Abstract
Background
There has been longstanding uncertainty over whether lower healthcare spending in Canada might be associated with inferior outcomes for hospital-based care. We hypothesized that mortality and surgical complication rates would be higher for patients who underwent four common surgical procedures in Canada as compared to the US.
Design, Setting, and Participants
We conducted a retrospective cohort study of all adults who underwent hip fracture repair, colectomy, pancreatectomy, or spine surgery in 96 Canadian and 585 US hospitals participating in the American College of Surgeons National Surgical Quality Improvement Project (ACS-NSQIP) between January 1, 2015 and December 31, 2019. We compared patients with respect to demographic characteristics and comorbidity. We then compared unadjusted and adjusted outcomes within 30-days of surgery for patients in Canada and the US including: (1) Mortality; (2) A composite constituting 1-or-more of the following complications (cardiac arrest; myocardial infarction; pneumonia; renal failure/; return to operating room; surgical site infection; sepsis; unplanned intubation).
Results
Our hip fracture cohort consisted of 21,166 patients in Canada (22.3%) and 73,817 in the US (77.7%), for colectomy 21,279 patients in Canada (8.9%) and 218,307 (91.1%), for pancreatectomy 873 (7.8%) in Canada and 12,078 (92.2%) in the US, and for spine surgery 14,088 (5.3%) and 252,029 (94.7%). Patient sociodemographics and comorbidity were clinically similar between jurisdictions. In adjusted analyses odds of death was significantly higher in Canada for two procedures (colectomy (OR 1.22; 95% CI 1.044–1.424; P = .012) and pancreatectomy (OR 2.11; 95% CI 1.26–3.56; P = .005)) and similar for hip fracture and spine surgery. Odds of the composite outcome were significantly higher in Canada for all 4 procedures, largely driven by higher risk of cardiac events and post-operative infections.
Conclusions
We found evidence of higher rates of mortality and surgical complications within 30-days of surgery for patients in Canada as compared to the US.
Introduction
There is growing appreciation of the value of international health system comparisons. [1] A major challenge for such studies has been identifying data sets that allow for valid comparisons. [1, 2] Analyses often have relied upon aggregate data submitted by countries to central repositories such as the World Health Organization or Organization for Economic Cooperation and Development, [3] but these data typically lack the granularity necessary for comparing disease-specific or procedure-specific outcomes. Other studies have used administrative data from multiple countries, [4, 5] but administrative data preclude detailed clinical risk adjustment. An alternative strategy involves using clinical registries, [6, 7] but few registry studies have evaluated surgical procedures.
The growing international reach of the American College of Surgeons National Surgical Quality Improvement Program registry (ACS-NSQIP) affords a unique opportunity to compare surgical outcomes between countries using state-of-the-art data and risk adjustment. [8] The recent growth in NSQIP from a US-focused registry to encompass numerous Canadian hospitals affords a unique opportunity to compare surgical outcomes in these two geopolitically aligned countries with vastly different health care systems. To date, we are aware of only a single study that has used ACS-NSQIP data for comparing US and Canadian surgical care and this study was limited to joint replacement. [9]
In the context of ongoing debates about the tradeoffs in outcomes inherent in the US and Canadian healthcare systems, we set out to compare surgical outcomes for four different surgical procedures.
Methods
Data and patients
We used data from ACS-NSQIP to identify adults who underwent urgent non-traumatic (aka, low impact) hip fracture repair, elective colectomy, elective pancreatectomy, or elective spine surgery between January 1, 2015 and December 31, 2019 at participating hospitals in the USA and Canada. NSQIP is a voluntary registry of more than 700 participating hospitals worldwide (585 in the US, 96 in Canada). For each patient, trained clinical reviewers at each hospital enter more than 300 demographic, clinical, surgery-related, and outcome-related variables, collected from various sources, including patient charts and hospital computer systems, into the NSQIP online data repository. [10] Data elements and collection processes are thoroughly specified and carefully defined. Prior research has demonstrated that NSQIP significantly outperforms administrative data with respect to identification of comorbid conditions and adverse surgical outcomes. [11] We selected adults identified with any of our 4 target procedures using a combination of CPT, ICD9, and ICD-10 codes based upon coding schemes that we and others have used in prior publications; [12–18] a full list of the codes that were used is provided as Appendix Table 1. Additional details of our protocol are available by request from the corresponding author.
Our cohort was limited to age ≥18 years for colectomy, pancreatectomy, and spine surgery and age ≥50 years for hip fracture. We limited our hip fracture cohort to patients undergoing non-elective surgery to hone our focus to patients with an acute fracture. We limited our colectomy, pancreatectomy, and spine surgery to non-emergent cases reflecting the typically pre-planned nature of these procedures.
Analyses
First, we compared demographic characteristics and measures of comorbidity among patients in Canada and the USA using simple bivariate measures for each of our four surgical cohorts. Comorbidity measures included American Society for Anesthesiology (ASA) class (range 1 [healthy] to 5 [moribund, not expected to survive surgery]), current tobacco use, chronic obstructive pulmonary disease (COPD), diabetes, and congestive heart failure (CHF) and whether the procedure was performed in the inpatient setting (or not).
Second, for each patient cohort, we compared patients treated in the USA and Canada with respect to the occurrence of nine individual adverse outcomes within 30-days of surgery. Our first co-primary outcome was mortality; our second co-primary outcome was a composite outcome consisting of one-or-more of the following outcomes within 30-days of surgery: cardiac arrest; myocardial infarction; pneumonia; renal failure/progressive renal insufficiency; return to operating room; surgical site infection; sepsis; unplanned intubation; wound disruption-all as explicitly defined by the ACS-NSQIP. We also compared patients treated in the USA and Canada with respect to hospital length-of-stay (LOS) and hospital readmission within 30-days of surgery. Denominators varied slightly for the calculation of each outcome reflecting rules incorporated into the NSQIP methodology.
Third, for each of our procedures we calculated risk-adjusted odds of each of the outcomes described above, in Canada as compared to the USA (reference). Covariates available for selection included age, sex, country, year of surgery and approximately 40 surgical, comorbidity, and laboratory values. Separate models were fit for each surgical procedure and each outcome. A preliminary logistic model (SAS PROC Logistic) used forward selection (except that country was forced into the model at step 0), from the appropriate initial predictor set, to identify a parsimonious predictor set, which was then used in a follow-up logistic regression (SAS PROC Surveylogistic) that used a generalized estimating equation-type approach to adjust standard errors for the clustering of patients within hospitals. C-statistics for mortality models ranged from 0.76 (pancreatectomy) to 0.86 (spine surgery), while c-statistics for composite outcome models ranged from 0.60 (pancreatectomy) to 0.71 (hip fracture). More detailed information about our statistical methods and models is available by request.
We conducted several sensitivity analyses to check the robustness of our findings. First, after excluding ASA class from our primary models because of implausibly large differences in ASA class between Canada and the USA (with patients in Canada coded as higher complexity likely related to Canadian billing incentives), we re-ran our risk-adjustment models after adding ASA class back into our models; ASA class was important to add back because it is often included in standard ACS-NSQIP risk adjustment models because of its importance as a prediction of outcomes. [19] Second, because of large differences in the proportion of spine surgery procedures performed in the outpatient setting (smaller proportion of outpatient surgery in the USA), we re-ran our statistical models after excluding outpatient spine procedures.
All analyses were conducted on site at the American College of Surgeons central offices using SAS Statistical Software (Cary, NC). This study was deemed exempt by both ACS-NSQIP and the University Health Network research ethics committee.
Results
There were 94,983 patients identified who underwent hip fracture repair (21,166 in Canada [22.3%] and 73,817 in the USA [77.7%]). The colectomy cohort consisted of 239,586 procedures (21,279 [8.9%] and 218,307 [91.1%]), for pancreatectomy 11,205 (873 [7.8%] and 12,078 [92.2%] and for spine surgery 266,117 (14,088 [5.3%] and 252,029 [94.7%]) (Table 1). Patients in Canada were significantly older than their US counterparts for hip fracture repair and colectomy, but age was similar for pancreatectomy and spine surgery (Table 1). Colectomy recipients were significantly less likely to be female in Canada compared to the USA (47.5% vs 52.4%; P <0.001). There were clinically implausible differences in ASA class between patients in Canada and the USA with Canadian patients significantly more likely to be classified as ASA Class 4–5 (extremely sick) than their US counterparts for all procedures. The prevalence of key comorbid conditions, however, was generally similar for patients in Canada and the USA for most conditions and procedures. While virtually all hip fracture, colectomy, and pancreatectomy procedures were inpatients, a significantly larger proportion of spine surgery procedures were inpatient in Canada, while a significantly larger proportion of spine procedures in the USA were outpatient (Table 1). Canada-US differences in sociodemographics and comorbidity generally did not differ for preference insensitive and preference sensitive procedures.
Table 1.
Demographic characteristics and comorbidity of surgical patients in Canada and the USA
| Hip fracture repair | Colectomy | Pancreatectomy | Spine Surgery | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Canada (N = 21,166) | US (N = 73,817) | P-value | Canada (N = 21,276) | US (N = 218,307) | P-value | Canada (N = 873) | US (N = 12,078) | P-value | Canada (N = 14,088) | US (N = 252,029) | P-value | |
| Age, years, mean (SD) | 82.3 | 81.0 | < 0.001 | 66.01 (14.1) | 61.82 (14.9) | < 0.001 | 62.23 (13.8) | 61.75 (14.1) | 0.334 | 58.75 (14.8) | 59.12 (14.0) | 0.002 |
| Female, (%) | 68.8 | 69.6 | 0.023 | 47.6 | 52.4 | < 0.001 | 55.6 | 55.6 | 0.74 | 45.2 | 48.1 | < 0.001 |
| ASA Class, (%) | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||
| 1,2 | 14.9 | 17.9 | 39.7 | 43.3 | 25.8 | 29.1 | 42.2 | 50.8 | ||||
| 3 | 55.8 | 64.5 | 49.8 | 51.5 | 59.0 | 66.3 | 51.8 | 46.7 | ||||
| 4,5 | 29.3 | 17.6 | 10.5 | 5.2 | 15.2 | 4.6 | 6.4 | 2.5 | ||||
| Functional status, (%) | < 0.001 | < 0.001 | 0.712 | < 0.001 | ||||||||
| Independent | 73.7 | 79.5 | 98.3 | 97.3 | 99.3 | 99.1 | 97.3 | 97.9 | ||||
| Partially dependent | 21.1 | 17.5 | 1.6 | 2.2 | 0.7 | 0.8 | 2.5 | 1.9 | ||||
| Totally dependent | 5.3 | 3.0 | 0.2 | 0.5 | 0.0 | 0.1 | 0.2 | 0.2 | < 0.001 | |||
| Tobacco use, (%) | 11.6 | 12.2 | 0.016 | 15.9 | 16.8 | < 0.001 | 15.4 | 16.9 | 0.252 | 21.9 | 20.7 | < 0.001 |
| Congestive heart failure, (%) | 3.6 | 3.7 | 0.373 | 0.8 | 1.1 | < 0.001 | 0.2 | 0.1 | 0.269 | 0.1 | 0.4 | < 0.001 |
| COPD, (%) | 10.2 | 11.1 | < 0.001 | 4.6 | 4.5 | 0.545 | 4.0 | 4.4 | 0.628 | 3.3 | 4.5 | < 0.001 |
| Hypertension, (%) | 60.5 | 67.7 | < 0.001 | 44.1 | 48.7 | < 0.001 | 42.6 | 52.1 | < 0.001 | 39.3 | 52.9 | < 0.001 |
| Diabetes, (%) | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||
| None | 83.8 | 81.2 | 83.9 | 84.1 | 79.2 | 74.5 | 86.3 | 81.3 | ||||
| Oral medication | 10.7 | 10.5 | 12.1 | 10.6 | 15.0 | 14.1 | 10.1 | 12.3 | ||||
| Insulin | 5.5 | 8.3 | 4.0 | 5.3 | 5.8 | 11.4 | 3.7 | 6.4 | ||||
| Inpatient (%) | 99.4 | 99.7 | < 0.001 | 99.2 | 99.0 | 0.018 | 99.8 | 99.6 | 0.358 | 84.2 | 65.5 | < 0.001 |
In unadjusted analyses mortality was generally similar for patients in Canada and the USA (Fig. 1 and Appendix Table 2). Alternatively, patients in Canada had significantly higher rates of cardiac events, pneumonia, and surgical site infections for virtually all procedures resulting a significantly increased rate of the composite outcome for patients in Canada than in the USA for all four procedures (Fig. 2 and Appendix Table 2). For example, after colectomy 1.62% of patients in Canada and 0.96% of patients in the USA experienced a cardiac complication (P <0.001), while after pancreatectomy 16.1% of patients in Canada and 12.7% in the USA experienced a surgical site infection (P <0.001). Mean hospital length of stay was significantly longer for patients in Canada for all four procedures, while the rate of hospital readmission was significantly lower.
Fig. 1.
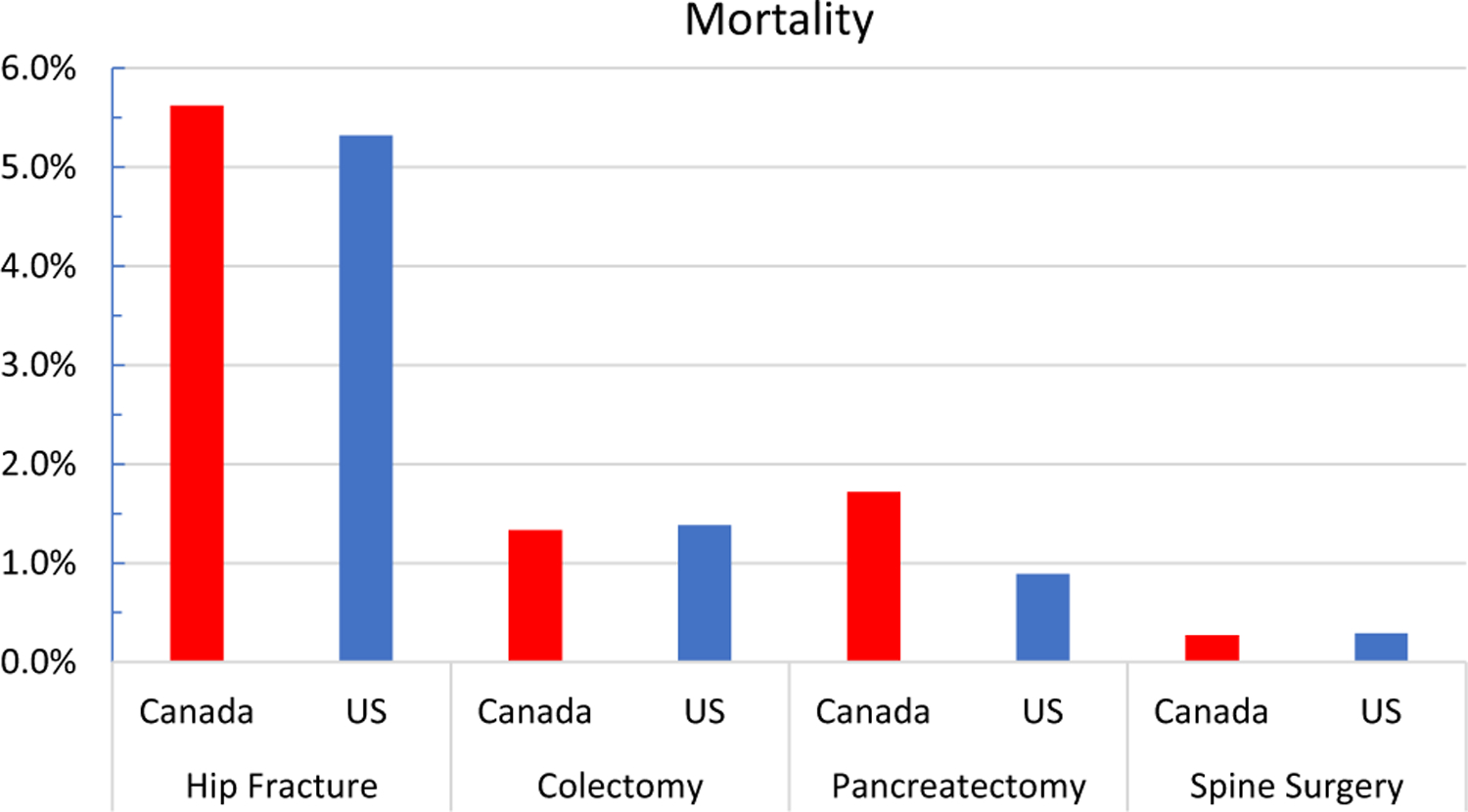
Unadjusted mortality within 30-days of surgery
Fig. 2.
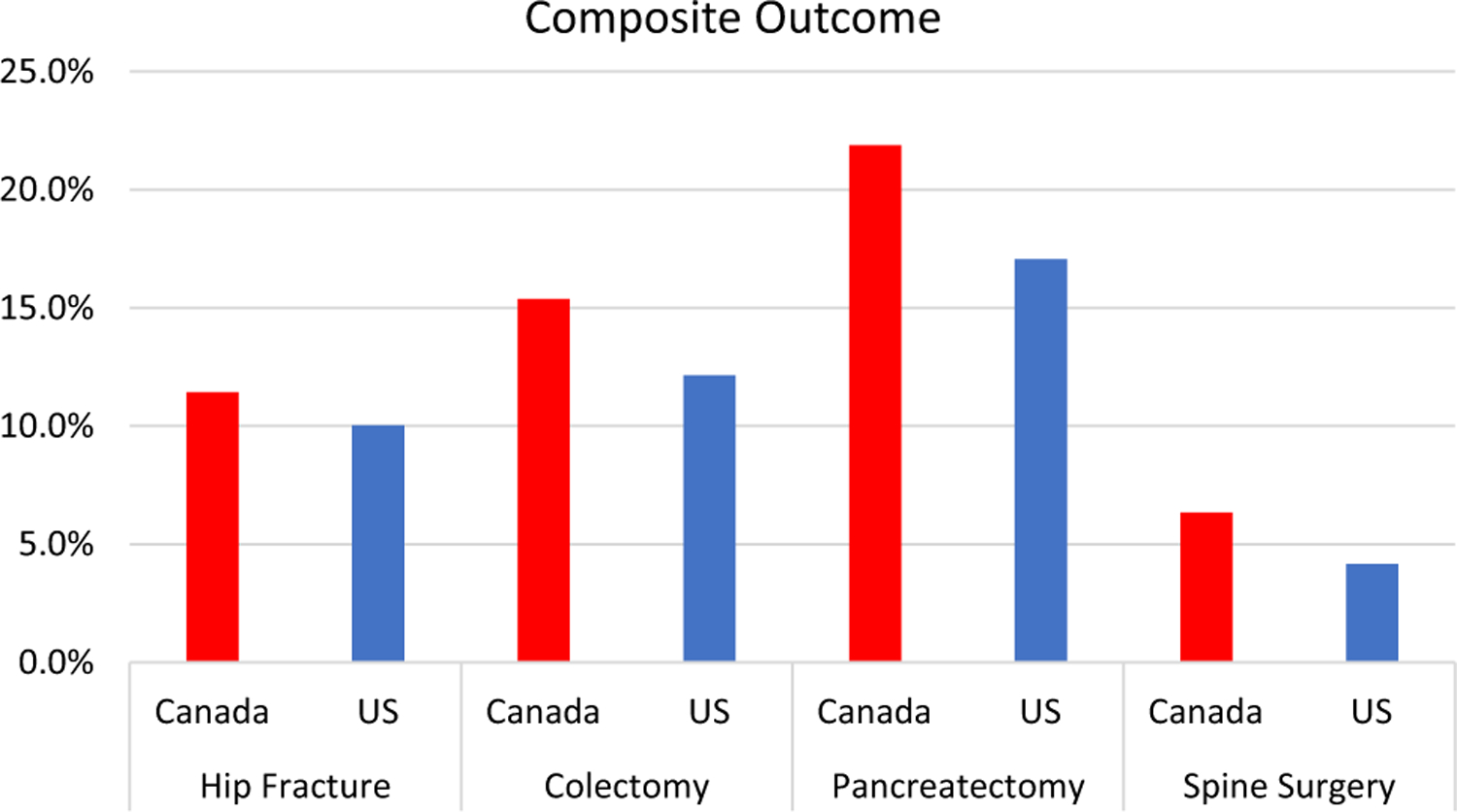
Unadjusted composite outcome within 30-days of surgery
In adjusted analyses focusing on death within 30-days of surgery that included ASA class, mortality was significantly higher in Canada for one procedure (pancreatectomy) and similar for the other three (Fig. 3 and Appendix Table 3); in analyses that excluded ASA class, mortality was significantly higher in Canada for two procedures (colectomy and pancreatectomy) and similar for the remaining two (Fig. 3). In adjusted analyses focusing on the composite outcome, odds of the composite outcome were significantly higher in Canada for three procedures (colectomy, pancreatectomy, and spine surgery) in models that included and excluded ASA class (Fig. 4 and Appendix Table 3). Odds of a prolonged hospital LOS were significantly higher, but odds of hospital readmission significantly lower in Canada for all four procedures as compared to the USA. Results were similar to our main findings when outpatient spine surgery cases were excluded.
Fig. 3.
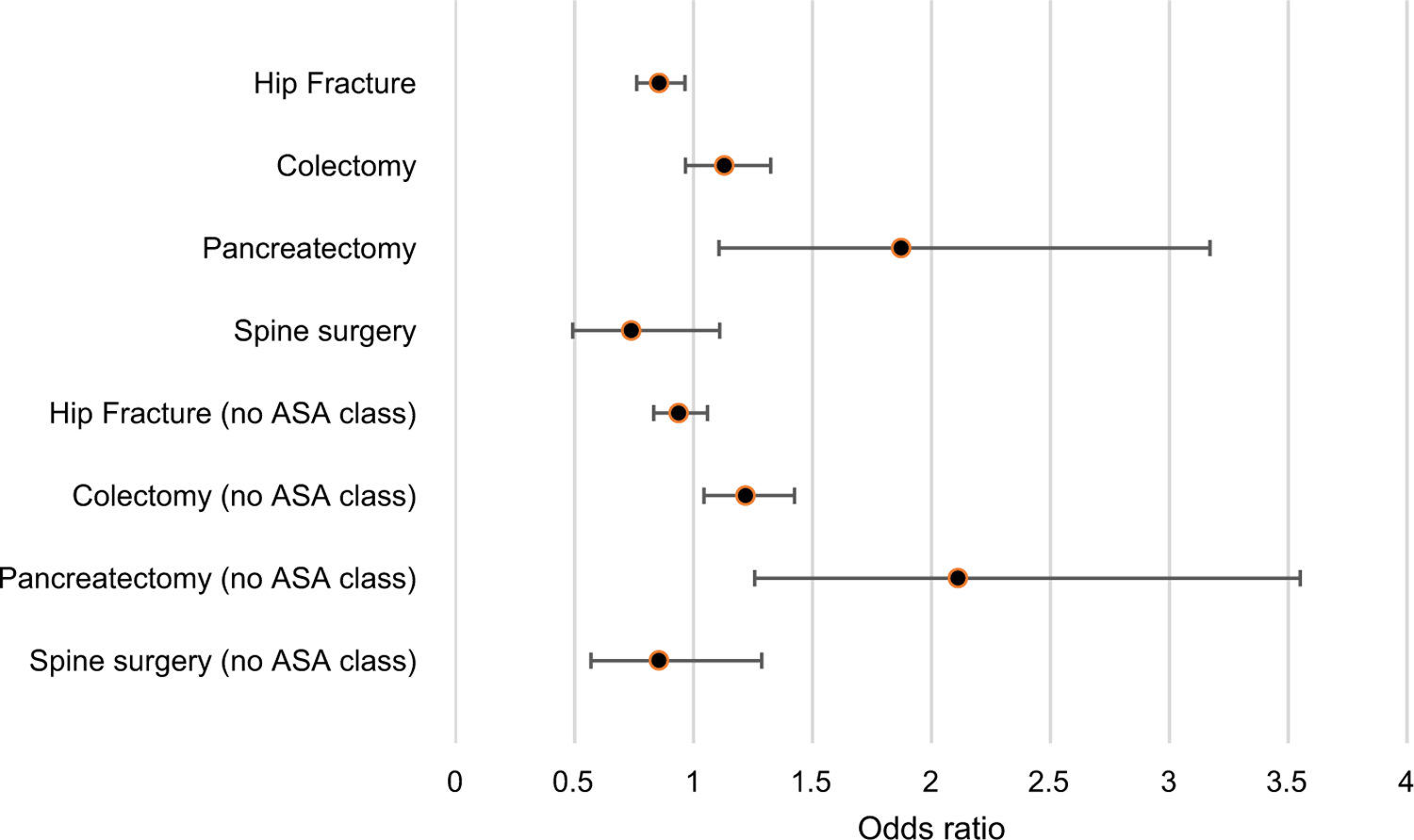
Adjusted odds of mortality within 30-days of surgery in Canada (USA as reference) in models with and without adjustment for ASA class
Fig. 4.
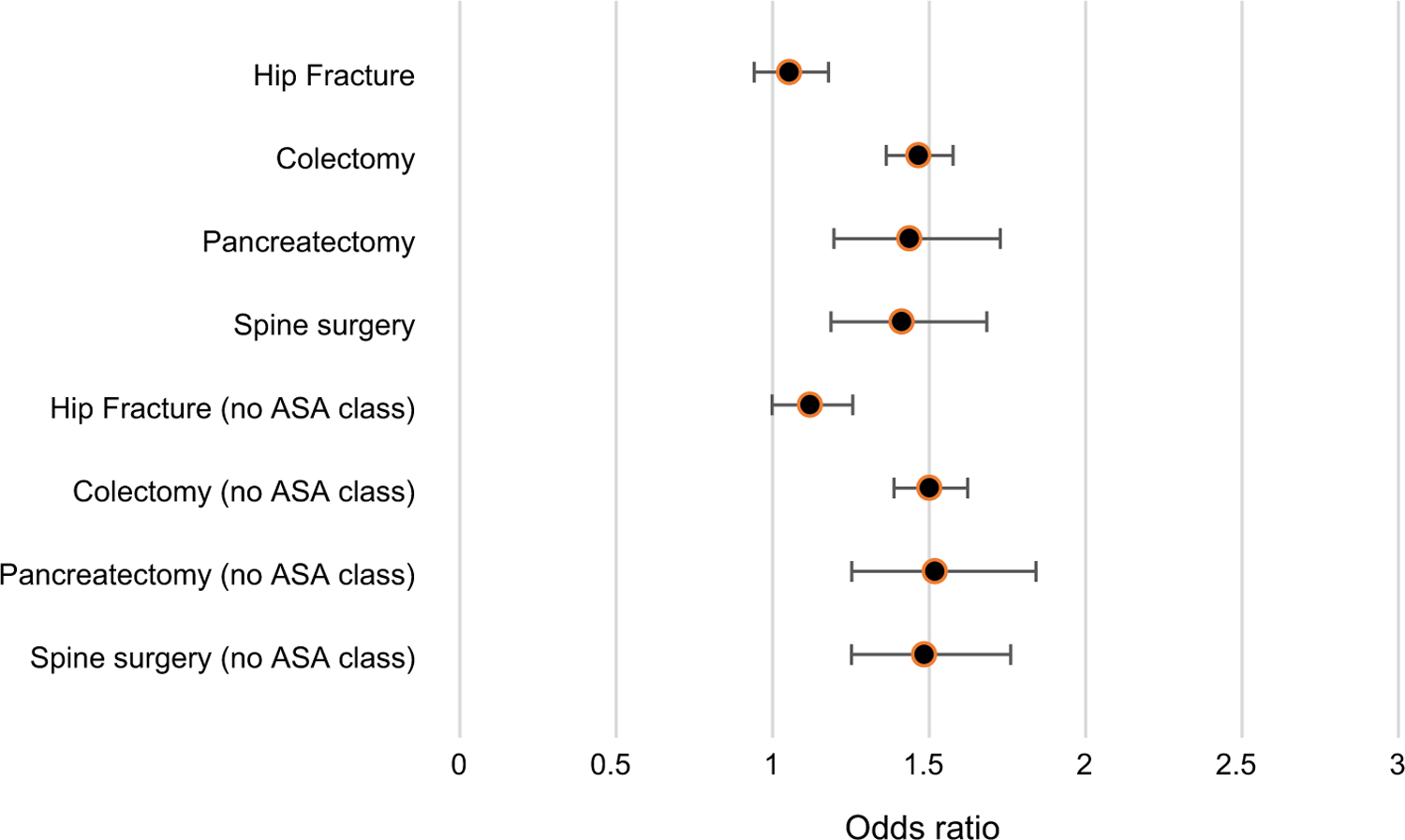
Adjusted odds of composite outcome (one-or-more of cardiac arrest, myocardial infarction, pneumonia, acute renal failure, return to operating room, surgical site infection, sepsis, unplanned intubation, wound disruption) within 30-days of surgery in Canada (USA as reference) in models with and without adjustment for ASA class
Discussion
In an analysis of data from a large international surgical registry we found evidence of worse outcomes in Canada than in the USA for four common surgical procedures. We found higher mortality in Canada for two procedures (colectomy and pancreatectomy) and higher complication rates in Canada for all four procedures. In total these results provide important new insights into differences in surgical outcomes for two geopolitically similar countries with different healthcare delivery systems.
Our finding of higher mortality for patients in Canada builds on several older studies comparing outcomes in Canada and the USA. Nearly 30-years ago seminal work by Roos et al. found higher surgical mortality in Canada relative to the USA for hip fracture and coronary artery graft bypass surgery. [20] In the intervening years several additional studies have used administrative data to compare Canada and the USA with respect to cardiovascular outcomes, [21, 22] with most finding similar mortality.
Far fewer studies have compared mortality for discrete surgical procedures; several, using administrative data, have demonstrated increased mortality for patients in Canada for procedures including spine surgery and joint arthroplasty. [5, 23] A crucial limitation has been a reliance upon administrative data [5, 20, 24, 25] resulting in limited ability to adjust for patient complexity and to ascertain more granular post-surgical outcomes. In the only registry-based Canada-US comparison of surgical outcomes that we are aware of, Hart et al. used data from ACS-NSQIP to compare surgical outcomes for total joint arthroplasty and found similar rates of mortality in the two countries, but higher rates of major complications in Canada for knee (but not hip) arthroplasty. [9]
Our finding of significantly higher mortality in Canada for two procedures (colectomy and pancreatectomy) and higher post-operative complication rates for all 4 procedures is noteworthy.
While administrative data are commonly used to identify post-operative complications including surgical site infections, venous thromboembolism, and myocardial infarction within a single country, [26] valid international comparisons are far more complicated and using administrative data has important limitations. For example, international comparisons require that case ascertainment (e.g., identification of colectomy or pancreatectomy), identification of outcomes (mortality or post-operative surgical site infections) and comorbidity coding algorithms (e.g., Elix-hauser, ADGs) be applied similarly in countries with different underlying coding schemes. [27] Moreover such comparisons are predicated on the assumption and that coding practices (e.g., capture of comorbid conditions) are similar in different countries. [1, 2] A recently published working paper from the Organization for Economic Cooperation and Development (OECD) provides a meticulous overview of the methodological challenges involved in analysis of multi-system administrative data. [2] The investigators reported on the significant issues that their research group encountered in trying to develop a standard method for allowing comparison of myocardial infarction rates across countries; these challenges would also apply to international comparison of surgical procedures. Administrative claims data can be problematic for between-country comparison for a variety of reasons. For example, the USA only switched from International Classification of Diseases) ICD-9 to ICD-10 codes in 2015, while Canada has been using ICD-10 since 2001. Moreover, while the US uses ICD-10 codes to capture both diagnoses and procedures, Canada uses Canadian Classification of Interventions (CCI) codes which are similar, but not completely analogous.
International registries such as ACS-NSQIP can circumvent many of the aforementioned limitations by using medical record review and meticulously developed definitions for key variables; administrative data enhanced by additional clinical variables could be another way to strength international comparisons. For example, studies using administrative data to compare outcomes in the USA and Canada commonly find that the prevalence of comorbid conditions such as diabetes or congestive heart failure appear to be 200%−300% higher in the USA than in Canada; these differences are seen in administrative (aka, billing) data because US hospitals have strong financial incentives to document comorbidities supported by well-developed infrastructure (billing offices, coders, electronic health records) that Canada lacks. [23, 28] These erroneous differences in comorbidity are largely absent in our current study using NSQIP data where data are collected in a standardized manner in both countries.
The notable exception to the comparability of NSQIP data from the USA and Canada appears to be ASA class and this warrants elaboration. Our authorship team includes practicing surgeons from both the USA and Canada and all suspect that the differences in ASA class reported in NSQIP reflect the effects of differential coding rather than true differences in patient severity. ASA class is commonly used in surgical and anesthesia risk adjustment and has been consistently used in ACS-NSQIP risk models because of its strong and consistent association with adverse outcomes. [8] ASA classes are clearly defined in clinical practice, making the differences we found in our analysis surprising. [29] We suspect that differences between the Canadian and US anesthesiology reimbursement systems might incentivize increased coding of complexity to a greater extent in Canada than in the USA. [30–32] Alternatively, it is possible that the higher ASA class seen in US patients relative to Canadian patients represents true differences in complexity; NSQIP should consider embarking on a targeted audit of this variable. Differences in reimbursement also apply to surgical complications. Hospitals in the USA have been shown to receive higher reimbursement for patients who experience complications than for patients who do not, [33, 34] whereas this is not the case in Canada; if anything such financial incentives would serve to increase the coding of complications in the USA and thus would artificially reduce the magnitude of the Canadian outcome deficit.
The findings of inferior outcomes in Canada beget questions of potential causes. The USA and Canada have many similarities in terms of culture, values, and politics, but also significant differences with respect to healthcare financing and delivery that nearly certainly contribute. Government in Canada is both the sole payer for healthcare services and operator of hospitals, and healthcare is largely administered at the provincial level. [35] Hospitals in Canada are typically globally budgeted, while most physicians are reimbursed on a fee-for-service basis resulting in a tension between hospitals that must live within a strict budget and physicians who have incentives to increase procedure volumes. Provinces deliberately regionalize many medical and surgical procedures. [36, 37] Alternatively, the USA has a mixture of public and private payers and organized regionalization of services is haphazard. While US physicians are generally reimbursed on a fee-for-service basis like their Canadian counterparts, US hospitals are also reimbursed on a fee-for-service (DRG) basis; thus, US hospitals are paid more for increasing volume, while Canadian hospitals are not. While regionalization has benefits of centralizing procedural expertise within circumscribed centers of excellence, regionalization is also known to result in prolonged travel distances. [37] Canadian health care has been plagued by chronic problems with access to and wait times for health services including surgical procedures. [24, 38] Both increased travel time [39] and prolonged wait times could adversely affect surgical outcomes. Differences in physician and nursing workload are also plausible causes. [40] There are few direct comparisons of nurse staffing ratios between countries, but some data do suggest greater nursing workload in Canada. [40] With respect to physician workload, the USA has imposed strict caps on the number of patients that resident physicians may look after, while Canada does not adhere to strict caps or work hour limits. [41, 42] It is also important to consider that the USA has invested heavily in important “enablers” of quality including health information technology and patient safety initiatives in ways that Canada has not. [43] For example, NSQIP was widely adopted across the USA in the late 1990s, but has only gained traction in Canada over the last 5-years. [44] Likewise, most large US hospitals fund the time of physicians and nurses to monitor and improve patient safety while funding for such positions is less common in Canadian hospitals [45]. While further research is always helpful, we would argue that Canadian government, hospitals, and physicians should consider taking action without delay.
Several other findings warrant brief attention. The finding of longer hospital LOS and lower hospital readmission rates in Canada relative to the US, reflects the incentives under which hospitals in each of the systems operate [4, 46]. Canadian hospitals are globally budgeted and receive no incremental funding for admissions (or readmissions). In contrast, US hospitals have historically received payment for each admission resulting in a strong incentive to discharge as quickly as possible, [47] at the expense of exceedingly high readmission rates.3Our finding of longer LOS but lower readmission rates in Canada in both unadjusted and adjusted results extends prior findings to the surgical population.
This study has several limitations that warrant mention. First, ACS-NSQIP data are contributed by voluntary participant hospitals which might represent institutions with an inherent interest in quality and must therefore be generalized with care. Second, the NSQIP sampling strategy does not allow us to calculate hospital or surgeon procedure volume or incidence or prevalence rates. Third, as is evident with the coding of ASA class, despite clear methods for recording data, there may be systematic differences in how particular data points are ascertained and recorded across the two countries. Research is needed within NSQIP to better understand the differences in ASA coding in the USA and Canada. Fourth, NSQIP does not contain information on the indication for surgery. While we applied identical inclusion and exclusion criteria for both the USA and Canada it is possible that there are differences in the surgical cohorts. We used NSQIP’s well studied risk-adjustment models but cannot exclude the possibility of unmeasured confounding.
In conclusion, we found evidence of better surgical outcomes in the USA as compared to Canada for four surgical procedures. While further research is certainly warranted, the potential seriousness of our findings should serve as an impetus for action by Canadian government, hospitals, and physicians.
Appendix 1
See Table 2
Table 2.
List of codes used for identification of hip fractures, colectomy, pancreatectomy, and spine surgery
| Procedure | Current procedural terminology (CPT) codes |
|---|---|
| Hip fracture | 27,130, 27,125, 27,236, 27,244, or 27,245 with ICD-9 code 820.21 or ICD10 S72.0, S72.1 or S72.2 |
| Colectomy | 44,140, 44,141, 44,143, 44,144, 44,145, 44,146, 44,147, 44,150, 44,151, 44,160, 44,204, 44,205, 44,206, 44,207, 44,208, and 44,210 |
| Pancreatectomy | 48,140, 48,145, and 48,146 |
| Spine surgery | 22,548, 22,551, 22,554, 22,856, 22,861, 63,075, 63,081, 63,300, 63,304 22,556, 22,558, 22,857, 22,862, 63,077, 63,085, 63,087, 63,090, 63,101, 63,102, 63,301, 63,302, 63,303, 63,305, 63,306, 63,307, 22,552, 63,076, 63,078, 63,082, 63,086, 63,088, 63,091, 63,103, 63,308, 22,845, 22,846, 22,847, 22,210, 22,216, 22,220, 22,226, 22,326, 22,590, 22,595, 22,600, 63,001,63,015, 63,020, 63,040, 63,045, 63,050, 63,051, 22,206, 22,207, 22,208, 22,212, 22,214, 22,216, 22,222, 22,224, 22,226,22,325, 22,327, 22,610, 22,612, 22,630, 22,633, 22,800, 22,802, 22,804,63,003, 63,005, 63,011, 63,012, 63,016, 63,017, 63,030, 63,042, 63,046, 63,047, 63,055, 63,056, 63,064, 22,614, 22,632, 22,634, 63,035, 63,043, 63,044, 63,048, 63,057, 63,066, 22,840, 22,841, 22,842, 22,843, 22,844, 22,848, 22,849, 22,840, 22,841, 22,842, 22,843, 22,844, 22,845, 22,846, 22,847,22,848,22,849, 22,851, 22,554, 22,556, 22,558, 22,585, 22,590, 22,595, 22,600, 22,610, 22,612, 22,614, 22,630, 22,632, 22,633, 22,634, 22,800, 22,802, 22,804, 22,552, 22,585, 22,614, 22,632, 22,634, 63,015, 63,016, 63,017, 63,035, > 1 level of surgery 63,043, 63,044, 63,048, 63,057, 63,066, 63,076, 63,078, 63,082, 63,086, 63,088, 63,091, 63,103, 63,308 |
Appendix 2
See Table 3
Table 3.
Unadjusted outcomes for hip fracture, colectomy, pancreatectomy, and spine surgery performed in Canada and the USA
| Hip fracture | Colectomy | Pancreatectomy | Spine surgery | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Canada (N = 21,166) | US (N = 73,817) | P-value | Canada (N = 21,276) | US (N = 218,307) | P-value | Canada (N = 873) | US (N = 12,078) | P-value | Canada (N = 14,088) | US (N = 252,029) | P-value | |
| Mortality, number (%) | 1190 (5.62) | 3962 (5.32) | 0.085 | 282 (1.33) | 3005, 1.38 | 0.541 | 15 (1.72) | 108 (0.89) | 0.015 | 38 (0.27) | 741 (0.29) | 0.604 |
| Cardiac, number (%) | 723 (3.42) | 1728 (2.34) | < 0.001 | 345 (1.62) | 2088 (0.96) | < 0.001 | 30 (3.44) | 162 (1.34) | < 0.001 | 60 (0.43) | 992 (0.39) | 0.552 |
| Pneumonia, number (%) | 751 (3.58) | 2179 (2.98) | < 0.001 | 483 (2.27) | 3733 (1.71) | < 0.001 | 55 (6.32) | 326 (2.70) | < 0.001 | 104 (0.74) | 1745 (0.69) | 0.524 |
| Renal Failure, number (%) | 123 (0.58) | 462 (0.63) | 0.462 | 227 (1.07) | 2492 (1.14) | 0.325 | 11 (1.26) | 88 (0.73) | 0.082 | 17 (0.12) | 474 (0.19) | 0.070 |
| ROR, number (%) | 302 (1.43) | 1310 (1.77) | < 0.001 | 890 (4.18) | 9066 (4.15) | 0.833 | 33 (3.78) | 346 (2.86) | 0.121 | 438 (3.11) | 6023 (2.39) | < 0.001 |
| SSI, number (%) | 320 (1.51) | 735 (1.00) | < 0.001 | 2169 (10.28) | 14,676 (6.82) | < 0.001 | 140 (16.13) | 1526 (12.72) | 0.004 | 434 (3.09) | 3737 (1.48) | < 0.001 |
| Sepsis, number (%) | 191 (0.91) | 860 (1.17) | 0.001 | 659 (3.12) | 6516 (3.07) | 0.677 | 30 (3.46) | 599 (4.99) | 0.043 | 66 (0.47) | 1489 (0.59) | 0.063 |
| Unplanned Intubation, number (%) | 101 (0.48) | 994 (1.35) | < 0.001 | 222 (1.04) | 2844 (1.30) | 0.001 | 13 (1.49) | 212 (1.76) | 0.561 | 50 (0.35) | 1053 (0.42) | 0.258 |
| Composite | 2419 (11.43) | 7408 (10.04) | < 0.001 | 3272 (15.38) | 26,514 (12.15) | < 0.001 | 191 (21.88) | 2060 (17.06) | < 0.001 | 893 (6.34) | 10,520 (4.17) | < 0.001 |
| LOS event (> 6 days), number (%) | 10,375 (49.02) | 10,748 (14.56) | < 0.001 | 5034 (23.66) | 40,628 (18.61) | < 0.001 | 282 (32.30) | 2689 (22.26) | < 0.001 | 4736 (33.62) | 51,554 (20.46) | < 0.001 |
| LOS, days, mean, SD) | 9.13 (9.33) | 4.42 (4.19) | < 0.001 | 6.60 (6.61) | 5.62 (5.48) | < 0.001 | 7.57 (5.92) | 6.58 (4.85) | < 0.001 | 3.89 (7.17) | 2.44 (4.81) | < 0.001 |
| Readmission, number (%) | 918 (4.34) | 6765 (9.16) | < 0.001 | 1699 (7.99) | 21,105 (9.67) | < 0.001 | 113 (12.94) | 2007 (16.62) | 0.005 | 495 (3.51) | 11,552 (4.58) | < 0.001 |
Bold values indicate statistical significance (P < 0.05)
Denominators vary slightly by procedure and outcome reflecting NSQIP methodology and rules for the coding and assessment of each outcome
Appendix 3
See Table 4
Table 4.
Odds of adverse outcomes in Canada (USA as reference) for each surgical procedure and outcome in models including and excluding ASA class from models
| Hip fracture | Hip fracture no ASA class | Colectomy | Colectomy no ASA class | |||||
|---|---|---|---|---|---|---|---|---|
| Canada OR (95% CI) | P-value | Canada OR (95% CI) | P-value | Canada OR (95% CI) | P-value | Canada OR (95% CI) | P-value | |
| Mortality | 0.856 (0.761–0.964) | 0.010 | 0.938 (0832–1.058) | 0.298 | 1.130 (0.965–1.324) | 0.128 | 1.219 (1.044–1.424) | 0.012 |
| Cardiac event | 1.417 (1.040–1.931) | 0.027 | 1.508 (1.089–2.089) | 0.014 | 1.651 (1.234–2.209) | < 0.001 | 1.740 (1.274–2.377) | < 0.001 |
| Pneumonia | 1.172 (1.023–1.343) | 0.023 | 1.225 (1.078–1.393) | 0.002 | 1.438 (1.233–1.678) | < 0.001 | 1.482 (1.284–1.711) | < 0.001 |
| Renal failure | 0.973 (0.773–1.225) | 0.818 | 0.973 (0.773–1.225) | 0.818 | 1.007 (0.868–1.170) | 0.922 | 1.025 (0.889–1.180) | 0.737 |
| Return to operating room | 0.794 (0.683–0.924) | 0.003 | 0.819 (0.705–0.951) | 0.009 | 1.077 (0.949–1.221) | 0.249 | 1.093 (0.965–1.238) | 0.163 |
| Surgical site infection | 1.568 (1.299–1.892) | < 0.001 | 1.558 (1.298–1.870) | < 0.001 | 1.730 (1.556–1.923) | < 0.001 | 1.732 (1.553–1.931) | < 0.001 |
| Sepsis | 0.775 (0.619–0.971) | 0.027 | 0.806 (0.647–1.004) | 0.055 | 1.120 (0.961–1.306) | 0.146 | 1.141 (0.988–1.318) | 0.072 |
| Unplanned intubation | 0.347 (0.268–0.448) | < 0.001 | 0.375 (0.291–0.482) | < 0.001 | 0.841 (0.689–1.026) | 0.088 | 0.881 (0.734–1.058) | 0.176 |
| Composite | 1.053 (0.941–1.178) | 0.371 | 1.120 (0.998–1.256) | 0.054 | 1.466 (1.363–1.576) | < 0.001 | 1.501 1.388–1.624) | < 0.001 |
| LOS event (> 6-days) | 6.558 (5.365–8.017) | < 0.001 | 6.702 (5.524–8.132) | < 0.001 | 1.678 (1.518–1.848) | < 0.001 | 1.718 (1.558–1.894) | < 0.001 |
| Readmission | 0.458 (0.402–0.521) | 0.467 (0.412–0.530) | < 0.001 | 0.850 (0.793–0.911) | < 0.001 | 0.864 (0.804–0.928) | < 0.001 | |
| Pancreatectomy | Pancreatectomy no ASA class | Spine surgery | Spine surgery no ASA class | |||||
| Canada OR (95% CI) | P-value | Canada OR (95% CI) | P-value | Canada OR (95% CI) | P-value | Canada OR (95% CI) | P-value | |
| Mortality | 1.873 (1.107–3.171) | 0.020 | 2.112 (1.257–3.550) | 0.005 | 0.739 (0.492–1.110) | 0.144 | 0.855 (0.569–1.286) | 0.452 |
| Cardiac event | 2.271 (1.128–4.571) | 0.022 | 2.717 (1.267–5.828) | 0.010 | 1.017 (0.758–1.363) | 0.913 | 1.124 (0.852–1.483) | 0.406 |
| Pneumonia | 2.751 (1.492–5.074) | 0.001 | 2.912 (1.536–5.523) | 0.001 | 0.963 (0.506–1.833) | 0.909 | 1.085 (0.567–2.078) | 0.804 |
| Renal failure | 2.019 (1.227–3.324) | 0.006 | 2.019 (1.227–3.324) | 0.006 | 0.676 (0.425–1.076) | 0.099 | 0.725 (0.461–1.140) | 0.163 |
| Return to operating room | 1.347 (0.924–1.964) | 0.121 | 1.444 (1.015–2.053) | 0.041 | 1.155 (0.984–1.354) | 0.077 | 1.195 (1.020–1.400) | 0.027 |
| Surgical site infection | 1.448 (1.231–1.703) | < 0.001 | 1.494 (1.267–1.762) | < 0.001 | 2.007 (1.540–2.614) | < 0.001 | 2.059 (1.578–2.687) | < 0.001 |
| Sepsis | 0.747 (0.558–1.001) | 0.051 | 0.786 (0.589–1.050) | 0.103 | 0.714 (0.462–1.105) | 0.131 | 0.771 (0.504–1.180) | 0.230 |
| Unplanned intubation | 0.952 (0.533–1.700) | 0.868 | 1.112 (0.633–1.951) | 0.711 | 0.744 (0.587–0.942) | 0.014 | 0.839 (0.658–1.071) | 0.159 |
| Composite | 1.437 (1.196–1.727) | < 0.001 | 1.519 (1.253–1.841) | < 0.001 | 1.413 (1.186–1.684) | < 0.001 | 1.485 (1.252–1.761) | < 0.001 |
| LOS event (> 6-days) | 1.924 (1.381–2.680) | < 0.001 | 2.069 (1.559–2.748) | < 0.001 | 1.757 (1.234–2.502) | 0.002 | 1.871 (1.314–2.664) | < 0.001 |
| Readmission | 0.778 (0.646–0.937) | 0.008 | 0.799 (0.661–0.965) | 0.020 | 0.691 (0.611–0.782 | < 0.001 | 0.727 (0.645–0.818) | < 0.001 |
Bold values indicate statistical significance (P < 0.05)
References
- 1.Baicker K, Chandra A (2018) Challenges in understanding differences in health care spending between the United States and other high-income countries. JAMA 319(10):986–987. 10.1001/jama.2018.1152[publishedOnlineFirst:2018/03/15] [DOI] [PubMed] [Google Scholar]
- 2.Padget M, Biondi N, Brownwood I. 2020. Methodological development of international measurement of acute myocardial infarction 30-day mortality rates at the hospital level: OECD.
- 3.Papanicolas I, Woskie LR, Jha AK (2018) Health care spending in the United States and other high-income countries. JAMA 319(10):1024–1039. 10.1001/jama.2018.1150[publishedOnlineFirst:2018/03/15] [DOI] [PubMed] [Google Scholar]
- 4.Samsky MD, Ambrosy AP, Youngson E et al. (2019) Trends in readmissions and length of stay for patients hospitalized with heart failure in Canada and the United States. JAMA Cardiol 4(5):444–453. 10.1001/jamacardio.2019.0766[publishedOnlineFirst:2019/04/11] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cram P, Landon BE, Matelski J et al. (2018) Utilization and short-term outcomes of primary total hip and knee arthroplasty in the United States and Canada: an analysis of New York and Ontario administrative data. Arthritis Rheumatol 70(4):547–554. 10.1002/art.40407[publishedOnlineFirst:2017/12/30] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung SC, Gedeborg R, Nicholas O et al. (2014) Acute myocardial infarction: a comparison of short-term survival in national outcome registries in Sweden and the UK. Lancet 383(9925):1305–1312. 10.1016/s0140-6736(13)62070-x[publishedOnlineFirst:2014/01/28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rapsomaniki E, Thuresson M, Yang E et al. (2016) Using big data from health records from four countries to evaluate chronic disease outcomes: a study in 114 364 survivors of myocardial infarction. European Heart Journal - Quality of Care and Clinical Outcomes 2(3):172–183. 10.1093/ehjqcco/qcw004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen ME, Ko CY, Bilimoria KY et al. (2013) Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg 217(2):336–346. 10.1016/j.jamcollsurg.2013.02.027[publishedOnlineFirst:2013/05/01] [DOI] [PubMed] [Google Scholar]
- 9.Hart A, Bergeron SG, Epure L et al. (2015) Comparison of US and Canadian perioperative outcomes and hospital efficiency after total hip and knee arthroplasty. JAMA Surg. 10.1001/jamasurg.2015.1239[publishedOnlineFirst:2015/08/20] [DOI] [PubMed] [Google Scholar]
- 10.American College of Surgeons. 2016. American College of Surgeons National Surgical Quality Improvement Program Users Guide.
- 11.Lawson EH, Louie R, Zingmond DS et al. (2012) A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg 256(6):973–981. 10.1097/SLA.0b013e31826b4c4f[publishedOnlineFirst:2012/10/26] [DOI] [PubMed] [Google Scholar]
- 12.Goyal A, Ngufor C, Kerezoudis P et al. (2019) Can machine learning algorithms accurately predict discharge to nonhome facility and early unplanned readmissions following spinal fusion? analysis of a national surgical registry. J Neurosurg Spine 31(4):568–578. 10.3171/2019.3.Spine181367[publishedOnlineFirst:2019/06/08] [DOI] [PubMed] [Google Scholar]
- 13.Maxwell BG, Mirza A (2019) Medical comanagement of hip fracture patients is not associated with superior perioperative outcomes: a propensity score-matched retrospective cohort analysis of the national surgical quality improvement project. J Hosp Med 14:E1–e7. 10.12788/jhm.3343[publishedOnlineFirst:2019/12/24] [DOI] [PubMed] [Google Scholar]
- 14.Basques BA, McLynn RP, Lukasiewicz AM et al. (2018) Missing data may lead to changes in hip fracture database studies: a study of the American College of Surgeons National Surgical Quality improvement program. Bone Joint J 100-B(2):226–232. 10.1302/0301-620x.100b2.Bjj-2017-0791.R1[publishedOnlineFirst:2018/02/14] [DOI] [PubMed] [Google Scholar]
- 15.Xourafas D, Ashley SW, Clancy TE (2017) Comparison of perioperative outcomes between open, laparoscopic, and robotic distal pancreatectomy: an analysis of 1815 patients from the ACS-NSQIP procedure-targeted pancreatectomy database. J Gastrointest Surg 21(9):1442–1452. 10.1007/s11605-017-3463-5[publishedOnlineFirst:2017/06/03] [DOI] [PubMed] [Google Scholar]
- 16.Daniel FE, Tamim HM, Hosni MN et al. (2019) Short-term surgical morbidity and mortality of distal pancreatectomy performed for benign versus malignant diseases: a NSQIP analysis. Surg Endosc. 10.1007/s00464-019-07163-5[publishedOnlineFirst:2019/10/11] [DOI] [PubMed] [Google Scholar]
- 17.Papageorge CM, Zhao Q, Foley EF et al. (2016) Short-term outcomes of minimally invasive versus open colectomy for colon cancer. J Surg Res 204(1):83–93. 10.1016/j.jss.2016.04.020[publishedOnlineFirst:2016/07/28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nfonsam V, Aziz H, Pandit V et al. (2016) Analyzing clinical outcomes in laparoscopic right vs. left colectomy in colon cancer patients using the NSQIP database. Cancer Treat Commun 8:1–4. 10.1016/j.ctrc.2016.03.006[publishedOnlineFirst: 2016/10/25] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen ME, Liu Y, Ko CY et al. (2017) An examination of American College of Surgeons NSQIP surgical risk calculator accuracy. J Am Coll Surg 224(5):787–95.e1. 10.1016/j.jamcollsurg.2016.12.057[publishedOnlineFirst:2017/04/09] [DOI] [PubMed] [Google Scholar]
- 20.Roos LL, Fisher ES, Brazauskas R et al. (1992) Health and surgical outcomes in Canada and the United States. Health Aff 11(2):56–72. 10.1377/hlthaff.11.2.56[publishedOnlineFirst:1992/01/01] [DOI] [PubMed] [Google Scholar]
- 21.Ko DT, Krumholz HM, Wang Y et al. (2007) Regional differences in process of care and outcomes for older acute myocardial infarction patients in the United States and Ontario Canada. Circulation 115(2):196–203. 10.1161/circulationaha.106.657601[publishedOnlineFirst:2006/12/28] [DOI] [PubMed] [Google Scholar]
- 22.Pilote L, Saynina O, Lavoie F et al. (2003) Cardiac procedure use and outcomes in elderly patients with acute myocardial infarction in the United States and Quebec, Canada, 1988 to 1994. Med Care 41(7):813–822. 10.1097/01.mlr.0000068539.51969.36[publishedOnlineFirst:2003/07/02] [DOI] [PubMed] [Google Scholar]
- 23.Cram P, Landon BE, Matelski J et al. (2019) Utilization and outcomes for spine surgery in the United States and Canada. Spine 44(19):1371–1380. 10.1097/BRS.0000000000003083[publishedOnlineFirst:2019/07/02] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ho V, Hamilton BH, Roos LL (2000) Multiple approaches to assessing the effects of delays for hip fracture patients in the United States and Canada. Health Serv Res 34(7):1499–1518 [PMC free article] [PubMed] [Google Scholar]
- 25.Cram P, Lix LM, Bohm E et al. (2019) Hip fracture care in Manitoba, Canada and New York State, United States: an analysis of administrative data. CMAJ Open 7(1):E55–E62. 10.9778/cmajo.20180126[publishedOnlineFirst:2019/02/14] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cram P, Ibrahim SA, Lu X et al. (2012) Impact of alternative coding schemes on incidence rates of key complications after total hip arthroplasty: a risk-adjusted analysis of a national data set. Geriatr Orthop Surg Rehabil 3(1):17–26. 10.1177/2151458511435723[publishedOnlineFirst:2013/04/10] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Austin PC, van Walraven C, Wodchis WP et al. (2011) Using the Johns Hopkins Aggregated Diagnosis Groups (ADGs) to predict mortality in a general adult population cohort in Ontario Canada. Med Care 49(10):932–939. 10.1097/MLR.0b013e318215d5e2[publishedOnlineFirst:2011/04/12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pang HYM, Chalmers K, Landon B et al. (2021) Utilization Rates of Pancreatectomy, Radical Prostatectomy, and Nephrectomy in New York, Ontario, and New South Wales, 2011 to 2018. JAMA Netw Open 4(4):e215477. 10.1001/jamanetworkopen.2021.5477[publishedOnlineFirst:2021/04/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doyle DJ, Goyal A, Bansal P, et al. 2020. American Society of Anesthesiologists Classification (ASA Class). StatPearls. Treasure Island (FL): StatPearls Publishing Copyright Ó 2020, StatPearls Publishing LLC [Google Scholar]
- 30.Redelmeier DA, Thiruchelvam D, Daneman N (2008) Introducing a methodology for estimating duration of surgery in health services research. J Clin Epidemiol 61(9):882–889. 10.1016/j.jclinepi.2007.10.015[publishedOnlineFirst:2008/05/13] [DOI] [PubMed] [Google Scholar]
- 31.Sun EC, Dutton RP, Jena AB (2018) Comparison of anesthesia times and billing patterns by anesthesia practitioners. JAMA Netw Open 1(7):e184288–e184388. 10.1001/jamanetworkopen.2018.4288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yasaitis LC, Guan J, Ko DT et al. (2020) Cardiac intervention rates for older patients with acute myocardial infarction in the United States and Ontario, 2003–2013: a retrospective cohort study. CMAJ Open 8(2):E437–E447. 10.9778/cmajo.20190190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu JB, Berian JR, Chen S et al. (2017) Postoperative complications and hospital payment: implications for achieving value. J Am Coll Surg 224(5):779–86.e2. 10.1016/j.jamcollsurg.2017.01.041[publishedOnlineFirst:2017/02/01] [DOI] [PubMed] [Google Scholar]
- 34.Eappen S, Lane BH, Rosenberg B et al. (2013) Relationship between occurrence of surgical complications and hospital finances. JAMA 309(15):1599–1606. 10.1001/jama.2013.2773[publishedOnlineFirst:2013/04/18] [DOI] [PubMed] [Google Scholar]
- 35.Simpson J (2012) Chronic Condition. Allan Lane, Toronto [Google Scholar]
- 36.Kreindler SA, Siragusa L, Bohm E et al. (2017) Regional consolidation of orthopedic surgery: impacts on hip fracture surgery access and outcomes. Can J Surg 60(5):349–354. 10.1503/cjs.000517[publishedOnlineFirst:2017/09/21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grumbach K, Anderson GM, Luft HS et al. (1995) Regionalization of cardiac surgery in the United States and Canada. Geographic access, choice, and outcomes. JAMA 274(16):1282–1288 [PubMed] [Google Scholar]
- 38.Wijeysundera HC, Wong WW, Bennell MC et al. (2014) Impact of wait times on the effectiveness of transcatheter aortic valve replacement in severe aortic valve disease: a discrete event simulation model. Can J Cardiol 30(10):1162–1169. 10.1016/j.cjca.2014.03.009[publishedOnlineFirst:2014/07/23] [DOI] [PubMed] [Google Scholar]
- 39.Urbach DR, Bell CM, Austin PC (2003) Differences in operative mortality between high- and low-volume hospitals in Ontario for 5 major surgical procedures: estimating the number of lives potentially saved through regionalization. CMAJ 168(11):1409–1414 [PMC free article] [PubMed] [Google Scholar]
- 40.Aiken LH, Sloane DM, Bruyneel L et al. (2014) Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 383(9931):1824–1830. 10.1016/s0140-6736(13)62631-8[publishedOnlineFirst:2014/03/04] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cram P, Chopra V, Soong C et al. (2019) Reimagining inpatient care in Canadian teaching hospitals: bold initiatives or tinkering at the margins? J Hosp Med 14(4):251–253. 10.12788/jhm.3146[publishedOnlineFirst:2019/04/02] [DOI] [PubMed] [Google Scholar]
- 42.Dunbar-Yaffe R, Wu RC, Oza A et al. (2021) Impact of an internal medicine nocturnist service on care of patients with cancer at a large Canadian teaching hospital: a quality-improvement study. CMAJ Open 9(2):E667–E672. 10.9778/cmajo.20200167[publishedOnlineFirst:2021/06/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schneider EC, Squires D (2017) From last to first - could the U.S. Health Care system become the best in the world? N Engl J Med 377(10):901–904. 10.1056/NEJMp1708704[publishedOnlineFirst:2017/07/15] [DOI] [PubMed] [Google Scholar]
- 44.Auspitz M, Cleghorn MC, Tse A et al. (2015) Understanding quality issues in your surgical department: comparing the ACS NSQIP with traditional morbidity and mortality conferences in a Canadian Academic Hospital. J Surg Educ 72(6):1272–1277. 10.1016/j.jsurg.2015.05.006[publishedOnlineFirst:2015/06/30] [DOI] [PubMed] [Google Scholar]
- 45.Byrnes J (2016) Winning at quality and safety: do you need a chief quality officer? J Healthc Manag 61(6):391–395. 10.1097/00115514-201611000-00003[publishedOnlineFirst:2016/01/01] [DOI] [PubMed] [Google Scholar]
- 46.Cram P, Girotra S, Matelski J et al. (2020) Utilization of advanced cardiovascular therapies in the United States and Canada: an observational study of New York and Ontario administrative data. Circ Cardiovasc Qual Outcomes 13(1):e006037–e6137. 10.1161/CIRCOUTCOMES.119.006037[publishedOnlineFirst:2020/01/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davis C, Rhodes DJ (1988) The impact of DRGs on the cost and quality of health care in the United States. Health Policy 9(2):117–131. 10.1016/0168-8510(88)90029-2[publishedOnlineFirst:1987/12/11] [DOI] [PubMed] [Google Scholar]


