels or the way of marking in clinical practice. For the low compliance (54.8%) of item D5 (i.e. hourly rounds), nurses indicated that there were too many children at high risk of falls to complete hourly rounds on time. Based on the feedback of nurses on the trial test, we found through literature review that HDFS with the cut‐off score of 12 had high sensitivity but low specificity, so that an overestimate the number of the children were scored in the high risk of falls (Messmer et al., 2013; Pauley et al., 2014). Therefore, the number of children with a high risk of falling accounted for more than two‐thirds of subjects in our trial tests. Such overestimation of fall risk can lead to the waste of resources or the more serious problem of staff becoming desensitized, because of the impossibility of following up on the large number of children deemed to be at high risk (Messmer et al., 2013; Pauley et al., 2014; Webster et al., 2010). As a result, the item D5 had the lowest compliance at 54.8%. Pauley et al. (2014) stated 15 was the cut point of HDFS that reflected a balance between sensitivity and specificity.
Based on nurses' feedback and references, the research group immediately held a discussion meeting to determine the adjustment plan. Drawing on the research results of Pauley (Pauley et al., 2014), the cut‐off score of HDFS was raised to 15. After practical adjustments, the care bundle protocol for preventing hospitalized children from falling was successfully developed in this study and has certain feasibility.
6. LIMITATIONS
Due to the limitation of the time of the study, an evidence evaluation summary study was not carried out, and the evidence summary after quality evaluation was directly retrieved and used. The whole bundle is content‐rich; however, the quality of evidence included is not pretty high, there is a risk of bias to some extent. In addition, all the Delphi study members were in China, therefore the applicability of the bundle outside of China is unknown.
7. CONCLUSIONS
The care bundle protocol constructed based on four basic concepts of nursing and evidence for preventing falls in hospitalized children in this study was evaluated by the Delphi method and a trial test, which is scientific and reliable and has certain feasibility. It provides practical standards for nurses to implement nursing practices to prevent falls in hospitalized children and provides the basis for nursing managers to carry out nursing quality management to prevent falls in hospitalized children. In the future, pilot studies will be conducted to evaluate the feasibility and effectiveness of the clustered care programme for preventing falls in hospitalized children. Furthermore, the bundle has only been developed and trial tested in China, so its wider applicability needs further study.
FUNDING INFORMATION
The author(s) received no financial support for the research, authorship and/or publication of this article.
CONFLICT OF INTERESTS
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
ACKNOWLEDGEMENTS
We would like to acknowledge the experts who supported the study (especially in the Delphi study) and also to the clinical nurses and managers at the local hospitals who devoted their time to this project.
Chen, L. , Liu, W. , & Li, H. (2023). Development of an evidence‐based care bundle protocol for preventing falls in hospitalized children: Delphi study and trial test. Nursing Open, 10, 1715–1725. 10.1002/nop2.1427
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- Alemdaroglu, E. , Ozbudak, S. D. , Mandiroglu, S. , Bicer, S. A. , Ozgirgin, N. , & Ucan, H. (2017). Predictive factors for inpatient falls among children with cerebral palsy. Journal of Pediatric Nursing, 32, 25–31. 10.1016/j.pedn.2016.08.005 [DOI] [PubMed] [Google Scholar]
- Almis, H. , Bucak, I. H. , Konca, C. , & Turgut, M. (2017). Risk factors related to caregivers in hospitalized children′s falls. Journal of Pediatric Nursing, 32, 3–7. 10.1016/j.pedn.2016.10.006 [DOI] [PubMed] [Google Scholar]
- AlSowailmi, B. A. , AlAkeely, M. H. , AlJutaily, H. I. , Alhasoon, M. A. , Omair, A. , & AlKhalaf, H. A. (2018). Prevalence of fall injuries and risk factors for fall among hospitalized children in a specialized childrens hospital in Saudi Arabia. Annals of Saudi Medicine, 38(3), 225–229. 10.5144/0256-4947.2018.225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender, M. (2018). Re‐conceptualizing the nursing metaparadigm: Articulating the philosophical ontology of the nursing discipline that orients inquiry and practice. Nursing Inquiry, 25(3), e12243. 10.1111/nin.12243 [DOI] [PubMed] [Google Scholar]
- Benning, S. , & Webb, T. (2019). Taking the fall for kids: A journey to reducing pediatric falls. Journal of Pediatric Nursing, 46, 100–108. 10.1016/j.pedn.2019.03.008 [DOI] [PubMed] [Google Scholar]
- Chen, Y. (2016). Optimize and study of bundle for prevention of ventilator‐associated pneumonia in an intensive care unit (Graduate Thesis, Third Military Medical University). https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD201701&filename=1017035297.nh
- Chen, Y. , Li, Z. , Peng, J. , Shen, L. , & Shi, J. (2020). Development of a care bundle for stroke survivors with psychological symptoms: Evidence summary and delphi study. Evidence‐based Complementary and Alternative Medicine, 2020, 7836024. 10.1155/2020/7836024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- China Nursing Quality Promotion Alliance . (2018). Nursing quality process management toolkit. National Alliance for the Promotion of Nursing Quality Press. [Google Scholar]
- Ding, H.‐P. (2016). Application of cluster‐based nursing care in prevention of falling down and falling down from bed among inpatient children. Nursing of Integrated Tradition Chinese and Western Medicine, 2(7), 72–74. 10.11997/nitcwm.201607024 [DOI] [Google Scholar]
- Fawcett, J. (1984). The metaparadigm of nursing: present status and future refinements. Image—The Journal of Nursing Scholarship, 16(3), 84–89. 10.1111/j.1547-5069.1984.tb01393.x [DOI] [PubMed] [Google Scholar]
- Feuerlicht, D. , Agaliotis, M. , & Hinchcliff, R. (2020). Falling short: Examination of the validity of methods used to identify paediatric hospital falls in NSW, Australia. Public Health Research & Practice, 30(1), 29121907. 10.17061/phrp29121907 [DOI] [PubMed] [Google Scholar]
- Fujita, Y. , Fujita, M. , & Fujiwara, C. (2013). Pediatric falls: Effect of prevention measures and characteristics of pediatric wards. Japan Journal of Nursing Science, 10(2), 223–231. 10.1111/jjns.12004 [DOI] [PubMed] [Google Scholar]
- Guillaume, D. , Crawford, S. , & Quigley, P. (2016). Characteristics of the middle‐age adult inpatient fall. Applied Nursing Research, 31, 65–71. 10.1016/j.apnr.2016.01.003 [DOI] [PubMed] [Google Scholar]
- Guo, X.‐B. , Wang, Y. , Lu, Z.‐H. , Yang, X.‐K. , Wang, L. , & Tian, L. (2020). Research progress on the safety management strategy of fall prevention in hospitalized children. Journal of Nursing Administration, 20(10), 720–726. 10.3969/j.issn.1671-315x.2020.10.008 [DOI] [Google Scholar]
- Hayes, B. , Fitzgerald, D. , Doherty, S. , & Walsh, G. (2015). Quality care, public perception and quick‐fix service management: A Delphi study on stressors of hospital doctors in Ireland. BMJ Open, 5(12), e009564. 10.1136/bmjopen-2015-009564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He, J.‐F. , Tang, Y. , Zhang, C.‐Y. , Zhang, Z.‐G. , & Tian, J.‐H. (2016). Bibliometric analysis of literatures on hospitalized patients' falls in China from 2004 to 2015. Chinese Nursing Management, 16(10), 1393–1395. 10.3969/j.issn.1672-1756.2016.10.022 [DOI] [Google Scholar]
- Hill‐Rodriguez, D. , Messmer, P. R. , Williams, P. D. , Zeller, R. A. , Williams, A. R. , Wood, M. , & Henry, M. (2009). The Humpty Dumpty Falls Scale: A case–control study. Journal for Specialists in Pediatric Nursing, 14(1), 22–32. 10.1111/j.1744-6155.2008.00166.x [DOI] [PubMed] [Google Scholar]
- Humphrey‐Murto, S. , Varpio, L. , Gonsalves, C. , & Wood, T. J. (2017). Using consensus group methods such as Delphi and Nominal Group in medical education research. Medical Teacher, 39(1), 14–19. 10.1080/0142159X.2017.1245856 [DOI] [PubMed] [Google Scholar]
- International Council of Nurses . (2012). Closing the gap: From evidence to action . Retrieved from https://www.oegkv.at/fileadmin/user_upload/International/IND_Kit_2012_for_NNAs.pdf
- Kim, E. J. , Kim, G. M. , & Lim, J. Y. (2021). A systematic review and meta‐analysis of fall prevention programs for pediatric inpatients. International Journal of Environmental Research and Public Health, 18(11), 5853. 10.3390/ijerph18115853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, E. J. , & Lee, A. (2021). Analysis of fall incident rate among hospitalized Korean children using big data. Journal of Pediatric Nursing, 61, 136–139. 10.1016/j.pedn.2021.05.005 [DOI] [PubMed] [Google Scholar]
- Kim, E. J. , Lim, J. Y. , Kim, G. M. , & Min, J. (2021). An electronic medical record‐based fall risk assessment tool for pediatric inpatients in South Korea: Improved sensitivity and specificity. Child Health Nursing Research, 27(2), 137–145. 10.4094/chnr.2021.27.2.137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, Y. L. , Yip, W. K. , Goh, B. W. , Chiam, E. P. , & Ng, H. P. (2013). Fall prevention among children in the presence of caregivers in a paediatric ward: a best practice implementation. International Journal of Evidence‐Based Healthcare, 11(1), 33–38. 10.1111/1744-1609.12003 [DOI] [PubMed] [Google Scholar]
- Liu, Y.‐X. , & Shang, L.‐P. (2021). Research progress in the application of different management models in fall prevention of patients. Chinese Nursing Research, 35(6), 1016–1020. 10.12102/j.issn.1009-6493.2021.06.012 [DOI] [Google Scholar]
- Long, Y.‐A. (2018). Bibliometric analysis of clustered nursing research in China. Chinese Nursing Research, 32(18), 2955–2958. 10.12102/j.issn.1009-6493.2018.18.039 [DOI] [Google Scholar]
- McPherson, S. , Reese, C. , & Wendler, M. C. (2018). Methodology update: Delphi studies. Nursing Research, 67(5), 404–410. 10.1097/nnr.0000000000000297 [DOI] [PubMed] [Google Scholar]
- Messmer, P. R. , Williams, P. D. , & Williams, A. R. (2013). A case–control study of pediatric falls using electronic medical records. Rehabilitation Nursing, 38(2), 73–79. 10.1002/rnj.73 [DOI] [PubMed] [Google Scholar]
- Murray, E. , Vess, J. , & Edlund, B. J. (2016). Implementing a pediatric fall prevention policy and program. Pediatric Nursing, 42(5), 256–259. [PubMed] [Google Scholar]
- National Database of Nursing Quality Indicators (NDNQI) (2020). Guidelines for data collection and submission on patient falls‐Ambulatory indicator . Retrieved from https://members.nursingquality.org/NDNQIPortal/Documents/General/Guidelines%20‐%20PatientFalls.pdf?linkid=s0_f776_m73_m230_a0_m236_a0_m242_a0
- Obeid, S. (2017). Evidence Summary. Pediatric Patient Falls: Prevention . The Joanna Briggs Institute EBP Database. Retrieved from http://connect.jbiconnectplus.org/Search.aspx
- Parker, C. , Kellaway, J. , & Stockton, K. (2020). Analysis of falls within paediatric hospital and community healthcare settings. Journal of Pediatric Nursing, 50, 31–36. 10.1016/j.pedn.2019.09.026 [DOI] [PubMed] [Google Scholar]
- Pauley, B. J. , Houston, L. S. , Cheng, D. , & Johnston, D. M. (2014). Clinical relevance of the Humpty Dumpty Falls Scale in a pediatric specialty hospital. Pediatric Nursing, 40(3), 137–142. [PubMed] [Google Scholar]
- Sheppard‐Law, S. , Brogan, F. , Usherwood, F. , Hunstead, P. , & Shala, D. R. (2022). Predictors of parent′s knowledge of hospital‐based pediatric falls. Journal for Specialists in Pediatric Nursing, 27(2), e12368. 10.1111/jspn.12368 [DOI] [PubMed] [Google Scholar]
- The Joanna Briggs Institute . (2017). Recommended Practice. Pediatric Patient Falls: Prevention . The Joanna Briggs Institute EBP Database. Retrieved from http://connect.jbiconnectplus.org/ Search.aspx
- Webster, J. , Courtney, M. , Marsh, N. , Gale, C. , Abbott, B. , Mackenzie‐Ross, A. , & McRae, P. (2010). The STRATIFY tool and clinical judgment were poor predictors of falling in an acute hospital setting. Journal of Clinical Epidemiology, 63(1), 109–113. 10.1016/j.jclinepi.2009.02.003 [DOI] [PubMed] [Google Scholar]
- Wu, M.‐B. , & Hu, Y. (2013). Analysis of misunderstandings of care bundles and suggestion for clinical application. Journal of Nursing Science, 28(18), 84–86. [Google Scholar]
- Xiao, L. , Xie, L.‐L. , & Ling, S.‐Y. (2021). Clustered nursing bibliometrics based on Web of Science. Chinese Health Quality Management, 28(6), 70–74. 10.13912/j.cnki.chqm.2021.28.6.19 [DOI] [Google Scholar]
- Xu, G. X. (2016). Statistical forecasting and decision making (5th ed.). Shanghai University of Finance and Economics Press. [Google Scholar]
- Yi, J.‐L. , Chen, J.‐X. , Ye, T.‐H. , & Qin, X.‐L. (2018). Bundles of care for fall prevention in hospitalized children. Journal of Nursing Science, 33(3), 85–87. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


