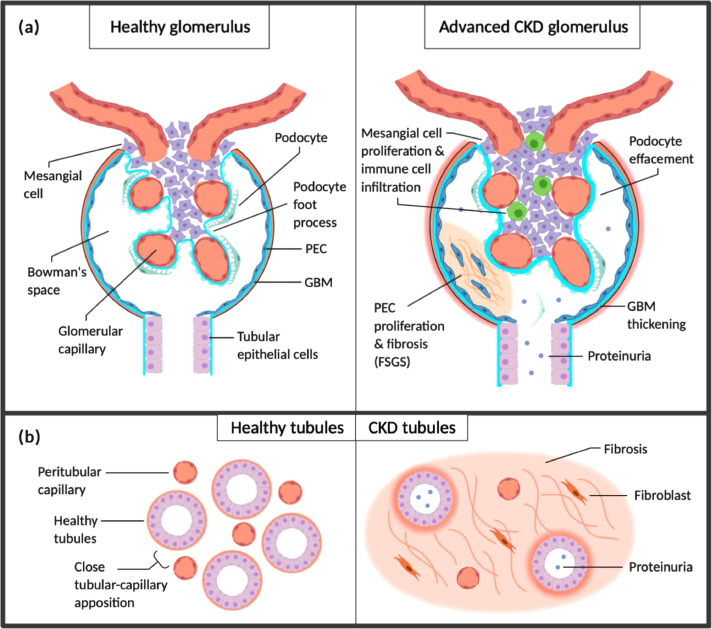
Fig. 1.
Chronic kidney disease. (a) Diseases including hypertension, DM and glomerulopathies lead to loss of functional nephrons and glomerular hypertension. Resultant RAS activation and release of pro-inflammatory, pro-fibrotic factors including TGF-α and EGFR contribute to nephron and podocyte hypertrophy. Podocytes are eventually lost due to shear stress, increasing the permeability of the glomerular basement membrane (GBM) and contributing to the development of proteinuria. Loss of podocytes also impairs capillary endothelial cell integrity due to loss of supportive factors including VEGF produced by podocytes. The pro-inflammatory environment promotes parietal epithelial cell (PEC) proliferation with fibrosis, forming ‘crescents’ crossing Bowman's space and contributing to further podocyte loss (focal segmental glomerulosclerosis; FSGS). (b) Albuminuria and infiltrating immune cells cause tubular epithelial cell stress and activation, creating a pro-inflammatory interstitial environment. This promotes interstitial fibrosis with loss of peritubular capillaries which further stresses tubular cells by reducing oxygen and nutrient transfer from capillaries, contributing to tubular atrophy. Fibrosis and atrophy accelerate the progression of CKD by further increasing demand on remaining functional nephrons.