Abstract
Background
With widespread use of the internet and mobile devices, many people have gained improved access to health-related information online for health promotion and disease management. As the health information acquired online can affect health-related behaviors, health care providers need to take into account how each individual’s online health literacy (eHealth literacy) can affect health-related behaviors.
Objective
To determine whether an individual’s level of eHealth literacy affects actual health-related behaviors, the correlation between eHealth literacy and health-related behaviors was identified in an integrated manner through a systematic literature review and meta-analysis.
Methods
The MEDLINE, Embase, Cochrane, KoreaMed, and Research Information Sharing Service databases were systematically searched for studies published up to March 19, 2021, which suggested the relationship between eHealth literacy and health-related behaviors. Studies were eligible if they were conducted with the general population, presented eHealth literacy according to validated tools, used no specific control condition, and measured health-related behaviors as the outcomes. A meta-analysis was performed on the studies that could be quantitatively synthesized using a random effect model. A pooled correlation coefficient was generated by integrating the correlation coefficients, and the risk of bias was assessed using the modified Newcastle-Ottawa Scale.
Results
Among 1922 eHealth literacy–related papers, 29 studies suggesting an association between eHealth literacy and health-related behaviors were included. All retrieved studies were cross-sectional studies, and most of them used the eHealth Literacy Scale (eHEALS) as a measurement tool for eHealth literacy. Of the 29 studies, 22 presented positive associations between eHealth literacy and health-related behaviors. The meta-analysis was performed on 14 studies that presented the correlation coefficient for the relationship between eHealth literacy and health-related behaviors. When the meta-analysis was conducted by age, morbidity status, and type of health-related behavior, the pooled correlation coefficients were 0.37 (95% CI 0.29-0.44) for older adults (aged ≥65 years), 0.28 (95% CI 0.17-0.39) for individuals with diseases, and 0.36 (95% CI 0.27-0.41) for health-promoting behavior. The overall estimate of the correlation between eHealth literacy and health-related behaviors was 0.31 (95% CI 0.25-0.34), which indicated a moderate correlation between eHealth literacy and health-related behaviors.
Conclusions
Our results of a positive correlation between eHealth literacy and health-related behaviors indicate that eHealth literacy can be a mediator in the process by which health-related information leads to changes in health-related behaviors. Larger-scale studies with stronger validity are needed to evaluate the detailed relationship between the proficiency level of eHealth literacy and health-related behaviors for health promotion in the future.
Keywords: eHealth literacy, digital health literacy, online health information, health-related behaviors, health-promoting behavior, meta-analysis
Introduction
Background
The development of digital media and communication technology has increased access to information, and a growing proportion of health-related information is being gained through the internet. A survey conducted in the United States reported that 59% of survey participants had experience in retrieving health information online and 35% had experience in self-diagnosing their health status using online health information [1]. The internet offers the advantage of quick and easy access to a vast amount of up-to-date information and allows communication with health care experts using diverse media platforms such as social networking websites, messengers, and video streaming services [2]. The internet’s capacity goes beyond the realm of merely acquiring health-related information, as bidirectional or multidirectional information sharing is also possible [3].
Furthermore, owing to the widespread penetration of the internet and mobile devices, numerous health care professionals increasingly use web-based or online materials to provide information to patients [4]. Previous studies have demonstrated that digital information can be implemented and used positively for public health projects, such as smoking cessation, weight control, and alcohol addiction management [5-7]. Although access to a wide range of information has improved with the internet, information on the internet comes from a variety of providers and sources that are difficult to control, which can lead to problems with quality and the risk of circulating biased content according to the interests and purposes involved [8].
Therefore, moving forward from the concept of traditional health literacy, the ability to seek, find, understand, and appraise health information from an electronic source has emerged as eHealth literacy [9,10]. Health literacy, a concept preceding eHealth literacy, is shown to be closely associated with health-related factors, such as health behavior, disease management, and quality of life, in various studies [11-13]. Likewise, numerous studies on eHealth literacy, including the development of measurement tools, measurement of individuals’ eHealth literacy, and identification of factors contributing to eHealth literacy, have been steadily conducted [14-17]. However, not much is known about the association between eHealth literacy and health-related behaviors, especially whether eHealth literacy can influence changes in the actual behavior. We raised the question of whether eHealth literacy might be the key mediator from obtaining online health information to changing actual health-related behaviors. Since extensive health information is available online and the acquisition of the information could influence individuals’ health-related behaviors, such as disease management, medication adherence, and seeking health care services [18], a comprehensive review of the influence of eHealth literacy on actual health-related behaviors affected by online health-related information is needed.
Objectives
Therefore, we performed a systematic review and meta-analysis to describe the effect of eHealth literacy on the types of health-related behaviors and to present the pooled quantitative relationship between them.
Methods
Definitions of eHealth Literacy and Health-Related Behaviors
The theoretical definition of eHealth literacy refers to the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem [10]. In our study, eHealth literacy was operationally defined as the total eHealth literacy score measured with a validated measurement tool, such as the eHealth Literacy Scale (eHEALS) developed by Norman and Skinner [19].
Health-related behaviors were defined as “behavioral patterns, actions, and habits that relate to health maintenance, to health restoration, and to health improvement” and included the use of health care services, such as vaccinations and health checkups, compliance with medical therapy, such as treatment diet or medication, and self-directed health behaviors related to diet, exercise, smoking, drinking, etc [20]. In this study, health-related behaviors were operationally defined and subsequently analyzed in the following 3 categories: health-promoting behavior, health-supporting behavior, and disease management behavior (Table 1). Health-promoting behavior consisted of the following 6 dimensions: nutrition, physical activity, health responsibility, stress management, interpersonal relations, and self-realization. It was measured with tools such as Health-Promoting Lifestyle Profile (HPLP) II [21]. Health-supporting behavior was defined as a health-related behavior that was only a part of the dimension of health-promoting behavior or was not included in health-promoting behavior. It was measured by the absence or presence of each experience, or the total score obtained using measurement tools of health behaviors such as Healthy Lifestyle and Personal Control Questionnaire [22]. Lastly, disease management behavior included any activity performed to manage a specific disease and was quantified by measurement tools according to disease-specific behavioral characteristics such as the Self-Care of Heart Failure Index [23].
Table 1.
Operational classification and definitions of health-related behaviors.
| Health-related behavior | Operational definition |
| Health-promoting behavior | A holistic behavioral pattern that includes health responsibility, nutrition, physical activity, stress management, interpersonal relations, and self-realization [24] |
| Health-supporting behavior | Lifestyle habits and disease prevention behaviors for maintaining health [25], which are only a part of the dimension of health-promoting behavior or are not included in health-promoting behavior |
| Disease management behavior | All activities performed to manage a specific disease |
Literature Search
We performed this systematic review and meta-analysis in accordance with the PICO-SD (Population, Intervention, Comparator, Outcome, Study Design) framework and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Multimedia Appendix 1) [26]. We searched MEDLINE, Embase, Cochrane Central Register of Controlled Trials, KoreaMed, and Research Information Sharing Service to collect research papers published until March 19, 2021. The search keywords combined synonyms of eHealth with synonyms of literacy for a more comprehensive search. Additional manual searches to find relevant studies were also performed by reviewing the bibliographies from the retrieved papers. The detailed search strategy is presented in Multimedia Appendix 2.
Eligible Criteria and Study Selection
For the systematic review, searched studies were selected according to the following inclusion criteria:
Population: Study participants were from the general population and were not health care professionals or students majoring in health care. Participants were not excluded based on their age, race, or morbidity status.
Intervention: Studies that reported levels of eHealth literacy measured by validated quantification tools, such as the eHEALS, were included.
Comparator: There was no specific comparator.
Outcomes: The outcomes of the included studies had to suggest objectively measured health-related behaviors. The behaviors could be evaluated individually or could be integrated.
Study design: Studies were selected regardless of their study design, except for qualitative studies.
Studies were excluded if they were (1) not measuring eHealth literacy or not using validated eHealth literacy measurement tools; (2) qualitative studies or not original research papers; (3) not written in either English or Korean; or (4) not available in full text.
The literature search and selection process was performed independently by 2 reviewers (KK and SS). Any discordance among the reviewers during the process of literature selection was resolved through mutual agreement or by involving a third researcher (SK) in a discussion. If two or more studies were performed on the same set of participants, the studies were considered duplicates, and only 1 comprehensive study was selected for further analysis.
Data Extraction and Risk of Bias Assessment
The following data were extracted from the selected literature using a standardized form by 2 reviewers (KK and SS): the characteristics of the studies (first author, publication year, country or location, study design, participants, and sample size); types of eHealth literacy scales; mean eHealth literacy score; types of health-related behaviors whose correlations with eHealth literacy were verified; methods of measuring health-related behaviors; statistical analysis methods; types of outcome indicators; and values of outcome indicators. Any inconsistency or ambiguity was resolved by discussion with other reviewers (SK and EL).
The risk of bias in the selected studies was assessed using the modified Newcastle-Ottawa Scale (NOS). While the NOS was developed for assessing the risk of bias in nonrandomized observational studies [27], our study used the modified NOS [28] that was developed for cross-sectional studies. The NOS uses a star system to assess the risk of bias in studies, whereby a lower score (ie, number of stars) is associated with a higher risk of bias: high risk, 0-3 stars; unclear risk, 4-6 stars; and low risk, 7-9 stars. Studies evaluated to have a high risk of bias were excluded from the meta-analysis.
Qualitative and Quantitative Synthesis of the Results
For a qualitative analysis of the results, study country, study population, eHealth literacy measurement tools, types of health-related behaviors and measurement tools, and the relationship between eHealth literacy and health-related behaviors were presented descriptively. The characteristics of the study population were described by age and morbidity status. The specific contents of health-related behaviors were summarized, and they were also classified into the following 3 categories: health-promoting behavior, health-supporting behavior, and disease management behavior. The relationship between eHealth literacy and health-related behaviors was evaluated by whether the effect of eHealth literacy was positive or negative.
For evaluating the association between eHealth literacy and health-related behaviors by a quantitative method, the pooled correlation coefficient was estimated by Fisher z-transformation and construction of the inverse transformation [29]. We used the correlation coefficients of individual studies and treated each result as a separate study when multiple subgroup results were reported in 1 study. The pooled correlation coefficient presented with a 95% CI was tested by performing hypothesis testing to determine whether the correlation was statistically significant. Interpretation of the pooled correlation coefficient was conducted according to Cohen criteria [30]. Cochran Q-statistics and I2-statistics were used to assess the heterogeneity within the studies included in the meta-analysis, and we applied either the fixed-effects model or random-effects model, depending on the significance of heterogeneity (P<.10 and I2≥50%) [29]. To test the validity of the study results, publication bias was evaluated using a funnel plot and Egger regression, and in case of suspected publication bias, the severity of bias was tested using the trim-and-fill method to estimate the degree to which the publication bias would affect the validity of the study results.
The total effect size (ie, pooled correlation coefficient) was derived from each group of studies divided by the participants’ mean age, morbidity status, and types of health-related behaviors, and from all studies that could be quantitatively synthesized. Through this, we tried to evaluate changes in the effect size according to detailed characteristics. All statistical analyses were performed using Comprehensive Meta-analysis, version 2 software (Biostat).
Results
Study Selection
Of 1922 identified nonduplicate studies, 1481 studies were excluded after a review of the studies’ titles and abstracts. The remaining 441 studies were assessed for eligibility through full-text review. Finally, 29 studies, which presented the association between eHealth literacy and health-related behaviors, were selected for qualitative analysis. Out of these, only 14 studies that were quantitatively synthesizable for analysis were included in the meta-analysis. The detailed study selection process with the reasons for exclusion during screening steps is shown in Figure 1.
Figure 1.
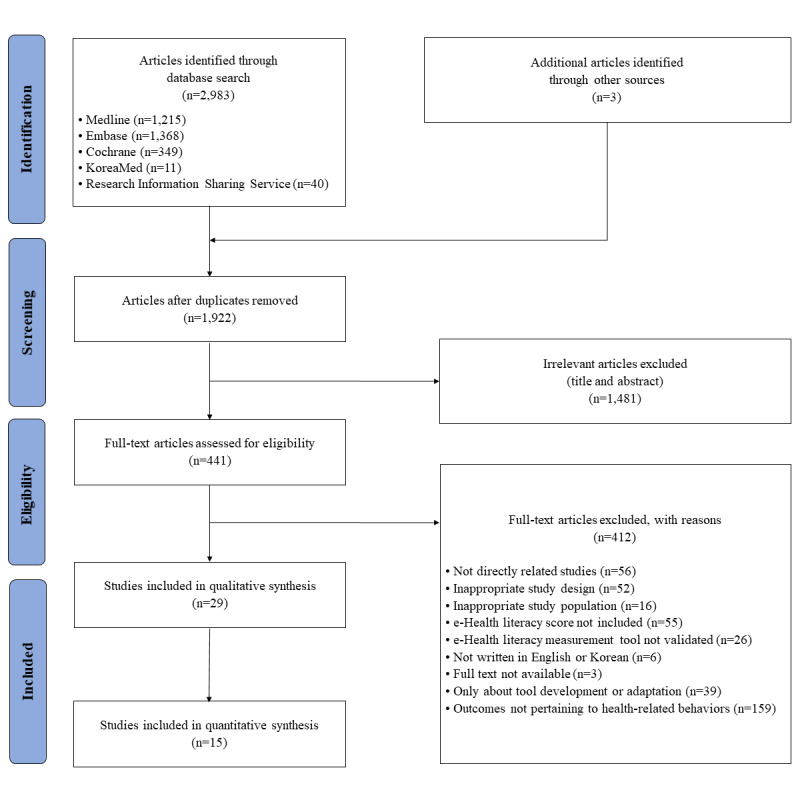
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of the study selection process.
Characteristics of the Included Studies
The overall characteristics of the included studies are summarized in Table 2 [31-59]. Among the 29 studies, most were published in South Korea (n=9), followed by Taiwan (n=5), the United States (n=4), China (n=3), Japan (n=3), Turkey (n=2), Germany/Austria (n=1), Iran (n=1), and Pakistan (n=1), showing that most of the studies were conducted in Asia. All retrieved studies were cross-sectional studies using questionnaires. The age groups of the study participants varied, and there were teenagers [31,32], college students [33-40], and older adults [41-46]. While most studies were conducted on the general population regardless of disease status, 6 studies [41,47-51] were conducted on patients with specific diseases, including heart failure, hypertension, diabetes, cancer, and HIV infection.
Table 2.
Characteristics of the included studies.
| Author (year) | Country | Population (sample n) | eHLa measurement tool | Health-related behaviors measurement tool | Types of health-related behaviors | Risk of bias |
| An et al (2021) [52] | United States | Adults aged over 18 years (n=1074) | Coronavirus-related eHEALSb | 7 self-reported items | Infection prevention behaviors | 6 |
| Blackstock et al (2016) [47] | United States | HIV-infected adult women (n=63) | eHEALS | HIV Risk-Taking Behaviour Scale and Addiction Severity Index | High-risk sexual and drug use behaviors | 6 |
| Britt et al (2017) [34] | United States | College students (n=420) | eHEALS | Questions for the 8 health areas identified from the American College Health Association | Diet, exercise, sleep, harmful substances, vaccination, safe sex practices, social relationship, and overall health | 3 |
| Cho and Ha (2019) [48] | Korea | Adult outpatients with hypertension (n=156) | Korean version of eHEALS | Self-care behaviors measurement tool | Diet, weight control, stress management, alcohol and tobacco use, physical activity, and medication | 7 |
| Choi (2020) [42] | Korea | Older adults aged over 65 years (n=198) | Korean version of eHEALS | Adapted HPLPc Ⅱ | Health responsibility, physical activity, nutrition, spiritual development, interpersonal support, and stress management | 6 |
| Chuang et al (2019) [49] | Taiwan | Adults with heart failure (n=141) | Chinese version of eHEALS | 22-item instrument Self-Care of Heart Failure Index version 6.2 | Self-care maintenance, management, and confidence in heart failure | 6 |
| Cui et al (2021) [43] | China | Older adults aged over 60 years (n=1201) | Chinese version of eHEALS | HPLP | Self-actualization, health responsibility, exercise, nutrition, interpersonal support, and stress management | 8 |
| Guo et al (2021) [50] | Taiwan | Diabetes mellitus outpatients aged 20 to 65 years (n=249) | eHEALS | 36-item Diabetes Self-care Behavior questionnaire | Self-care activities related to diabetes mellitus | 4 |
| Gürkan and Ayar (2020) [31] | Turkey | High school students (n=219) | Turkish version of eHEALS | Adolescent Health Promotion Scale | Diet, life appreciation, social support, exercise, stress management, and health responsibility | 6 |
| Hsu et al (2014) [33] | Taiwan | College students (n=525) | eHLSd | Self-developed 12-item Health Behavior Scale | Diet, exercise, and sleep behaviors | 8 |
| Hwang and Kang (2019) [35] | Korea | College students (n=242) | eHL scale composed of functional, communicative, and critical eHL | Adapted HPLP Ⅱ | Health responsibility, physical activity, nutrition, spiritual development, interpersonal support, and stress management | 8 |
| Kim and Kim (2020) [51] | Korea | Cancer patients aged 19 to 64 years (n=76) | Adapted eHEALS | Adapted HPLP Ⅱ | Health responsibility, physical activity, nutrition, spiritual development, interpersonal support, and stress management | 6 |
| Kim and Son (2017) [53] | Korea | Young adults aged 18 to 39 years (n=230) | Korean version of eHEALS | 5-item validated Health-Related Behaviors Scale | Behaviors to prevent disease and promote health | 9 |
| Korkmaz Aslan et al (2021) [32] | Turkey | Students aged 14 to 19 years (n=409) | Turkish version of eHEALS | Adolescent Health Promotion Scale | Diet, life appreciation, social support, exercise, stress management, and health responsibility | 8 |
| Lee et al (2017) [54] | Korea | Adults aged 20 to 59 years (n=195) | Adapted eHEALS | Adapted HPLP Ⅱ | Health responsibility, physical activity, nutrition, spiritual development, interpersonal support, and stress management | 7 |
| Li et al (2021) [44] | China | Older adults aged over 60 years (n=2300) | Chinese version of eHEALS | HPLP | Self-actualization, health responsibility, exercise, nutrition, interpersonal support, and stress management | 8 |
| Li and Liu (2020) [55] | China | Internet users aged 20 to 60 years (n=802) | Chinese version of eHEALS | Self-developed 10-item protective behaviors measurement scale | COVID-19 prevention behaviors | 7 |
| Lin et al (2020) [41] | Iran | Older adults aged over 65 years with heart failure (n=468) | Persian version of eHEALS | 5-item self-reported Medication Adherence Report Scale | Medication adherence | 7 |
| Mitsutake et al (2012) [56] | Japan | Adult internet users aged 20 to 59 years (n=2970) | Japanese version of eHEALS | A question with “Yes” or “No” answer | Colorectal cancer screening test | 7 |
| Mitsutake et al (2016) [57] | Japan | Internet users aged 20 to 59 years (n=2115) | Japanese version of eHEALS | Self-developed questions | Cigarette smoking, physical exercise, alcohol consumption, sleeping hours, and dietary habits | 5 |
| Nam and Jung (2020) [36] | Korea | Korean and Chinese university students (n=240) | Adapted eHEALS | 15-item Adapted Health Behavior Scale | Diet, exercise, and sleep behaviors | 4 |
| Park et al (2014) [58] | United States | Adults aged over 18 years who had experience using the internet (n=108) | eHEALS | A question with “Yes” or “No” answer | Breast, cervical, colorectal, or prostate cancer screening tests | 3 |
| Rabenbauer and Mevenkamp (2021) [59] | Germany and Austria | Facebook users aged over 18 years (n=224) | eHEALS | Healthy lifestyle and personal control questionnaire | Diet, daily time management, physical exercise, social support, and positive thinking | 5 |
| Ryu (2019) [45] | Korea | Older adults aged over 65 years (n=99) | Korean version of eHEALS | A tool for measuring the health behavior of elderly people | Diet, exercise, restriction of cigarette smoking or alcohol use, stress management, and disease prevention | 7 |
| Song and Shin (2020) [46] | Korea | Older adults aged over 65 years using the internet (n=102) | Korean version of eHEALS | Adapted HPLP Ⅱ | Health responsibility, physical activity, nutrition, spiritual development, interpersonal support, and stress management | 8 |
| Tariq et al (2020) [37] | Pakistan | College students (n=505) | eHEALS | Self-developed and validated questions on health behaviors | Physical activity and use of dietary supplements | 4 |
| Tsukahara S et al (2020) [38] | Japan | University students (n=3183) | Japanese version of eHEALS | Self-developed questions | Exercise, breakfast, smoking, alcohol consumption, and hours of sleep | 6 |
| Yang et al (2017) [39] | Taiwan | College students (n=556) | eHLS | Health-Promoting Lifestyle Scale | Self-actualization, health responsibility, interpersonal support, exercise, nutrition, and stress management | 8 |
| Yang et al (2019) [40] | Taiwan | College students (n=813) | eHLS | 14-item Dietary Behaviors Scale | Dietary habits | 7 |
aeHL: eHealth literacy.
beHEALS: eHealth Literacy Scale.
cHPLP: Health-Promoting Lifestyle Profile.
deHLS: 12-item eHealth Literacy Scale.
In 25 out of the 29 studies, the original eHEALS (comprising an 8-item questionnaire with a 5-point Likert scale) or its language or culturally adapted versions for respective countries were used. In the studies analyzed, versions of the eHEALS adapted into Korean, Chinese, Turkish, Japanese, and Persian that were undergoing a reliability test were used. Among the 4 studies that used measurement tools other than the eHEALS, 3 studies [33,39,40] used the 12-item eHealth Literacy Scale (eHLS) and 1 study [35] used a 51-item eHealth Literacy Scale developed and validated in Korean.
Health-related behaviors considered to be correlated with eHealth literacy included health-promoting behavior, health-supporting behavior, and disease management behavior. HPLP Ⅱ was the most frequently used tool for measuring health-promoting behavior. The Short-form HPLP, Health-Promoting Lifestyle Scale, and Adolescent Health Promotion Scale were used alongside. Health-supporting behaviors included a regular and balanced diet, appropriate physical activity, sufficient sleep, abstinence, smoking cessation, vaccination, safe sex life, prevention of infectious diseases, cancer screening experience, and positive thinking. These behaviors were comprehensively assessed using various tools, including the Health-related Behavior Scale, Healthy Lifestyle and Personal Control Questionnaire, and Dietary Behaviors Scale, as well as self-developed items. Disease management behaviors included heart failure self-management, diabetes self-management, chronic disease self-management, and medication adherence. Disease management behaviors were measured using validated tools specific to each disease (Table 2).
Risk of Bias Assessment
The risk of bias assessment revealed that 15 studies had a low risk of bias and 12 studies had an unclear risk of bias (Table 2). Two studies [34,58] were found to have a high risk of bias with a NOS score of 3, and both studies were confirmed to have selection biases, such as representativeness of the study population, calculation of the sample size, and proportion of nonresponders. The high risk of bias in the 2 studies was also attributed to the failure to control confounding variables and to use validated tools for measuring health-related behaviors (Multimedia Appendix 3).
Qualitative Analysis of eHealth Literacy and Health-Related Behaviors
Among the 29 included studies, 6 showed that not all health-related behaviors were significantly associated with eHealth literacy [36-38,48,51,58] and 1 demonstrated a negative effect of eHealth literacy on health-related behaviors [47]. Significant associations were not found between the eHEALS score and disease management behaviors in hypertension patients [48], and between the eHEALS score and health-promoting behaviors or health-supporting behaviors in cancer patients [51,58] or college students [36,37]. In a study with Japanese university students [38], the eHEALS score was positively associated with some behaviors, such as regular exercise and breakfast eating, but was not associated with behaviors related to sleeping, smoking, and drinking. A study with HIV-infected low-income women [47] identified that higher eHealth literacy was significantly associated with HIV transmission risk behaviors. In the remaining 22 out of 29 studies, positive associations were present between eHealth literacy and health-related behaviors, that is, individuals with higher eHealth literacy scores were reported to show higher scores in health-promoting behaviors [31,32,35,39,43,44,46,54], regular eating and exercise [33,34,38,40,42,45,57,59], sufficient sleep [33,34,38,57], stress management [42,45], smoking cessation [34,38,45,57], alcohol abstinence [34,38,45,57], compliance with disease-prevention behaviors [45,52,55,56], medication adherence [41], self-care management of heart failure [49], and self-care management for diabetes [50]. The relationship between eHealth literacy and health-related behaviors in the included studies is summarized in Multimedia Appendix 4.
Quantitative Analysis of eHealth Literacy and Health-Related Behaviors
Correlation Between eHealth Literacy and Health-Related Behaviors by Population Characteristics and Types of Health-Related Behaviors
The correlation coefficients between eHealth literacy and health-related behaviors in the studies [31, 35, 41-43, 45, 46, 48-51, 54, 55, 59] included in the meta-analysis ranged from 0.14 to 0.45. Among these studies, the correlation between eHealth literacy and health-related behaviors was synthesized by age, morbidity status, and types of health-related behaviors. From the age subgroups, the pooled estimates of correlation coefficients were 0.28 (95% CI 0.22-0.34) and 0.37 (95% CI 0.29-0.44) for studies in which participants’ mean age was <65 years and ≥65 years, respectively. While the pooled correlation coefficient of the patient group was estimated at 0.28 (95% CI 0.17-0.39), that of the nonpatient group was 0.32 (95% CI 0.25-0.39). For the subtypes of health-related behaviors, the highest effect size of the pooled correlation coefficient was shown by health-promoting behavior (0.36, 95% CI 0.27-0.41), and the lowest was shown by disease management behavior (0.24, 95% CI 0.12-0.35) (Table 3).
Table 3.
Correlation between eHealth literacy and health-related behaviors by age, morbidity status, and type of health-related behavior.
| Characteristic | Studies, n | Pooled correlation coefficient, value (95% CI) | |||
| Age |
|
|
|||
|
|
<65 years | 9 | 0.28 (0.22-0.34) | ||
|
|
≥65 years | 5 | 0.37 (0.29-0.44) | ||
| Morbidity status |
|
|
|||
|
|
Patients | 4 | 0.28 (0.17-0.39) | ||
|
|
Nonpatients | 10 | 0.32 (0.25-0.39) | ||
| Type of health-related behavior |
|
|
|||
|
|
Health-promoting behavior | 7 | 0.36 (0.27-0.41) | ||
|
|
Health-supporting behavior | 3 | 0.31 (0.19-0.42) | ||
|
|
Disease management behavior | 4 | 0.24 (0.12-0.35) | ||
Overall Estimate of the Correlation Between eHealth Literacy and Health-Related Behaviors
The overall estimate of the correlation between eHealth literacy and health-related behaviors was conducted for all 14 studies available for quantitative analysis. The pooled correlation coefficient was 0.31 (95% CI 0.25-0.34; P<.001), with high heterogeneity (Cochrane Q=51.34; P<.001; I2=72.73%), which indicated a moderate correlation [30] between eHealth literacy and health-related behaviors (Figure 2).
Figure 2.
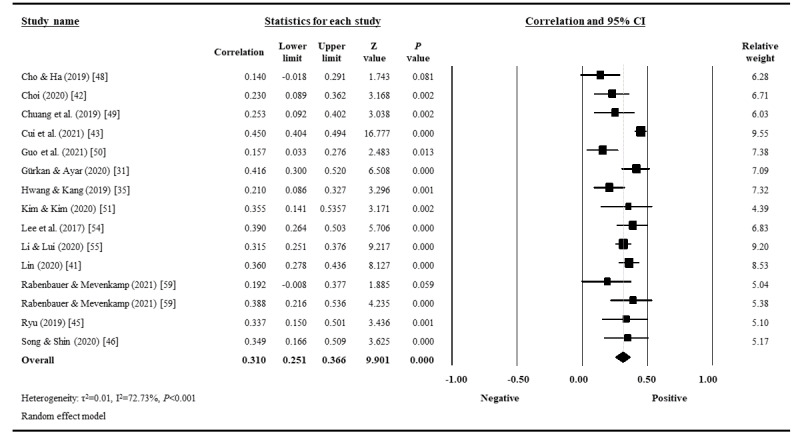
Forest plot of the correlation coefficients between eHealth literacy and health-related behaviors.
Regarding publication bias, slight asymmetry in visual analysis using a funnel plot was observed (Figure 3), and a weak but statistically significant asymmetry was verified in the Egger regression test (P=.049). In further trim-and-fill analysis, no studies were found to require further transformation to symmetry, and consequently, no changes in the size effect occurred, indicating that the publication bias did not affect the validity of the study results.
Figure 3.
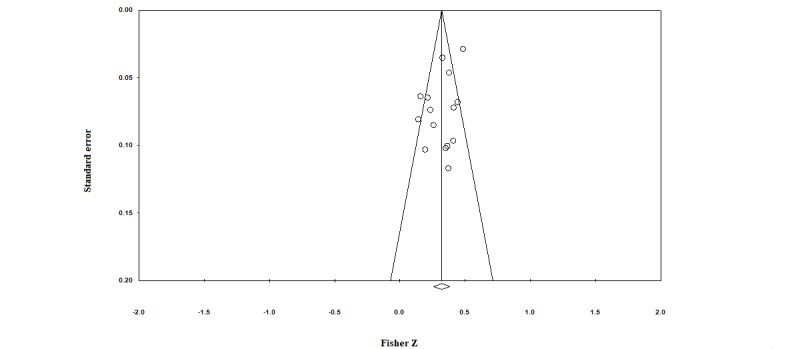
Funnel plot of the correlation between eHealth literacy and health-related behaviors.
Discussion
Prior Work and Principal Findings
The pursuit of health information can affect various health-related outcomes, such as disease prevention actions, perceived health status, and use of health care medical services [60]. With access to and sharing of an enormous amount of health information through the internet in the general population, the concept of eHealth literacy has been studied as a mediator in the process from online health information acquisition to changing individual health-related behaviors [61-63]. Therefore, health care professionals need to have an in-depth understanding of eHealth literacy and its effects on health-related behaviors. In previous studies, concerns were raised that a lower eHealth literacy level was associated with greater difficulty in accessing and understanding online health information, making it more difficult for affected individuals to manage their chronic diseases and to comply with disease prevention actions such as cancer screening [64,65]. However, eHealth literacy may not necessarily have a positive effect on health behaviors or disease-prevention behaviors. A study by Aharony and Goldman [66] found that the group that hesitated to get vaccinated had a higher frequency and intensity of using online information sources. Since eHealth literacy can have a multifaceted effect on health-related behaviors, a more comprehensive analysis is needed to gain an in-depth understanding of the correlation between eHealth literacy and health-related behaviors.
Our meta-analysis showed a moderately positive correlation between eHealth literacy and health-related behaviors, and eHealth literacy was found to have a significant effect on health-related behaviors such as health-promoting behavior, health-supporting behavior, and disease management behavior. However, some of the studies, which specifically focused on younger age groups and were not included in the meta-analysis, showed no association or rather a negative association [36,38,47,58]. Therefore, the effect of eHealth literacy on health-related behaviors should be carefully interpreted, and the possibility of other factors mediating the relationship between eHealth literacy and health-related behaviors should be taken into account. As eHealth literacy alone cannot explain the correlation between online health information acquisition and health-related behaviors, additional research is needed to identify other factors.
In the results of the quantitative analysis by age, the younger population showed a relatively weak correlation between eHealth literacy and health-related behaviors, while the older population showed a moderate correlation. These results might suggest that health-related behaviors in the younger population are influenced by other factors, such as perceived health status and interest in health, going beyond the level of merely obtaining health information [67]. According to previous studies, health literacy among older adults was positively associated with health-related behaviors [68,69], and a computer-based health literacy intervention conducted for elderly people improved participation in their own health care [70]. Considering the results of previous studies and our meta-analysis, eHealth literacy can act as a mediator in changing health-related behaviors using online health information in older adults. Moreover, the older population aged ≥65 years showed a lower level of eHealth literacy than those aged <65 years in previous studies [63,71]. Thus, efforts are needed to promote the level of eHealth literacy in older adults, which is expected to contribute to the promotion of positive health-related behaviors in this population.
The correlation coefficient between eHealth literacy and health-related behaviors was lower in the patient group than in the nonpatient group. Since patients were reported to have more opportunities to obtain health information from various sources, including their doctors or health care providers, when compared with the general population [72], we believe that health-related behaviors showed a relatively low correlation with eHealth literacy in the patient group. The number of patients who find and use health information on the internet is increasing [73-75], and patients’ eHealth literacy can influence their health-related decision-making process and health care provider-patient communication [76,77]. Therefore, the low correlation between eHealth literacy and health-related behaviors should not be interpreted as a finding of overlooking the importance of a patient’s eHealth literacy.
In the quantitative analysis by subtypes of health-related behaviors, a correlation between eHealth literacy and health-promoting behavior was most frequently observed (n=7), and its effect size was also the largest. In contrast, a weak correlation was observed between eHealth literacy and disease management behavior, and the context was similar to that in the patient subgroup. Therefore, improvement in eHealth literacy is expected to greatly contribute to boosting the level of health-promoting behaviors such as eating habits, exercise, stress management, health responsibility, interpersonal relationships, and internal growth. Moreover, it would be beneficial to consider individual eHealth literacy levels when health care professionals provide eHealth services related to health-promoting behaviors.
Strengths and Limitations
In this study, eHealth literacy–related studies were systematically reviewed and comprehensively summarized. In addition, a pooled effect size was derived for the correlation between eHealth literacy and health-related behaviors using a meta-analysis. This study is significant in that it comprehensively presented the characteristics of the research subjects to be considered for understanding eHealth literacy and provided a resource framework regarding the role of eHealth literacy in health-related behaviors and decision-making. The results of this study suggest that health care providers can manage people’s health behaviors and promote health more effectively by providing eHealth care services that consider individuals’ eHealth literacy. In addition, the moderate correlation between eHealth literacy and health-related behaviors supports the importance of eHealth literacy in the process of health care delivery.
Several limitations of the study should be considered when interpreting the findings. First, the sample size of each study included in the meta-analysis was small, and pooled estimates of the correlation coefficient showed high heterogeneity. Due to this limitation, there is a lack of generalizability, and additional research on eHealth literacy and health behaviors is required to support the results. Second, only studies that provided results in the form of correlation coefficients were included in the meta-analysis. Specifically, studies that presented the relationship between eHealth literacy and health-related behaviors in the form of regression coefficients could not be included in quantitative synthesis to estimate the pooled correlation coefficient. Therefore, the causal relationship between eHealth literacy and health behaviors could not be verified in the study, and further meta-analyses need to be performed on the data to demonstrate the effectiveness of eHealth literacy enhancement programs and the resultant changes in health-related behaviors. Third, the eHealth literacy and health-related behavior measurement items used in the included studies varied, which in turn might have led to biased analysis results. Moreover, the eHealth literacy measurement tools of the included studies, such as eHEALS, were developed in the Web 2.0 era and could not fully assess the concept of Web 3.0. Therefore, it is necessary to consider these points when interpreting the results of this study and applying them to practice. Further studies are needed to better explain the relationship between eHealth literacy and health-related behaviors by using measurement tools that are standardized and appropriate in the Web 3.0 era.
Conclusion
In this study, a systematic literature review was conducted on the studies investigating the association between eHealth literacy and health-related behaviors, and a meta-analysis was performed on the results of quantitatively synthesizable cross-sectional studies. Our study found that eHealth literacy has fairly significant positive correlations with health-related behaviors such as self-management behavior, medication adherence, disease management, and prevention actions. Among health-related behaviors, health-promoting behavior was observed to have the highest correlation with eHealth literacy. The findings from our study indicate that eHealth literacy can be a mediator in the process by which health-related information leads to changes in health-related behaviors. Larger-scale studies with stronger validity are needed to evaluate the detailed relationship between the proficiency level of eHealth literacy and health-related behaviors for health promotion in the future.
Acknowledgments
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (The Ministry of Science and ICT [Information and Communications Technology]) (number: 2020R1A2C1101560) and the fourth phase of the Brain Korea 21 Program in 2022.
Abbreviations
- eHEALS
eHealth Literacy Scale
- HPLP
Health-Promoting Lifestyle Profile
- NOS
Newcastle-Ottawa Scale
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 checklist.
Search strategy.
Risk of bias assessment for the included studies using the modified Newcastle-Ottawa Scale.
The relationship between eHealth literacy and health-related behaviors in the included studies.
Footnotes
Authors' Contributions: KK, SS, SK, and EL conceived and designed this study. All authors participated in the selection of studies and acquisition of data. KK, SK, and EL analyzed and interpreted the data. KK, SK, and EL wrote the original draft. All authors reviewed and revised the manuscript. SK and EL equally served as corresponding authors.
Conflicts of Interest: None declared.
References
- 1.Fox S, Duggan M. Health Online 2013: Information Triage. Pew Research Center. [2021-09-04]. http://www.pewinternet.org/2013/01/15/information-triage/
- 2.Jadad AR, Gagliardi A. Rating health information on the Internet: navigating to knowledge or to Babel? JAMA. 1998 Mar 25;279(8):611–4. doi: 10.1001/jama.279.8.611.jrv71042 [DOI] [PubMed] [Google Scholar]
- 3.Ha Y, Ryu S. Usage of health information on the internet. Health and Welfare Policy Forum. 2004;11:71–87. doi: 10.23062/2004.11.7. [DOI] [Google Scholar]
- 4.Win KT, Hassan NM, Bonney A, Iverson D. Benefits of online health education: perception from consumers and health professionals. J Med Syst. 2015 Mar 11;39(3):27. doi: 10.1007/s10916-015-0224-4. [DOI] [PubMed] [Google Scholar]
- 5.Baskerville NB, Azagba S, Norman C, McKeown K, Brown KS. Effect of a Digital Social Media Campaign on Young Adult Smoking Cessation. Nicotine Tob Res. 2016 Mar;18(3):351–60. doi: 10.1093/ntr/ntv119.ntv119 [DOI] [PubMed] [Google Scholar]
- 6.Benetoli A, Chen TF, Aslani P. The use of social media in pharmacy practice and education. Res Social Adm Pharm. 2015;11(1):1–46. doi: 10.1016/j.sapharm.2014.04.002.S1551-7411(14)00038-2 [DOI] [PubMed] [Google Scholar]
- 7.Chang T, Chopra V, Zhang C, Woolford SJ. The role of social media in online weight management: systematic review. J Med Internet Res. 2013 Dec 28;15(11):e262. doi: 10.2196/jmir.2852. https://www.jmir.org/2013/11/e262/ v15i11e262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fast AM, Deibert CM, Hruby GW, Glassberg KI. Evaluating the quality of Internet health resources in pediatric urology. J Pediatr Urol. 2013 May;9(2):151–6. doi: 10.1016/j.jpurol.2012.01.004.S1477-5131(12)00007-1 [DOI] [PubMed] [Google Scholar]
- 9.Health Literacy in Healthy People 2030. US Department of Health & Human Services, Office of Disease Prevention and Health Promotion. [2021-09-04]. https://health.gov/our-work/national-health-initiatives/healthy-people/healthy-people-2030/health-literacy-healthy-people-2030 .
- 10.Norman CD, Skinner HA. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res. 2006 Jul 16;8(2):e9. doi: 10.2196/jmir.8.2.e9. https://www.jmir.org/2006/2/e9/ v8i2e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011 Jul 19;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005.155/2/97 [DOI] [PubMed] [Google Scholar]
- 12.Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med. 2013 Mar 13;28(3):444–52. doi: 10.1007/s11606-012-2241-z. https://europepmc.org/abstract/MED/23065575 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim S, Oh J, Lee Y. Health Literacy: An Evolutionary Concept Analysis. Journal of Korean Academic Society of Nursing Education. 2013;19(4):558–570. doi: 10.5977/jkasne.2013.19.4.558. [DOI] [Google Scholar]
- 14.Lee J, Lee E, Chae D. eHealth Literacy Instruments: Systematic Review of Measurement Properties. J Med Internet Res. 2021 Dec 15;23(11):e30644. doi: 10.2196/30644. https://www.jmir.org/2021/11/e30644/ v23i11e30644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: A systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care. 2016;41(1):1–19. doi: 10.3109/17538157.2014.948171. [DOI] [PubMed] [Google Scholar]
- 16.Stellefson M, Hanik B, Chaney B, Chaney D, Tennant B, Chavarria EA. eHealth literacy among college students: a systematic review with implications for eHealth education. J Med Internet Res. 2011 Dec 01;13(4):e102. doi: 10.2196/jmir.1703. https://www.jmir.org/2011/4/e102/ v13i4e102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arcury TA, Sandberg JC, Melius KP, Quandt SA, Leng X, Latulipe C, Miller DP, Smith DA, Bertoni AG. Older Adult Internet Use and eHealth Literacy. J Appl Gerontol. 2020 Mar;39(2):141–150. doi: 10.1177/0733464818807468. https://europepmc.org/abstract/MED/30353776 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Santana S, Lausen B, Bujnowska-Fedak M, Chronaki CE, Prokosch H, Wynn R. Informed citizen and empowered citizen in health: results from an European survey. BMC Fam Pract. 2011 May 16;12(1):20. doi: 10.1186/1471-2296-12-20. https://bmcfampract.biomedcentral.com/articles/10.1186/1471-2296-12-20 .1471-2296-12-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norman CD, Skinner HA. eHEALS: The eHealth Literacy Scale. J Med Internet Res. 2006 Dec 14;8(4):e27. doi: 10.2196/jmir.8.4.e27. https://www.jmir.org/2006/4/e27/ v8i4e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gochman DS. Health Behavior Research. In: Gochman DS, editor. Health Behavior. Boston, MA: Springer; 1988. pp. 409–424. [Google Scholar]
- 21.Walker SN, Sechrist K, Pender N. Lifestyle Profile HPLP II. University of Michigan Library. 1995. [2021-11-21]. https://deepblue.lib.umich.edu/bitstream/handle/2027.42/85349/HPLP_II-English_Version.pdf .
- 22.Darviri C, Alexopoulos EC, Artemiadis AK, Tigani X, Kraniotou C, Darvyri P, Chrousos GP. The Healthy Lifestyle and Personal Control Questionnaire (HLPCQ): a novel tool for assessing self-empowerment through a constellation of daily activities. BMC Public Health. 2014 Oct 24;14(1):995. doi: 10.1186/1471-2458-14-995. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-14-995 .1471-2458-14-995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riegel B, Lee CS, Dickson VV, Carlson B. An update on the self-care of heart failure index. J Cardiovasc Nurs. 2009;24(6):485–97. doi: 10.1097/JCN.0b013e3181b4baa0. https://europepmc.org/abstract/MED/19786884 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walker SN, Sechrist KR, Pender NJ. The Health-Promoting Lifestyle Profile. Nursing Research. 1987;36(2):76–81. doi: 10.1097/00006199-198703000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Short SE, Mollborn S. Social Determinants and Health Behaviors: Conceptual Frames and Empirical Advances. Curr Opin Psychol. 2015 Oct;5:78–84. doi: 10.1016/j.copsyc.2015.05.002. https://europepmc.org/abstract/MED/26213711 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33782057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute. [2021-09-26]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm .
- 28.Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013 Mar 19;13:154. doi: 10.1186/1471-2458-13-154. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-154 .1471-2458-13-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins JPT. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008 Oct 02;37(5):1158–60. doi: 10.1093/ije/dyn204.dyn204 [DOI] [PubMed] [Google Scholar]
- 30.Cohen J. A power primer. Psychological Bulletin. 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 31.Gürkan KP, Ayar D. The Impact of e-Health Literacy on Health Promotion Behaviors of High School Students. J Pediatr Res. 2020 Jul 8;7(4):286–292. doi: 10.4274/jpr.galenos.2019.81488. [DOI] [Google Scholar]
- 32.Korkmaz Aslan G, Kartal A, Turan T, Taşdemir Yiğitoğlu G, Kocakabak C. Association of electronic health literacy with health-promoting behaviours in adolescents. Int J Nurs Pract. 2021 May 22;27(2):e12921. doi: 10.1111/ijn.12921. [DOI] [PubMed] [Google Scholar]
- 33.Hsu W, Chiang C, Yang S. The effect of individual factors on health behaviors among college students: the mediating effects of eHealth literacy. J Med Internet Res. 2014 Dec 12;16(12):e287. doi: 10.2196/jmir.3542. https://www.jmir.org/2014/12/e287/ v16i12e287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Britt RK, Collins WB, Wilson K, Linnemeier G, Englebert AM. eHealth Literacy and Health Behaviors Affecting Modern College Students: A Pilot Study of Issues Identified by the American College Health Association. J Med Internet Res. 2017 Dec 19;19(12):e392. doi: 10.2196/jmir.3100. https://www.jmir.org/2017/12/e392/ v19i12e392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hwang AR, Kang H. Influence of eHealth Literacy on Health Promoting Behaviors among University Students. Journal of the Korean Society of School Health. 2019;32(3):165–174. doi: 10.15434/kssh.2019.32.3.165. [DOI] [Google Scholar]
- 36.Nam YH, Jung IS. A Comparative Study on the Effect of e-Health Literacy, Health Information Reliability and Health Behavior on the Health Information Use Motive in Korean and Chinese University Students. dcs. 2020 Mar 31;21(3):513–520. doi: 10.9728/dcs.2020.21.3.513. [DOI] [Google Scholar]
- 37.Tariq A, Khan SR, Basharat A. Internet Use, eHealth Literacy, and Dietary Supplement Use Among Young Adults in Pakistan: Cross-Sectional Study. J Med Internet Res. 2020 Jul 10;22(6):e17014. doi: 10.2196/17014. https://www.jmir.org/2020/6/e17014/ v22i6e17014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsukahara S, Yamaguchi S, Igarashi F, Uruma R, Ikuina N, Iwakura K, Koizumi K, Sato Y. Association of eHealth Literacy With Lifestyle Behaviors in University Students: Questionnaire-Based Cross-Sectional Study. J Med Internet Res. 2020 Jul 24;22(6):e18155. doi: 10.2196/18155. https://www.jmir.org/2020/6/e18155/ v22i6e18155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang S, Luo Y, Chiang C. The Associations Among Individual Factors, eHealth Literacy, and Health-Promoting Lifestyles Among College Students. J Med Internet Res. 2017 Jan 10;19(1):e15. doi: 10.2196/jmir.5964. https://www.jmir.org/2017/1/e15/ v19i1e15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang SC, Luo YF, Chiang C. Electronic Health Literacy and Dietary Behaviors in Taiwanese College Students: Cross-Sectional Study. J Med Internet Res. 2019 Dec 26;21(11):e13140. doi: 10.2196/13140. https://www.jmir.org/2019/11/e13140/ v21i11e13140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin C, Ganji M, Griffiths MD, Bravell ME, Broström A, Pakpour AH. Mediated effects of insomnia, psychological distress and medication adherence in the association of eHealth literacy and cardiac events among Iranian older patients with heart failure: a longitudinal study. Eur J Cardiovasc Nurs. 2020 Mar 13;19(2):155–164. doi: 10.1177/1474515119873648. [DOI] [PubMed] [Google Scholar]
- 42.Choi M. Association of eHealth Use, Literacy, Informational Social Support, and Health-Promoting Behaviors: Mediation of Health Self-Efficacy. Int J Environ Res Public Health. 2020 Oct 28;17(21):7890. doi: 10.3390/ijerph17217890. https://www.mdpi.com/resolver?pii=ijerph17217890 .ijerph17217890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cui G, Li S, Yin Y, Chen L, Li J, Liang F, Liu X, Chen L. The relationship among social capital, eHealth literacy and health behaviours in Chinese elderly people: a cross-sectional study. BMC Public Health. 2021 Jan 06;21(1):45. doi: 10.1186/s12889-020-10037-4. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-10037-4 .10.1186/s12889-020-10037-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li S, Cui G, Yin Y, Wang S, Liu X, Chen L. Health-promoting behaviors mediate the relationship between eHealth literacy and health-related quality of life among Chinese older adults: a cross-sectional study. Qual Life Res. 2021 Aug;30(8):2235–2243. doi: 10.1007/s11136-021-02797-2. https://europepmc.org/abstract/MED/33661455 .10.1007/s11136-021-02797-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ryu H. Seoul National University Library. Seoul, South Korea: Seoul National University; 2019. [2022-12-31]. The association between e-Health literacy and health behaviors in elderly people [master's thesis] https://s-space.snu.ac.kr/handle/10371/150537 . [Google Scholar]
- 46.Song J, Shin S. The Effects of e-Health Literacy and Subjective Health Status on Health-seeking Behaviors of Elderly Using the Internet in the Community. Journal of Digital Convergence. 2020;18(1):321–332. doi: 10.14400/JDC.2020.18.1.321. [DOI] [Google Scholar]
- 47.Blackstock OJ, Cunningham CO, Haughton LJ, Garner RY, Norwood C, Horvath KJ. Higher eHealth Literacy is Associated With HIV Risk Behaviors among HIV-Infected Women Who Use the Internet. J Assoc Nurses AIDS Care. 2016;27(1):102–8. doi: 10.1016/j.jana.2015.09.001. https://europepmc.org/abstract/MED/26456347 .S1055-3290(15)00202-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cho GY, Ha MN. Mediating Effects of Health Belief on the Correlations among Disease-related Knowledge, eHealth Literacy, and Self-care Behaviors in Outpatients with Hypertension. Korean J Adult Nurs. 2019;31(6):638–649. doi: 10.7475/kjan.2019.31.6.638. [DOI] [Google Scholar]
- 49.Chuang H, Kao C, Lin W, Chang Y. Factors Affecting Self-care Maintenance and Management in Patients With Heart Failure. J Cardiovasc Nurs. 2019 Apr 17;34(4):297–305. doi: 10.1097/jcn.0000000000000575. [DOI] [PubMed] [Google Scholar]
- 50.Guo SH, Hsing H, Lin J, Lee C. Relationships Between Mobile eHealth Literacy, Diabetes Self-care, and Glycemic Outcomes in Taiwanese Patients With Type 2 Diabetes: Cross-sectional Study. JMIR Mhealth Uhealth. 2021 Mar 05;9(2):e18404. doi: 10.2196/18404. https://mhealth.jmir.org/2021/2/e18404/ v9i2e18404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim HJ, Kim M. Comparison Study of e-Health Literacy and Health Promoting Behaviors of Cancer Patients and Nurses. Asian Oncol Nurs. 2020;20(2):100–109. doi: 10.5388/aon.2020.20.2.100. [DOI] [Google Scholar]
- 52.An L, Bacon E, Hawley S, Yang P, Russell D, Huffman S, Resnicow K. Relationship Between Coronavirus-Related eHealth Literacy and COVID-19 Knowledge, Attitudes, and Practices among US Adults: Web-Based Survey Study. J Med Internet Res. 2021 Mar 29;23(3):e25042. doi: 10.2196/25042. https://www.jmir.org/2021/3/e25042/ v23i3e25042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim S, Son Y. Relationships Between eHealth Literacy and Health Behaviors in Korean Adults. Comput Inform Nurs. 2017 Mar;35(2):84–90. doi: 10.1097/CIN.0000000000000255. [DOI] [PubMed] [Google Scholar]
- 54.Lee S, Son H, Lee D, Kang H. The Influence of e-Health Literacy, Subjective Health Status, and Health Information Seeking Behavior on the Internet on Health Promoting Behavior. KSW. 2017;12(4):55–67. doi: 10.21097/ksw.2017.11.12.4.55. [DOI] [Google Scholar]
- 55.Li X, Liu Q. Social Media Use, eHealth Literacy, Disease Knowledge, and Preventive Behaviors in the COVID-19 Pandemic: Cross-Sectional Study on Chinese Netizens. J Med Internet Res. 2020 Oct 09;22(10):e19684. doi: 10.2196/19684. https://www.jmir.org/2020/10/e19684/ v22i10e19684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mitsutake S, Shibata A, Ishii K, Oka K. Association of eHealth literacy with colorectal cancer knowledge and screening practice among internet users in Japan. J Med Internet Res. 2012 Dec 13;14(6):e153. doi: 10.2196/jmir.1927. https://www.jmir.org/2012/6/e153/ v14i6e153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mitsutake S, Shibata A, Ishii K, Oka K. Associations of eHealth Literacy With Health Behavior Among Adult Internet Users. J Med Internet Res. 2016 Jul 18;18(7):e192. doi: 10.2196/jmir.5413. https://www.jmir.org/2016/7/e192/ v18i7e192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Park H, Moon M, Baeg JH. Association of eHealth literacy with cancer information seeking and prior experience with cancer screening. Comput Inform Nurs. 2014 Oct;32(9):458–63. doi: 10.1097/CIN.0000000000000077. [DOI] [PubMed] [Google Scholar]
- 59.Rabenbauer LM, Mevenkamp N. Factors in the Effectiveness of e-Health Interventions for Chronic Back Pain: How Self-Efficacy Mediates e-Health Literacy and Healthy Habits. Telemed J E Health. 2021 Mar 01;27(2):184–192. doi: 10.1089/tmj.2019.0301. [DOI] [PubMed] [Google Scholar]
- 60.Basu A, Dutta MJ. Participatory change in a campaign led by sex workers: connecting resistance to action-oriented agency. Qual Health Res. 2008 Jan 01;18(1):106–19. doi: 10.1177/1049732307309373.18/1/106 [DOI] [PubMed] [Google Scholar]
- 61.Lee K, Hoti K, Hughes JD, Emmerton LM. Consumer Use of "Dr Google": A Survey on Health Information-Seeking Behaviors and Navigational Needs. J Med Internet Res. 2015 Dec 29;17(12):e288. doi: 10.2196/jmir.4345. https://www.jmir.org/2015/12/e288/ v17i12e288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ritterband LM, Thorndike FP, Cox DJ, Kovatchev BP, Gonder-Frederick LA. A behavior change model for internet interventions. Ann Behav Med. 2009 Aug;38(1):18–27. doi: 10.1007/s12160-009-9133-4. https://europepmc.org/abstract/MED/19802647 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Neter E, Brainin E. eHealth literacy: extending the digital divide to the realm of health information. J Med Internet Res. 2012 Jan 27;14(1):e19. doi: 10.2196/jmir.1619. https://www.jmir.org/2012/1/e19/ v14i1e19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002 May;40(5):395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 65.Davis TC, Gazmararian J, Kennen EM. Approaches to improving health literacy: lessons from the field. J Health Commun. 2006 Oct 23;11(6):551–4. doi: 10.1080/10810730600835517.M37T888858H68827 [DOI] [PubMed] [Google Scholar]
- 66.Aharony N, Goldman R. E-health literacy and the vaccination dilemma: an Israeli perspective. Information Research. 2017;22(2):paper751. http://informationr.net/ir/22-2/paper751.html . [Google Scholar]
- 67.Kim B, Jung M, Han C. Health Promoting Behavior of University Students and Related Factors. Korean Journal of Health Education and Promotion. 2002;19(1):59–85. https://koreascience.kr/article/JAKO200211922619422.page . [Google Scholar]
- 68.Jeong JH, Kim JS. Health Literacy, Health Risk Perception and Health Behavior of Elders. J Korean Acad Community Health Nurs. 2014;25(1):65. doi: 10.12799/jkachn.2014.25.1.65. [DOI] [Google Scholar]
- 69.Xie B. Older adults, e-health literacy, and collaborative learning: An experimental study. J. Am. Soc. Inf. Sci. 2011 Mar 14;62(5):933–946. doi: 10.1002/asi.21507. [DOI] [Google Scholar]
- 70.Xie B. Improving older adults' e-health literacy through computer training using NIH online resources. Libr Inf Sci Res. 2012 Jan 01;34(1):63–71. doi: 10.1016/j.lisr.2011.07.006. https://europepmc.org/abstract/MED/22639488 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tennant B, Stellefson M, Dodd V, Chaney B, Chaney D, Paige S, Alber J. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J Med Internet Res. 2015 Mar 17;17(3):e70. doi: 10.2196/jmir.3992. https://www.jmir.org/2015/3/e70/ v17i3e70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Marrie RA, Salter AR, Tyry T, Fox RJ, Cutter GR. Preferred sources of health information in persons with multiple sclerosis: degree of trust and information sought. J Med Internet Res. 2013 Mar 17;15(4):e67. doi: 10.2196/jmir.2466. https://www.jmir.org/2013/4/e67/ v15i4e67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bundorf MK, Wagner TH, Singer SJ, Baker LC. Who searches the internet for health information? Health Serv Res. 2006 Jul;41(3 Pt 1):819–36. doi: 10.1111/j.1475-6773.2006.00510.x. https://europepmc.org/abstract/MED/16704514 .HESR510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Finney Rutten LJ, Agunwamba AA, Wilson P, Chawla N, Vieux S, Blanch-Hartigan D, Arora NK, Blake K, Hesse BW. Cancer-Related Information Seeking Among Cancer Survivors: Trends Over a Decade (2003-2013) J Cancer Educ. 2016 Jul;31(2):348–57. doi: 10.1007/s13187-015-0802-7.10.1007/s13187-015-0802-7 [DOI] [PubMed] [Google Scholar]
- 75.Finney Rutten LJ, Blake KD, Greenberg-Worisek AJ, Allen SV, Moser RP, Hesse BW. Online Health Information Seeking Among US Adults: Measuring Progress Toward a Healthy People 2020 Objective. Public Health Rep. 2019;134(6):617–625. doi: 10.1177/0033354919874074. https://europepmc.org/abstract/MED/31513756 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee BG, Byun WJ, Lim JR. The influence of individual’s e-health literacy on doctor-patient communication. Journal of Cybercommunication Academic Society. 2010;27(3):89–125. https://www.dbpia.co.kr/journal/articleDetail?nodeId=NODE01532835 . [Google Scholar]
- 77.Kim M, Lee J, Doo E. Factors Influencing Healthcare Provider-Patient Communication of Patients with Chronic Diseases. J Korean Acad Nurs Adm. 2020;26(2):73. doi: 10.11111/jkana.2020.26.2.73. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 checklist.
Search strategy.
Risk of bias assessment for the included studies using the modified Newcastle-Ottawa Scale.
The relationship between eHealth literacy and health-related behaviors in the included studies.


