Abstract
Introduction
Oncology care professionals are exposed to high levels of stress that can lead to burnout. The aim of this study was to investigate the prevalence of burnout among nurses, oncologists and radiographers working in oncology patient care during the COVID -19 pandemic.
Methods
Our electronic questionnaire was sent to e-mail contacts registered in the system of the Hungarian Society of Oncologists and to all oncology staff via an internal information system in each cancer center. Burnout was measured using the Maslach Burnout Inventory, which measures depersonalization (DP), emotional exhaustion (EE), and personal accomplishment (PA). Demographic and work-related characteristics were collected in our self-designed questionnaire. Descriptive statistics, chi-square tests, two-sample t-tests, analyzes of variance, Mann–Whitney and Kruskal–Wallis tests were performed.
Results
A total of 205 oncology care workers' responses were analyzed. Oncologists (n = 75) were found to be significantly more committed to DP and EE (p = 0.001; p = 0.001). Working more than 50 h per week and being on-call had a negative effect on the EE dimension (p = 0.001; p = 0.003). Coming up with the idea of working abroad had a negative effect on all three dimensions of burnout (p ≤ 0.05). Respondents who did not leave their job due to their current life situation had significantly higher DE, EE, and lower PA (p ≤ 0.05). Intention to leave current profession was specific in (n = 24/78; 30.8%) of nurses (p = 0.012).
Conclusion
Our results suggest that male gender, being an oncologist, working more than 50 h per week and taking on call duties have a negative impact on individual burnout. Future measures to prevent burnout should be integrated into the professionals' work environment, regardless of the impact of the current pandemic.
Implications for practice
Prevention and oncopsychological training should be developed gradually at the organisational or personal level to avoid early burnout of professionals.
Keywords: Oncology, Burnout, Oncologist, Nurse, Radiographer, Maslach burnout Inventory, COVID-19
Introduction
Given the endemic nature of the pandemic, increased attention needs to be paid to how best to support healthcare providers who are struggling with the stress of the pandemic at work and at home. Previous pandemics such as Severe Acute Respiratory Syndrome (SARS) and Influenza A virus subtype H1N1 (A/H1N1) have negatively impacted the mental health of healthcare providers.1 , 2
Hungary responded quickly to the threat of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and established the operational strain on 31st January 2020 with Government Decision 1012/2020 (1/31/2020).3 The first case was registered on 4th March 2020 and the first death was reported on 15th March 2020. Following the outbreak, a state of emergency was imposed on 11th March 2020. Along with the restrictions, health systems came under increasing pressure to cope with rising patient numbers.4 , 5
According to current literature, changes in mental health due to COVID -19 may vary by occupation and country.6, 7, 8 The basis for balanced human functioning is the harmonious unity of body and soul. The long-term psychological effects of increasing stress in health professionals are difficult to predict and need to be continuously monitored.7 , 8 In the context of oncology care, these risks and stressors for patients and providers are worsen. This means that the mental health of healthcare workers is of paramount importance and must be constantly monitored in an ever-changing environment.9, 10, 11
Burnout is a state of physical and mental exhaustion resulting from prolonged interpersonal and emotional stress, loss of caring and depletion of empathic capacity. Burnout develops over a long period of time. Individuals who perform their daily work in critical places and life situations (e.g. cancer care, emergency care, intensive care, etc.) are at increased risk.12 According to Maslach et al. to identify burnout, three factors need to be examined: emotional exhaustion, depersonalization, and a lower sense of personal accomplishment.13 The continuous maintenance of the relationship between medical staff and patients requires emotional labour, especially in oncological patient care. The multitude and variety of emotions and the mishandling of them are commonplace, overwhelming the person over time.6, 7, 8 , 12
Coping mechanisms are important in dealing with stress and its associated factors. Dysfunctional coping has been shown to be a significant predictor of burnout. The available literature shows that coping mechanisms and job satisfaction are related to the prevalence of burnout symptoms in the work environment. Often the tasks and responsibilities of health professionals are not aligned with the opportunities in the workplace and training for new tasks is often inadequate.14 , 15 It is therefore important to identify effective protective factors that can promote well-being and cushion the negative impact of emergency working conditions and demands. This process begins with recognising the impact of the pandemic on this particular group of professionals.
In Hungary, the somatic and psychological vulnerability of healthcare workers to workplace stress has been confirmed by numerous studies. These studies underline the high prevalence of physical and psychological symptoms due to chronic stress.16, 17, 18, 19
Study aim
As far as we know, no study has yet been conducted in Hungary that simultaneously analysed the prevalence of burnout among oncologists, nurses and radiation therapy radiographers working in oncology patient care. A further aim of the survey was to determine whether demographic and work-related factors have an influence on burnout in the above-mentioned professional group.
Methods
Study design, permission
A cross-sectional study was conducted and approved by the Medical Research Council (registration number: IV/617-3/2021/ECU). No questions were asked during data collection to identify the respondents, which contributed to the anonymity of the respondents. Informed consent was available to each respondent before completing the questionnaire. Completion of the questionnaire was completely voluntary and could be interrupted at any time.
Our questionnaire consisted of the Maslach Burnout Inventory-Human Services Survey (MBI-HSS) and our self-created questionnaire. The questionnaire was available between November 2020 and July 2021 and was supported by the Hungarian Society of Oncologists. Our e-questionnaire was sent in the form of a newsletter to the email contacts registered in the Society's system. The questionnaire was also distributed on the social media (Facebook) platforms of the relevant specialty groups. Our research group also contacted all oncology treatment centres in Hungary to inform the professionals about our research. The electronic questionnaire was also sent to all oncology staff via an internal information system in each centre. Monthly reminders were sent to the target group to complete the questionnaire.
The measurement of burnout
Burnout was measured with the MBI-Human Services Survey (MBI-HSS).10 To determine emotional exhaustion (EE), depersonalisation (DP) and personal accomplishment (PA), nine, five and eight questions were asked, respectively. The frequency of symptoms was calculated on a 7-point scale, with 0 representing “never” and 6 representing “every day”. Respondents with a score ≥27 in the dimension EE, ≥10 in the dimension DP or <33 in the dimension PA show a high level of burnout.10
The variables of the self-made questionnaire
We also collected demographic and work-related characteristics of oncology staff. Demographic characteristics included biological sex, age, marital status and number of children. Occupational characteristics included occupation, workplace, work experience, number of hours worked per week and presence of on-call duties during a month. In the literature, many publications mention the intention to leave the profession and the migration possibilities among oncology care professionals.20 Therefore, we were also interested in how respondents perceived working abroad and leaving the profession. We measured how much respondents valued their profession among health professionals, society and patients. Respondents could express their appreciation on a 10-point Likert scale, with a score of 1 representing the lowest appreciation and a score of 10 representing the highest appreciation.
Statistical analysis
Responses that were incomplete were excluded from our survey. After data cleaning, statistical analysis was conducted using Statistical Package for the Social Sciences (SPSS) version 23.0 software (IBM Inc, Armonk, NJ). Cronbach's alpha was measured to determine the internal consistency of a set of survey items from MBI-HSS. Descriptive statistics were used to determine the characteristics of the health workers in the sample and the levels of burnout. For normal distributions, a two-sample t-test and analysis of variance (ANOVA) were used to examine the relationship between nominal variables and scale scores. For non-parametric distributions, Mann–Whitney and Kruskal–Wallis tests were used. Chi-square tests were used to assess differences between nominal variables. The above statistical tests were performed with a confidence interval of 95% (p ≤ 0.05).
Results
A total of 205 respondents answered our questionnaire (mean age 46.6 years (SD = 12.6, range 22–83)). The majority of respondents were women (n = 158, 77.1%). In terms of profession, the proportion of radiographers (n = 52, 25.4%), nurses (n = 78, 38.0%) and oncologists (n = 75, 36.6%) was almost equal. The majority of respondents live with a spouse/partner and children (n = 148, 72.2%). Twenty-four percent of the sample had one child (n = 50) and another 45.3% had two or more children (n = 99). In terms of workplace, the majority of health workers worked in a county hospital (n = 91, 44.4%) with at least 20 years of work experience (n = 122, 59.5%). 59.0% (n = 121) of respondents work between 40 and 50 h per week, while another 58.0% (n = 119) do not perform on-call duties. 48.3% of the respondents (n = 99) are not interested in working abroad, but almost the same percentage (n = 84, 41.0%) would be interested in working abroad, but they stay in Hungary due to their current life situation. The vast majority of respondents (n = 134, 65.4%) would not like to change their profession (All results reported in Supplementary Table 1).
The Cronbach values were 0.729, 0.883, and 0.697 for the dimensions DE, EE, and PA, respectively, which can be considered an acceptable value.20
In terms of mean scores, DE was 6.42 (SD = 5.80), EE was 24.53 (SD = 12.26) and PA was 38.08 (SD = 5.95). 26.3% (n = 54) of the health workers were in the high category for DE and another 44.9% (n = 92) were in the high category for EE. PA was high for 46.3% (n = 95) of the respondents (Table 1 ).
Table 1.
The mean values and the severity of burnout for the dimensions of the MBI-HSS of the respondents.
| Maslach Burnout Inventory |
||
|---|---|---|
| Burnout dimension | Category | n (%) |
| Depersonalization | Low | 110 (53.7) |
| Moderate | 41 (20.0) | |
| High | 54 (26.3) | |
| OVERALL DEPERSONALIZATION MEAN | 6.42 (SD=5.80) | |
| Emotional Exhaustion | Low | 65 (31.7) |
| Moderate | 48 (23.4) | |
| High | 92 (44.9) | |
| OVERALL EMOTIONAL EXHAUSTION MEAN | 24.53 (SD=12.26) | |
| Personal Accomplishment | Low | 51 (24.9) |
| Moderate | 59 (28.8) | |
| High | 95 (46.3) | |
| OVERALL PERSONAL ACCOMPLISHMENT MEAN | 38.08 (SD=5.95) | |
When examining the relationship between burnout category severity and occupation, significantly more radiographers (57.7%, n = 30) and nurses (61.5%, n = 48) were classified in the low burnout group DE (χ2 = 11.657; p = 0.001). It should be noted that 41.3% (n = 31) of oncologists were classified in the high burnout group DE (χ2 = 21.271; p = 0.001) and another 60.0% (n = 45) were classified in the high burnout group EE (χ2 = 14.348; p = 0.006). When the PA dimension was examined, 57.7% of radiographers (n = 30), 46.2% of nurses (n = 36) and 38.7% of oncologists (n = 29) were in the high severity group (χ2 = 13.401; p = 0.009) (Table 2 ).
Table 2.
Severity of burnout of MBI-HSS dimensions regarding profession. (DE = depersonalization, EE = emotional exhaustion, PA = personal accomplishment).
| Low (n, %) | Moderate (n, %) | High (n, %) | ||
|---|---|---|---|---|
| DE | Radiographer | 30 (57.7) | 7 (13.5) | 15 (28.8) |
| Nurse | 48 (61.5) | 22 (28.2) | 8 (10.3) | |
| Oncologist | 32 (42.6) | 12 (16,1) | 31 (41.3) | |
| EE | Radiographer | 23 (44.3) | 10 (19.2) | 19 (36.5) |
| Nurse | 28 (35.9) | 22 (28.2) | 28 (35.9) | |
| Oncologist | 14 (18.7) | 16 (21.3) | 45 (60.0) | |
| PA | Radiographer | 17 (32.7) | 5 (9.6) | 30 (57.7) |
| Nurse | 16 (20.5) | 26 (33.3) | 36 (46.2) | |
| Oncologist | 18 (24.0) | 28 (37.3) | 29 (38.7) |
The dimension DE was significantly influenced by biological sex (t = 3.685; p = 0.001), profession (F = 5.996; p = 0.008), number of hours worked per week (F = 3.465; p = 0.033), being on call (t = 2.150; p = 0.033), the idea of working abroad (F = 11.577; p = 0.001) and the attitude of leaving the profession (F = 7.117; p = 0.001).
The dimension EE was significantly influenced by profession (F = 4.898; p = 0.008), number of hours worked per week (F = 8.200; p = 0.001), being on call (t = 2.971; p = 0.003), the idea of working abroad (F = 10.909; p = 0.001) and the attitude towards leaving the profession (F = 14.140; p = 0.001).
The dimension of PA was influenced only by the idea of working abroad (F = 5262; p = 0.006) and leaving the profession (F = 8915; p = 0.001) (Supplementary Table 1).
No significant relationship was found between profession and working abroad (χ2 = 9.149; p = 0.057). Intention to leave the profession was present in 30.8% of nurses (24/78), 15.3% of radiographers (8/52) and 13.3% (10/75) of oncologists. 76.9% of radiographers (40/52) and 72.0% of oncologists (54/75) did not consider leaving their profession (chi2 = 12.836; p = 0.012) (Table 3 ).
Table 3.
The attitude of working abroad and leaving the profession of the respondents.
| Are you interested in working abroad? | |||
|---|---|---|---|
| Profession (n) | Yes n (% | Yes, but due to my current life situation I'm staying n (% | No n (%) |
| Radiographer (52) | 2 (3.9%) | 21 (40.4%) | 29 (55.7%) |
| Nurse (78) | 6 (7.8%) | 36 (46.1%) | 36 (46.1%) |
| Oncologist (75) | 14 (18.7%) | 27 (36.0%) | 34 (45.3%) |
|
Are you interested or about to leave your profession? |
|||
| Yes n (% | Yes, but due to my current life situation I'm not starting a new one n (% | No n (% | |
| Radiographer (52) | 8 (15.3%) | 4 (7.8%) | 40 (76.9%) |
| Nurse (78) | 24 (30.8%) | 14 (17.9%) | 40 (51.3%) |
| Oncologist (75) | 10 (13.3%) | 11 (14.7%) | 54 (72.0%) |
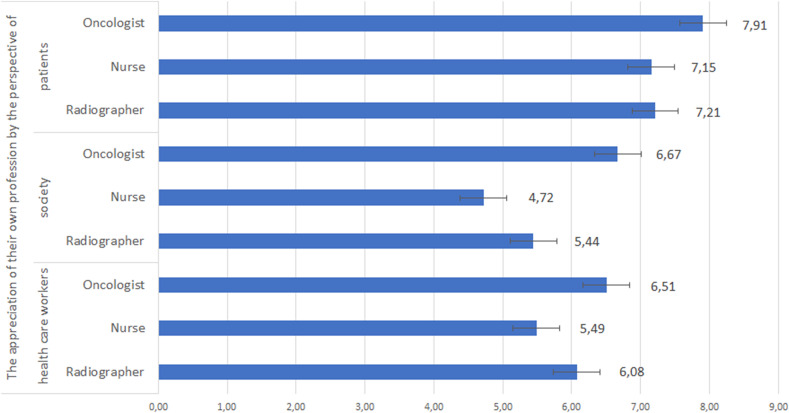
Oncologists rate the appreciation of their own profession significantly higher from the perspective of other healthcare workers (F = 4.546; p = 0.012), in society (F = 15.409; p = 0.001) and also from the perspective of patients (F = 3.166; p = 0.044) (Fig. 1 ).
Figure 1.
The appreciation of own profession by the perspective of healthcare workers, society and patients. A score of 1 represented the lowest appreciation and a score of 10 represented the highest appreciation. The error bars represent the standard error of the variable.
Discussion
Apart from the current pandemic, international literature reports increased emotional stress among professionals in oncology patient care, mainly due to patient suffering, death, on call duties, years spent in healthcare.9, 21, 22, 23 Chronic stress and inappropriate communication techniques can lead to burnout, which affects the quality of patient care, collegial relationships and the occurrence of medical errors as well.23 , 24 The presence of COVID-19 symptoms can further exacerbate psychological effects, including stress and burnout of the oncology patient care professionals.11 , 12 , 23 In our study, we investigated the prevalence of burnout and possible connecting work and demographic related influencing factors among radiographers, nurses and oncologists involved in oncology patient care during the pandemic COVID -19.
Regarding our study, 44.9% (92/205) of oncology care professionals were affected by high EE; 46.3% (95/205) by high PA and 26.3% (54/205) by high DE (Table 1). Also professionals who took on-call duties had higher DE and EE scores (Supplementary Table 1).
The phenomenon of burnout can be triggered by a variety of factors, which ultimately include career change intentions and professional migration.8 , 25, 26, 27 Arimon-Pagès et al.28 found compassionate fatigue, anxiety and a desire to leave the profession because of the ongoing demands of empathy in oncology nurses. This correlated with nurses' desire to change departments and leave their profession, and had a negative impact on staff satisfaction.
According to our own results, the nurses' self-assessment (from the perspective of society, patients and health professionals) was significantly lower than the scores of oncologists and radiographers' values. 30.7% of nurses are interested in changing profession, while a further 17.9% are not changing because of their current living situation. Overally, respondents who developed the idea of working abroad and also who are staying due to their current life situation had significantly higher scores on DE and EE. Respondents who are not interested starting a new profession due to their current life situation had significantly higher DE, EE and significantly lower PA. The intention of leaving profession affected significantly on DE and EE.
A meta-analysis by Yates et al.23 found that 32% of EE, 24% of DP and 37% of PA were among oncologists. In contrast, YG Lee et al.29 showed 74% high EE, 87% high DP and 65% low PA. In certain cases doctors experience burnout early in their careers.9 , 30 In contrast, Lazarescu et al.31 showed that older oncologists were more at risk regarding EE. According to the data of a Hungarian survey, 30% of them had already reached a significant level, and a quarter of them also suffered from psychosomatic (mental-physical) complaints.32
Regarding our research 41.3% (31/75) oncologists had high DE, 60.0% (45/75) high EE and 24.0% (18/75) high PA. There were no significant differences by work experience, but mean values on all three dimensions of burnout improved over time. It should be noted that oncologists rated their appreciation of their profession significantly higher (compared to radiographers and nurses in the survey) regarding patients, the society and other healthcare workers.
In a survey by Chen et al.,33 11.9% of nurses of oncology patients reported high levels of burnout EE, 18.7% DP and 36.1% PA. In a similar survey by Caliandro et al.,11 70% of the respondents were in the low EE group, surprisingly none of the respondents were affected by a high EE. As for DE, the majority of respondents (65.4%) were affected by a medium severity level. Male biological sex was found to be a predisposing factor for high PA. Książek et al.34 and Molavynejad et al.35 the intensity of burnout was significantly higher among nurses working in oncology patient care.
Among nurses only 10.3% (8/78) were affected by high DP, 35.9% (28/78) by high EE and 46.2% (36/78) by high PA. In terms of biological sex, men were significantly more affected by DP.
In a study by Singh et al.,36 high levels of EE, DE and PA were present in 93%, 87% and 61% of radiographers, respectively. Pereira et al.37 reported 43.5%, 45.5% and 59.8% from the same perspective. Radiographers cited high workload and labour shortages, as well as interpersonal conflicts, as the main causes of stress. Based on the findings of Zanardo et al.38 before and during the pandemic, radiographers showed high EE, DP and moderate PA. In a multivariate analysis, female biological sex and having children resulted in higher EE scores. With regard to our previous study, single radiographers who were on-call, worked more than 40 h per week and were involved in oncology patient care also showed high levels of EE. The presence of a child in the family had a positive effect on all dimensions of burnout.39 , 40
Based on our own results, radiographers were the least concerned about the dimensions of DE (57.7%; 30/52) and EE (44.3%; 23/52). PA was found to be high in 57.7% (30/52) of radiographers which is a result that is consistent with a relatively lower assessment of the appreciation of the profession. Overally, 40–50 h worked per week (excluding on-call) had a significant negative effect on the DP dimension. The EE dimension values increased significantly with increasing hours worked per week.
Study limitations
With regard to our results, we must emphasise that it is not possible to think of actual causal relationships due to the cross-sectional nature of our study. Our results do not apply to all Hungarian oncology care professionals, but are rather indicative. Further researches should focus on the long-term impact of the current pandemic on oncology professionals. Another limitation is the small number of respondents (22.3% in total), which could weaken the results of the group comparison in particular. The strengths of our study are that we investigated the level of burnout among oncologists, nurses and radiologists at the same time during the pandemic COVID -19 using a validated questionnaire, which is an internationally recognised measurement tool.
Conclusion
In summary, our study revealed the burnout levels of radiographers, nurses and oncologists working in oncology patient care. Our results suggest that male biological sex, being an oncologist, working more than 50 h per week and taking on call duties have a negative impact on individual burnout. The high emotional exhaustion of oncologists and the intention of almost one third of nurses to leave their profession give pause for thought. Radiographers were the least likely to consider working abroad or leaving their profession. Future measures to prevent burnout should be integrated into the professionals' work environment, regardless of the impact of the current pandemic.
Clinical implications
Burnout is the result of a process in which interruption is possible at any time. Prevention should be developed gradually and can be carried out at an organisational or personal level. It is important to emphasise the importance of burnout and oncopsychological training and its integration into the training curriculum, which is implemented in several centres in Hungary and all over the world as well. The training can be completed at practise sites. Learning and developing dialogue and building a relationship with the patient starts at this point in the practise. Besides being used in training, art therapies and exercises are known to be effective in preventing burnout. Therefore, it is recommended to have regular exercise programmes even during hard clinical work.41, 42, 43
Author contributions
David Sipos: Conceptualization, Methodology, Formal analysis, Investigation, Writing – Original Draft.
Olivér Kunstár: Formal analysis, Writing.
Árpád Kovács: Writing - Review and Editing.
Melinda Petőné Csima: Supervision, Methodology, Writing – Review and Editing.
Conflict of interest
None.
Footnotes
Permanent address: Department of Medical Imaging, Faculty of Health Sciences, University of Pécs, Szent Imre street 14/B, 7400 Kaposvár, Hungary.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.radi.2023.02.009.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Blake H, Bermingham F., Johnson G., Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. Int J Environ Res Publ Health. 2020;17(9) doi: 10.3390/ijerph17092997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maben Jill, Bridges Jackie. Covid-19: supporting nurses' psychological and mental health. J Clin Nurs 29(15-16):2742-2750. 10.1111/jocn.15307. [DOI] [PMC free article] [PubMed]
- 3.Governmental decree 1012/2020. (I. 31.) on establishing executive board on defense against COVID–19. A kormány 1012/2020. (1. 31.) korm. Határozata a koronavírus-járvány elleni védekezésért felelős operatív törzs felállításáról. Hatályos: 2020.01.31.–2020.06.17. Magyar Közlöny 2020. január 31. Hungarian.
- 4.The first COVID–19 patient is dead. [Meghalt az első koronavírusos beteg.] Available from: https://web.archive.org/web/20200317064138/https://koronavirus.gov.hu/cikkek/meghalt-az-elso-magyar-beteg [accessed: November 24, 2022]. [Hungarian].
- 5.Strengthening the health system response to COVID-19 – Re- commendations for the WHO European Region: policy brief, 1 April 2020 produced by the WHO European Region).
- 6.Liu C., Zhao Y., Okwan-Duodu D., Basho R., Cui X. COVID-19 in cancer patients: risk, clinical features, and management. Cancer Biol Med. 2020;17(3):519–527. doi: 10.20892/j.issn.2095-3941.2020.0289. [online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teo I., Chay J., Cheung Y.B., Sung S.C., Tewani K.G., Yeo L.F., et al. Healthcare worker stress, anxiety and burnout during the COVID-19 pandemic in Singapore: a 6-month multi-centre prospective study. PLoS One. 2021 doi: 10.1371/journal.pone.0258866. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1480457 [online] pp.e0258866–e0258866. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duarte I., Teixeira A., Castro L., Marina S., Ribeiro C., Jácome C., et al. Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Publ Health. 2020;20(1) doi: 10.1186/s12889-020-09980-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alacacioglu A., Yavuzsen T., Dirioz M., Oztop I., Yilmaz U. Burnout in nurses and physicians working at an oncology department. Psycho Oncol. 2009;18(5):543–548. doi: 10.1002/pon.1432. [DOI] [PubMed] [Google Scholar]
- 10.Ádám S.Z., Mészáros V. Psychometric properties and health correlates of the Hungarian Version of the Maslach Burnout Inventory — human Services Survey (MBI-HSS) among physicians; (A humán szolgáltató szektorban dolgozók kiégésének mérésére szolgáló Maslach Kiégés Leltár magyar változatának pszichometriai jellemzői és egészségügyi korrelátumai orvosok körében) Mentálhigiéné es Pszichoszomatika. 2012;13:127–143. doi: 10.1556/mental.13.2012.2.2. [DOI] [Google Scholar]
- 11.Caliandro M., Fabiana G., Surgo A., Carbonara R., Ciliberti M.P., Bonaparte I., et al. Impact on mental health of the COVID-19 pandemic in a radiation oncology department. La Radiologia Medica. 2022;127(2):220–224. doi: 10.1007/s11547-021-01440-x. [online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cañadas-De la Fuente G.A., Gómez-Urquiza J.L., Ortega-Campos E.M., Cañadas G.R., Albendín-García L., De la Fuente-Solana E.I. Prevalence of burnout syndrome in oncology nursing: a meta-analytic study. Psycho Oncol. 2018;27(5):1426–1433. doi: 10.1002/pon.4632. [online] [DOI] [PubMed] [Google Scholar]
- 13.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 14.Maresca G., Corallo F., Catanese G., Formica C., Lo Buono V. Coping strategies of healthcare professionals with burnout syndrome: a systematic review. Medicina (Kaunas, Lithuania) 2022;58(2):327. doi: 10.3390/medicina58020327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Montero-Marin J., Prado-Abril J., Piva Demarzo M.M., Gascon S., García-Campayo J. Coping with stress and types of burnout: explanatory power of different coping strategies. PLoS One. 2014;9(2) doi: 10.1371/journal.pone.0089090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Czeglédi E., Tandari-Kovács M. Characteristics and prevention of burnout syndrome among nurses. Orv Hetil. 2019;160(1):12–19. doi: 10.1556/650.2019.30856. [online] [DOI] [PubMed] [Google Scholar]
- 17.Győrffy Z., Girasek E. Burnout among Hungarian physicians. Who are the most jeopardized? Orv Hetil. 2015;156(14):564–570. doi: 10.1556/oh.2015.30121. [DOI] [PubMed] [Google Scholar]
- 18.Mészáros V., Cserháti Z., Oláh A., Perczel Forintos D., Ádám S. Coping with work-related stress in health care professionals – strategies for prevention of burnout and depression. Orv Hetil. 2013;154(12):449–454. doi: 10.1556/oh.2013.29572. [DOI] [PubMed] [Google Scholar]
- 19.Kovács M., Kovács E., Hegedűs K. Is emotional dissonance more prevalent in oncology care? Emotion work, burnout and coping. Psycho Oncol. 2009;19(8):855–862. doi: 10.1002/pon.1631. [DOI] [PubMed] [Google Scholar]
- 20.Tavakol M., Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shanafelt T.D., Raymond M., Kosty M., Satele D., Horn L., Pippen J., et al. Satisfaction with work-life balance and the career and retirement plans of US oncologists. J Clin Oncol Off J Amer Soc Clin Oncol. 2014;32(11):1127–1135. doi: 10.1200/JCO.2013.53.4560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duarte, J. and Pinto-Gouveia, J. (2016). Effectiveness of a mindfulness-based intervention on oncology nurses' burnout and compassion fatigue symptoms: a non-randomized study. Int J Nurs Stud, 64, pp.98–107. doi:10.1016/j.ijnurstu.2016.10.002. [DOI] [PubMed]
- 23.Yates M., Samuel V. Burnout in oncologists and associated factors: a systematic literature review and meta-analysis. Eur J Cancer Care. 2019;28(3) doi: 10.1111/ecc.13094. [DOI] [PubMed] [Google Scholar]
- 24.Shanafelt T.D., Balch C.M., Bechamps G., Russell T., Dyrbye L., Satele D., et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000. doi: 10.1097/sla.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 25.Shah M., Roggenkamp M, Ferrer L., Burger V., Brassil K.J. Mental health and COVID-19: the psychological implications of a pandemic for nurses. Clin J Oncol Nurs. 2021;25(1):69–75. doi: 10.1188/21.CJON.69-75. [DOI] [PubMed] [Google Scholar]
- 26.Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Globalization Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Desideri I., Francolini G., Ciccone L.P., Stocchi G., Salvestrini V., Aquilano M., et al. Impact of COVID-19 on patient–doctor interaction in a complex radiation therapy facility. Support Care Cancer. 2021;29(6):2931–2937. doi: 10.1007/s00520-020-05793-3. [online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arimon-Pagès E., Torres-Puig-Gros J., Fernández-Ortega P., Canela-Soler J. Emotional impact and compassion fatigue in oncology nurses: results of a multicentre study. Eur J Oncol Nurs. 2019;43 doi: 10.1016/j.ejon.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 29.Lee Y.-G., Maeng C.H., Kim D.Y., Kim B.-S. Perspectives on professional burnout and occupational stress among medical oncologists: a cross-sectional survey by Korean society for medical oncology (ksmo) Cancer Research and Treatment. 2020 doi: 10.4143/crt.2020.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ogundipe O.A., Olagunju A.T., Lasebikan V.O., Coker A.O. Burnout among doctors in residency training in a tertiary hospital. Asian J Psychiatry. 2014;10:27–32. doi: 10.1016/j.ajp.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 31.Lazarescu I., Dubray B., Joulakian M.B., Blanchard P., Chauvet B., Mahé M.-A., et al. Prevalence of burnout, depression and job satisfaction among French senior and resident radiation oncologists. Cancer Radiother. 2018;22(8):784–789. doi: 10.1016/j.canrad.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 32.Szidónia P., Ferenc T. A pályakezdő orvosok jövőképe és egészségi állapota. Lege Artis Med. 2010;20(06-07):423–429. https://elitmed.hu/kiadvanyaink/lege-artis-medicinae/a-palyakezdo-orvosok-jovokepe-es-egeszsegi-allapota [online] Available at. (Accessed 16 June 2022) [Google Scholar]
- 33.Chen Z., Leng J., Pang Y., He Y., Heng F., Tang L. Demographic, occupational, and societal features associated with burnout among medical oncology staff members: cross-sectional results of a Cancer Center in Beijing, China. Psycho-Oncol. 2019;28(12):2365–2373. doi: 10.1002/pon.5230. [online] [DOI] [PubMed] [Google Scholar]
- 34.Książek I., Stefaniak T.J., Stadnyk M., Książek J. Burnout syndrome in surgical oncology and general surgery nurses: a cross-sectional study. Eur J Oncol Nurs. 2011;15(4):347–350. doi: 10.1016/j.ejon.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 35.Molavynejad S., Babazadeh M., Bereihi F., Cheraghian B. Relationship between personality traits and burnout in oncology nurses. J Fam Med Prim Care. 2019;8(9):2898. doi: 10.4103/jfmpc.jfmpc_423_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh N., Wright C., Knight K., Baird M., Akroyd D., Adams R.D., et al. Occupational burnout among radiation therapists in Australia: findings from a mixed methods study. Radiography. 2017;23(3):216–221. doi: 10.1016/j.radi.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 37.Pereira J.M., Cristiana S., Davide F., Ana S. Burnout among Portuguese radiographers during the COVID-19 pandemic. Radiography. 2021 doi: 10.1016/j.radi.2021.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zanardo M., Cornacchione P., Marconi E., Dinapoli L., Fellin F., Gerasia R., et al. Occupational burnout among radiation therapy technologists in Italy before and during COVID-19 pandemic. J Med Imag Radiat Sci. 2022;53(1):58–64. doi: 10.1016/j.jmir.2021.12.004. [online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sipos D., Vandulek C., Pandur A.A., Kovács P., Cseh S., Kedves A., et al. The effect of family and workplace characteristics on the burnout level of radiographers working in oncology patient care. Med Imag Radiotherapy J. 2020;37(2):5–12. doi: 10.47724/MIRTJ.2020.i02.a001. [online] [DOI] [Google Scholar]
- 40.Sipos D., Varga V., Pandur A.A., Kedves A., Petőné Csima M., Cseh S., et al. Burnout level among radiology department workers in Hungary. Orvosi Hetilap. 2019;160(27):1070–1077. doi: 10.1556/650.2019.31442. [online] [DOI] [PubMed] [Google Scholar]
- 41.Maresca G., Corallo F., Catanese G., Formica C., Lo Buono V. Coping strategies of healthcare professionals with burnout syndrome: a systematic review. Medicina (Kaunas, Lithuania) 2022;58(2327) doi: 10.3390/medicina58020327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bretland R.J., Thorsteinsson E.B. Reducing workplace burnout: the relative benefits of cardiovascular and resistance exercise. PeerJ. 2015;3:e891. doi: 10.7717/peerj.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guveli H., Anuk D., Oflaz S., Guveli M.E., Yildirim N.K., Ozkan M., et al. Oncology staff: burnout, job satisfaction and coping with stress. Psycho Oncol. 2015;24(8):926–931. doi: 10.1002/pon.3743. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.