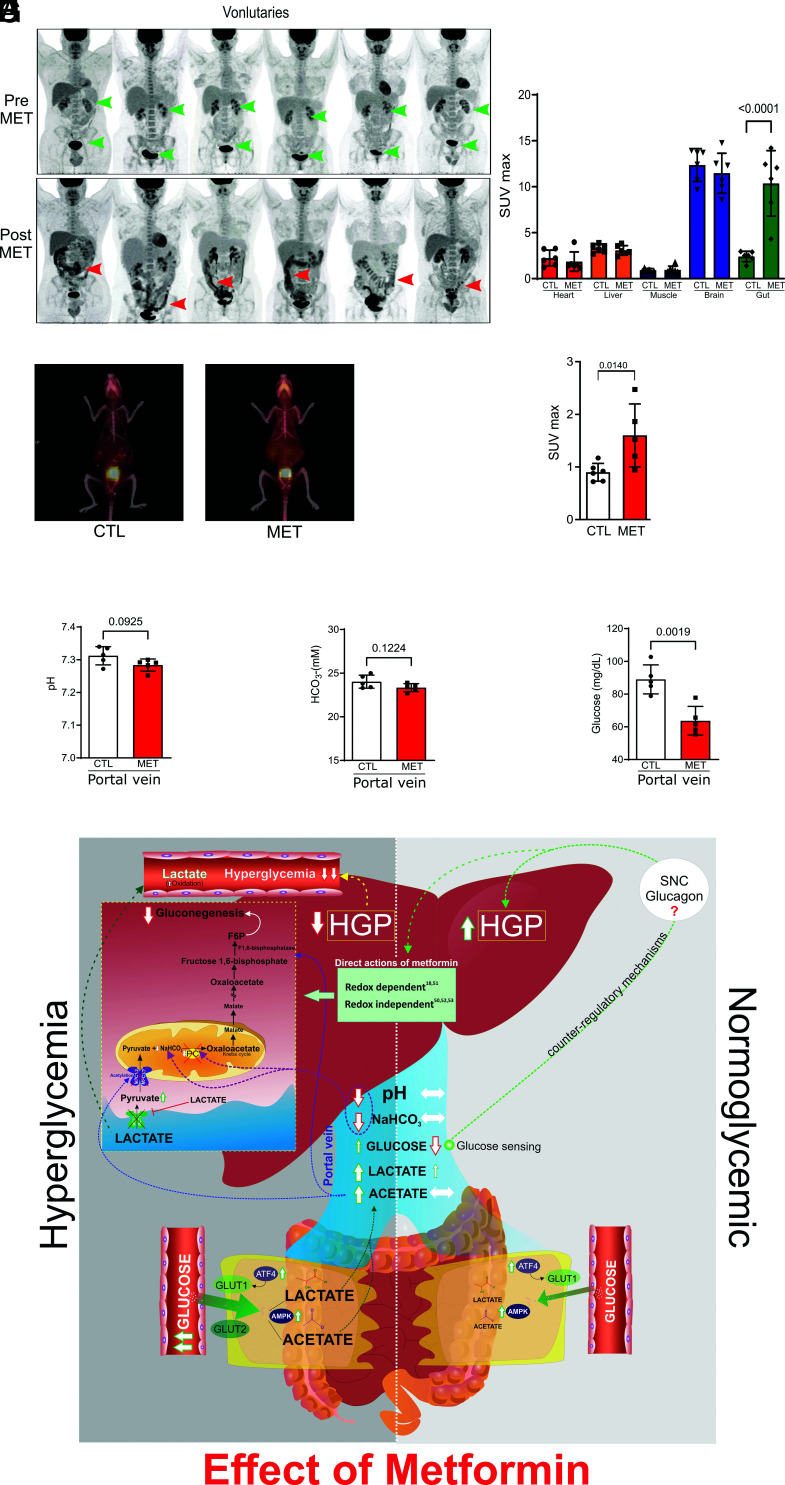
Fig. 4.
Metformin induces moderate increase BIGU in control individuals and normal glucose-tolerant rodents and does not reduce HGP in the liver of these rodents. (A) Representative images of whole-body 18F-FDG PET/CT scanning from the same healthy subjects before (PRE) and after metformin (2 g/day for 5 d) (POST). 18F-FDG PET/CT uptake is color coded, and areas of increased signal exhibit black color. (B) 18F-FDG biodistribution analysis (SUVmax) in different tissues from CTL and MET subjects (one-way ANOVA and Bonferroni’s test, P < 0.001, n = 6). (C) Representative images of whole-body 18F-FDG PET/CT scanning from mice on control chow mice treated with vehicle or metformin (MET 50 mg/kg/day for 10 d) and for 2 h before the PET/CT, 18F-FDG PET/CT uptake is color coded, and areas of increased signal exhibit red-orange color. 18F-FDG PET/CT images from lean mice (CTL) and treated with vehicle or metformin (MET). (D) SUVmax in the intestine of CTL and MET treated mice (50 mg/kg/day for 10 d) (one-way ANOVA and Bonferroni’s test, P < 0.05, n = 5 to 6). (E and F) pH and bicarbonate levels in blood from the portal vein of CTL and MET (250 mg/kg/10 d) treated Wistar rats. (G) Glucose levels in CTL and MET treated (250 mg/kg/day for 10 d) in lean Wistar rats (Student’s t test, P < 0.05, n = 5). (H) Schematic representation of metformin actions in conditions of hyperglycemia and normoglycemia. In hyperglycemic conditions, metformin induces GLUT1 and GLUT2 in the colon and ileum, where both these glucose transporters are expected to promote BIGU. In enterocytes, the glucose is metabolized to lactate, which will decrease pH and NaHCO3 in the portal vein and decrease gluconeogenesis via PC inhibition. In parallel, an increase in acetate production in the gut will induce acetylation and inhibit MPC1/2, leading to cytosolic accumulation of pyruvate, which in turn prevents the uptake of extracellular lactate through MCT1. Acetylation also blocks FBP1. These mechanisms demonstrate that metformin establishes a crosstalk between gut and liver to reduce gluconeogenesis in hyperglycemic conditions. In normoglycemic conditions, metformin induces GLUT1 and 2 expressions, but considering the Km of the glucose transporters, GLUT1 is expected to be preferentially used to modestly increase BIGU. In this condition, the increase in lactate will be discreet, and no alteration in acid–base equilibrium in the portal vein will be observed. The moderate increase in BIGU will induce hypoglycemia in the portal vein, which can induce portal glucose sensing and a possible counter-regulatory response that will avoid a decrease in HGP or even increase it. It is important to mention that other actions of metformin directly in the liver can synergize with the demonstrated gut-liver crosstalk to reduce HGP. However, in conditions of normoglycemia, the counter-regulatory mechanisms may overcome these direct actions.