Abstract
The COVID-19 pandemic has amplified the awareness and demand of public health worldwide. Based on the panel data of 81 developing countries from 2002 to 2019, this study probes into the effect of digitalization on public health and explores the mechanism through which digitalization affects public health from the perspective of income inequality. The results show that digitalization significantly enhances public health in developing countries, and this conclusion still holds after the robustness test. The heterogeneity analysis based on geographic location and income level indicates that the enhancing effect of digitalization on public health is most evident in Africa and middle-income countries. A further mechanism analysis suggests that digitalization can positively impact public health through the intermediary channel of suppressing income inequality. This study enriches the research on digitalization and public health and provides insights for comprehending public health needs and the powerful empowering effects of digitalization.
Keywords: Digitalization, Public health, Income inequality, Developing countries
1. Introduction
After the outbreak of COVID-19, Google Trends statistics showed that the retrieval quantity of “masks” and “hand washing” reached record levels in January 2020 [1]. Public health is once again in the spotlight. Public health is a crucial determinant of economic growth and is considered to be one of the most essential and fundamental human rights [2]. The United Nations Development Program (UNDP) formally adopted Transforming Our World: The 2030 Agenda for Sustainable Development in 2015 and declared sustainable development goals (SDGs) to guarantee and encourage healthy lives and well-being for all (Goal 3 of SDGs) [3]. Under the concerted effort of the global community, the global under-5 mortality rate fell by 14% based on data from 2015 to2020.1 Although, from a global perspective, actions to improve public health have yielded favorable outcomes, the situation is not as good for developing counties. In line with the World Bank statistics, despite the average under-5 mortality rate in developing countries decreasing from 3.91% to 3.33% from 2015 to 2020, the average under-5 mortality rate in developed countries also decreased from 0.64% to 0.59%. Under-5 mortality rates in developing countries are consistently at least 2.5% points higher than in developed countries. A noticeable gap exists between developed and developing countries in achieving Goal 3 of the SDGs. It is, therefore, urgent for us to explore how to raise public health levels in developing countries to achieve Goal 3 of the SDGs inclusively.
According to existing research, the factors influencing public health are mainly examined from three aspects: individual, family, and society. The individual level chiefly covers socioeconomic status [4], religious beliefs [5], and psychological characteristics [6]. The family level involves factors such as parental health literacy [7] and family social capital [8]. The social level comprises external factors such as trade openness [9], environmental pollution [10], and income disparity [11]. With the rapid development of digital technologies such as artificial intelligence, big data, cloud computing, and the internet, digitalization has inexorably integrated into all aspects of social life, profoundly changing the public's way of life [12]. It has become an essential factor affecting public health. It is worth noting that digitalization reflects both digital inputs in the production process and the broad societal changes, such as new consumption patterns, investment possibilities, and financial instruments, caused by the application of digital technologies and tools [13]. Therefore, the effect of digitalization on public health is not only health-specific, but also realized by the broader changes in society, including the widespread availability of smartphones and the increased awareness and tracking of health and lifestyle data, as well as the storage and processing of large amounts of heterogeneous data that may not be directly related to health but are relevant in understanding health and health outcomes in populations [14].
In addition to digitalization, the impact of income equality on public health cannot be ignored. Numerous studies show that income inequality hurts public health undoubtedly [15,16]. Explicitly speaking, income inequality exacerbates the sense of dispossession of residents at the bottom of the social ladder, resulting in severe psychological stress and negative emotions [17]. Income inequality can also induce profound social polarization and fail the social mechanisms of mutual trust and benefit, which in turn affects public health [18,19]. The World Inequality Report 2022 shows that current income and wealth inequalities are significantly large. The richest 10% of the global population currently takes 52% of global income, whereas the poorest half of the population earns 8.5% of it.2 Income inequality in some developing countries is more serious than that in developed countries. According to the World Inequality Database data, in Latin America and Sub-Saharan Africa, the top 10% capture 58.6% and 55.4% of national income, respectively, compared to 36% in Europe and 45.7% in North America in 2021. Therefore, confronted with the rigorous situation of income inequality, it is necessary for us not only to recognize the relationship between digitalization and public health but also to investigate how to make full use of digitalization to promote fair income distribution and narrow the income gap to achieve a “win-win” situation in terms of equity and public health enhancement in developing countries.
In light of the above discussion, this study aims to clarify the relationship between digitalization and public health by considering the mediating effect of income inequality. Compared to previous studies, the marginal contributions of this research are as follows: First, the study focuses on developing countries and comprehensively analyzes the impact of digitalization on public health from a macro perspective. Second, we theorize the impact mechanism of digitalization on public health and validate it by adopting a mediating effects model. Third, the findings may provide guidance for the formulation of policies on promoting and applying digitalization to enhance public health in a wide range of developing countries.
The remainder of the paper is organized as follows: Section 2 summarizes the existing literature. Section 3 analyzes the theoretical mechanism and hypothesis. Section 4 introduces the data and methods. Section 5 presents the empirical analysis. Section 6 discusses the conclusions and policy implications.
2. Literature review
2.1. Digitalization and public health
As the wave of digitalization advances, the health effects of digitalization are gradually being explored in depth. However, the relationship between digitalization and public health has not yet been confirmed [20]. As pre some scholars, the penetration of digitalization, as a new form of technology, into modern healthcare, education, and technology has indeed improved and enhanced public health [21,22]. Cotten (2014) found a positive contribution of digitalization to the mental well-being of retired older adults in the United States by analyzing data from four waves (2002–2008) of the Health and Retirement Survey [23]. Ma et al. (2021) supported this result with the survey data collected from 304 elderly participants in China [24]. Odone et al. (2019) suggested that digitalization should be a means, a set of tools for public health. Furthermore, digitalization can support and enable public health implementation [25]. Zhang et al. (2022) assessed the impact of digitalization on public health outcomes using China's provincial panel data from 2001 to 2016 and the China Family Panel Studies. Empirical results proved that digitalization significantly reduces population mortality in China [26]. Another portion of scholars argue that with the deep digital adoption, problematic internet use is gradually emerging and bringing about health problems, which hurts public health outcomes [27]. Sami et al. (2018) deemed that problematic internet use can cause sleep deprivation and a decline in sleep satisfaction, which can result in depression [28]. Meanwhile, Bozkurt et al. (2018) pointed out that problematic internet use crowds out physical activity and induces sedentary behavior, while reducing physical activity and sedentary behavior can lead to obesity [29]. Additionally, some scholars consider that whether digitalization enhances public health outcomes depends on the strong willingness of health demanders to search for health information [30] and the ability of health providers to access materials, skills, use and incentivize [31].
2.2. Income inequality and public health
The Income Inequality Hypothesis argues that income distribution rather than absolute income determines health outcomes. Moreover, income inequality can hurt public health [32]. This previously well accepted relationship between income inequality and health has recently come under scrutiny. On the micro level, Wilkinson (1996) stated that income inequality increases stress, which leads to negative emotions such as frustration and anger, and causes unhealthy behaviors such as smoking and alcohol consumption, thus infringing on health [32]. Using longitudinal data from the European Community Household Panel (ECHP) survey, Hildebrand and Van Kerm (2009) examined the effect of income inequality on individual self-reported health status. They found consistent evidence that income inequality was negatively related to health status in the European Union for both men and women [15]. On the macro level, Chang and Gao (2021) estimated the impact of income inequality on health outcomes in emerging Asian economies for a time horizon ranging from 1991 to 2019. The empirical results showed that income inequality negatively affects life expectancy in the long run [33]. Curran and Mahutga (2018) estimated fixed-effects models with different measures of income inequality and public health. Their results suggest that income inequality is a proximate or conditional cause of lower public health. Income inequality has a 139.7%–374.3% more harmful effect on health in poorer than richer countries [16].
2.3. Digitalization and income inequality
The inclusiveness, integration, and sharing of digitalization have become critical tools for addressing unbalanced and inadequate development [34]. However, the existing studies on digitalization and income inequality have yet to reach uniform conclusions due to the different econometric methods and samples used. Several studies have found that digitalization has income-generating and poverty-reducing effects that can reduce income inequality and contribute to shared prosperity and inclusive growth [35,36]. Mora-Rivera et al. (2021) argued that the spread of the Internet contributes to reducing rural poverty in Mexico, thus reducing urban–rural income inequality [37]. Yin and Choi (2022) examined the effects of digitalization on income inequality using the panel data of the Group of Twenty countries for 2002–2018. The results suggest that digitalization alleviates income inequality [38]. Others believe that digitalization could exacerbate income inequality [39,40]. By applying a generalized linear mixed model and a random effects model based on Australian household panel data covering 2011–2017, Ali et al. (2019) found that gross information and communication technology affordability is positively associated with income distribution and socioeconomic inequality [41]. Njangang et al. (2022) investigated the effect of digitalization on wealth inequality using panel data for 45 developed and developing countries from 2000 to 2017 and demonstrated that digitalization increases wealth inequality [42].
To sum up, previous research has attempted to investigate the effect of digitalization on public health, but there are factors that still merit improvement. First, the application scenarios for digitalization are rich and diverse from macro to micro. While existing literature mostly focuses on the impact of digitalization on micro health behaviors, there is little literature to interpret the effects of digitalization on public health at the macro level. Second, the mechanisms through which digitalization improves public health in developing countries have not been satisfactorily explained. Third, few studies have analyzed the regional differences in the impact of digitalization on public health in developing countries. Therefore, this study empirically investigates the effect of digitalization on public health and its mechanism using panel data for 81 developing countries from 2002 to 2019.
3. Mechanism analysis and hypothesis
3.1. Digitalization and public health
As the most representative form of the new generation of information technology, digitalization deeply empowers the medical service field, significantly impacting traditional medical services. Meanwhile, digitalization also profoundly affects people's living habits and medical concepts and reshapes health values. First, digitalization integrates into medical services and pharmaceutical research and development with its powerful technology spillover effect, providing a solid medical foundation for residents [43]. Specifically, digitalization acts on traditional medical services. It promotes conventional medical services such as appointment booking, health consultations, price payment, and medical report inquiry to be realized by a mobile network. This not only contributes to optimizing the medical service process and improving the medical service efficiency but also helps break the mode of traditional medical services and maximizes the accessibility of medical services for residents, thus improving public health. Digitalization stimulates pharmaceutical research and development, fully excavates the market demand for pharmaceuticals, quickly analyzes the clinical trial results of pharmaceuticals, and liberates pharmaceutical research and development from the dilemma of high investment, high risk, and long cycle. Digitalization can also produce many medications with effective, rapid, and high curative effects providing a solid material foundation to protect public health. Second, with its powerful knowledge spillover influence, digitalization disseminates health information and helps residents establish correct health concepts. Digitalization eliminates the spatial and temporal barriers to health information dissemination and the costs of health information creation, sharing, and access. It broadens the channels through which residents access health information and health status awareness, improving public health to some extent. For example, residents have gained a wealth of dietary knowledge through online platforms to make healthier food choices [44,45]. Accordingly, we propose Hypothesis 1.
Hypothesis 1
Digitalization has a significant effect on enhancing public health.
3.2. Digitalization, income equality, and public health
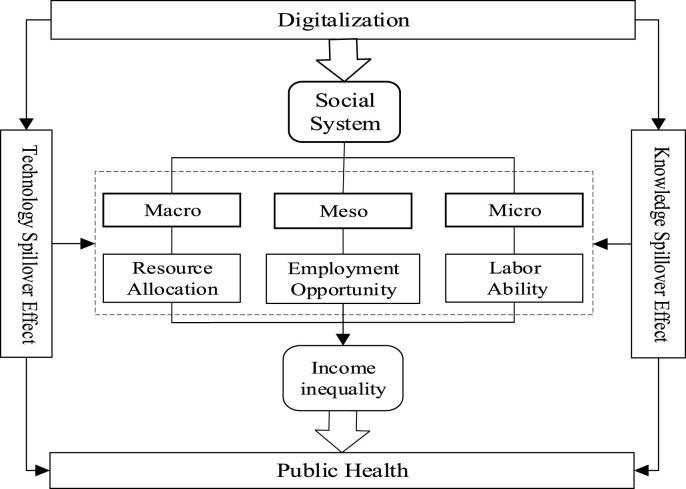
Digitalization directly impacts public health and can indirectly affect public health by reducing income inequality. On the macro level, referring to the center-periphery theory, developing countries do not possess the conditions for balanced development. They can only invest limited resources in some sectors and regions to form a scale economy and then drive the economic development of less developed areas. Digitalization's inter-temporal properties can exponentially amplify the economic drive of developed regions to less developed areas, thus improving resource allocation and narrowing the income gap. On the Mesoscopic level, the deep integration of digitalization and the real economy gives birth to many new industries and business models, which provide additional employment opportunities for low-skilled workers. For example, the upsurge and development of E-commerce brands such as Amazon, Seamless, and Yelp have offered many employment opportunities for low-skilled laborers (couriers and food delivery staff). The increase in employment opportunities and the expansion of the employment scale discourage poverty and income inequality, which improves public health in the long run [19]. On the micro level, digitalization is deeply integrated with education, innovates teaching forms, gathers learning resources, and provides more learning opportunities for groups with limited educational resources [46]. By accessing cutting-edge educational resources, workers in less developed regions continue accumulating labor skills and updating their knowledge, laying a good foundation for earning higher incomes. Therefore, we propose Hypothesis 2 (see Fig. 1 ).
Hypothesis 2
Digitalization can enhance public health by bridging the income gap and reducing income inequality.
Fig. 1.
The impact mechanism of digitalization on public health.
4. Methodology and data
4.1. Methodology
To empirically analyze the impact of digitalization on public health, the following model is set up in this study:
| (1) |
Where the subscripts and represent the country and year, respectively. is the explanatory variable that denotes the level of public health in country in year . is the core independent variable and indicates the level of digitalization in country in year . , , , , , , and are control variables that present the prevalence rate of basic sanitation services, employment rate, financial development, trade freedom, health expenditure, urbanization, and per capita income in the country in year , respectively represents individual effects. denotes time effects. is the residual term.
To further test the validity of Hypothesis 2, drawing on the research ideas of Baron and Kenny (1986), Mackinnon et al. (2007), and others [47,48], we adopt a stepwise regression to test for the existence of a mediating effect. The stepwise regression covers three steps. In addition to Eq. (1), the following two regressions should be constructed.
| (2) |
| (3) |
First, Eq. (1) is estimated to test whether public health is affected by digitalization. Second, the mediating variable of income inequality is regressed against digitalization as shown in Eq. (2). Finally, public health is regressed against both digitalization, income inequality and other variables in Eq. (3). Where is the mediating variable in Eq. (2) and Eq. (3) that denotes the level of income inequality. Other variables have the same meaning as Eq. (1). If in Eq. (2), and in Eq. (3) are significant, then has a partial mediating effect. In contrast, if in Eq. (2) and in Eq. (3) are significant, and in Eq. (3) is insignificant, has a complete mediating effect.
4.2. Variables
Explained variable: public health (). Regarding existing studies, this study adopts both life expectancy () and mortality () as proxies for public health [49,50]. Life expectancy is the average number of years newborns would live, assuming that current mortality levels and patterns remain constant over their lifetimes [51]. The under-5 mortality rate excludes deaths caused by accidents, which is a more accurate indicator of public health than the overall mortality rate [52]. The higher mortality rate, the lower level of public health.
Core independent variable: digitalization (). The deep integration of digitalization with public health provides great convenience for residents to obtain health information, prevent diseases, and receive medical services, thus positively impacting public health outcomes. Drawing on the research methodology of Wang and Xu (2022), this study selects the internet penetration rate () to measure the level of digitalization of a country [53]. Furthermore, this study also includes mobile phone penetration rate () as a proxy variable for internet penetration rate to conduct robustness tests.
Mediating variable: income inequality (). Severe income inequality negatively impacts public health outcomes [54], and this negative impact is mainly manifested in the increased incidence of chronic diseases (cardiovascular diseases and depression) [55]. The GINI may not be the best measure of objective inequality since it fails to adequately capture the income of the richest individuals in particular societies [56]. Moreover, considering the completeness and availability of data, we adopt the top 10% share (the share of total pre-tax national income held by the top 10%) from the World Inequality Database to measure income inequality. The top 10% share is the concentration of cumulative taxable individual income split by couples among the top 10% of a country's population at the current time point [57].
Control variable: (1) prevalence rate of basic sanitation services (). The availability of basic sanitation services such as safe drinking water, clean public toilets, and health education can significantly improve public health and living conditions [58]. This study utilizes the number of people using at least basic sanitation services in the population to indicate. (2) employment rate (). Employment positively shapes residents' physical and mental health by affecting the income of individuals or families [59]. This study uses the percentage of the employed population in the total population over 16 years old to characterize the employment situation, where employment includes both formal and informal employment. (3) financial development (). Driven by the effects of finance on income and education, the residents can afford better food, housing, and education [60] to increase their health level. This study measures financial development by adopting the percentage of domestic credit to the private sector by banks in the gross domestic product (GDP). (4) trade freedom (). Trade freedom refers to the share of total trade in the GDP, which is expected to correlate positively with public health. (5) health expenditure (). Health expenditures are measured by current health expenditures as a share of GDP. Health expenditure reflects the government's public health policy. It is a contributing factor in maintaining national health [61]. (6) urbanization (). Urbanization is represented by the ratio of the urban population to the total population. On the one side, urbanization has brought residents convenient medical services and healthy lifestyles. On the other side, urbanization has caused serious environmental pollution due to the massive population concentration. Therefore, the relationship between urbanization and public health is uncertain. (7) per capita income (). The higher the general income level, the higher the level of public health.
4.3. Data
Following the classification criteria for developed and developing countries launched by the United Nations Conference on Trade and Development (UNCTAD), this study selects 81 developing countries worldwide from 2002 to 2019 as samples. There have been a few years with missing data for explanatory variables, so the moving average method is used to supplement the missing data. The primary data of this study are collected from the World Bank, the World Income Inequality, and the UNCTAD databases. For the empirical estimation, the model variables are log-transformed so that the sharpness in data is diminished and variables show improved distributional properties. Natural logarithmic transformation helps to remove autocorrelation and heteroskedasticity issues from data. Compared to the linear transformation, results derived from log-transformed models are generally consistent and efficient [62,63]. Therefore, all the variables in this study are logarithmically treated. The descriptive statistics of each variable are shown in Table 1 , and the countries are listed in Table 2a, Table 2b a and 2b.
Table 1.
Descriptive statistics of variables.
| 1458 | 67.7995 | 8.4312 | 41.3760 | 83.4980 | |
| 1458 | 7.4224 | 3.2458 | 1.1270 | 21.8300 | |
| 1458 | 25.7086 | 25.3634 | 0.0550 | 99.7010 | |
| 1458 | 74.4593 | 47.8365 | 0.0800 | 212.6390 | |
| 1458 | 0.5068 | 0.0660 | 0.3637 | 0.7155 | |
| 1458 | 64.9742 | 29.4286 | 5.0377 | 100.0000 | |
| 1458 | 66.0702 | 11.4559 | 41.4700 | 90.3400 | |
| 1458 | 36.9857 | 28.8917 | 0.0074 | 165.3904 | |
| 1458 | 41.7698 | 22.4415 | 10.6663 | 208.3329 | |
| 1458 | 5.2578 | 2.1111 | 1.2636 | 20.4134 | |
| 1458 | 55.6878 | 21.3222 | 14.2398 | 100.0000 | |
| 1458 | 6740.3790 | 10538.4700 | 278.3194 | 65129.3800 |
Table 2a.
List of sample countries in this research by geographic locations.
| Asia | Africa | The Americas | |||
|---|---|---|---|---|---|
| Armenia | Azerbaijan | Algeria | Angola | Argentina | Chile |
| Bahrain | Bangladesh | Benin | Botswana | Barbados | Colombia |
| Bhutan | Cambodia | Cameroon | Burundi | Belize | Costa Rica |
| China | Georgia | Chad | Comoros | Bolivia | Haiti |
| India | Indonesia | Gabon | Egypt | Brazil | Ecuador |
| Saudi Arabia | United Arab Emirates | Equatorial Guinea | Côte d'Ivoire | El Salvador | Dominican Republic |
| Jordan | Kazakhstan | Gambia | Ghana | Guatemala | Honduras |
| Iraq | Pakistan | Guinea | Madagascar | Jamaica | Nicaragua |
| Kuwait | Qatar | Mali | Mauritania | Mexico | Panama |
| Kyrgyzstan | Iran | Mauritius | Morocco | Paraguay | Peru |
| Lebanon | Singapore | Mozambique | Namibia | ||
| Malaysia | Tajikistan | Niger | Nigeria | ||
| Mongolia | Thailand | Rwanda | Senegal | ||
| Nepal | Turkey | Sierra Leone | South Africa | ||
| Oman | Tanzania | Togo | |||
| Tunisia | Kenya | ||||
Table 2b.
List of sample countries in this research by income level.
| High-income country | Bahrain |
Barbados |
Chile |
Kuwait |
Singapore |
United Arab Emirates |
|---|---|---|---|---|---|---|
| Oman | Panama | Qatar | Saudi Arabia | |||
| Middle-income country | Algeria | Argentina | Angola | Azerbaijan | Bangladesh | Costa Rica |
| Armenia | Botswana | Belize | Brazil | Cambodia | Colombia | |
| Benin | Bolivia | Bhutan | Cameroon | China | Comoros | |
| Gabon | Georgia | Ghana | Egypt | Ecuador | Côte d'Ivoire | |
| Guatemala | Honduras | India | Indonesia | Iran | Dominican Republic | |
| Iraq | Jamaica | Jordan | Kazakhstan | Kenya | El Salvador | |
| Kyrgyzstan | Lebanon | Malaysia | Mauritania | Mexico | Equatorial Guinea | |
| Mongolia | Morocco | Namibia | Nepal | Nicaragua | South Africa | |
| Pakistan | Paraguay | Senegal | Peru | Tunisia | Tanzania | |
| Thailand | Nigeria | Turkey | Mauritius | |||
| Low-income country | Burundi | Chad | Guinea | Madagascar | Rwanda | Mozambique |
| Tajikistan | Gambia | Haiti | Mali | Niger | Sierra Leone | |
| Togo |
5. Results and discussion
5.1. Results of benchmark regression
To empirically analyze the logical relationship between digitalization and public health, this study employs the classical static panel model for the regression estimation of Eq. (1). The estimation results are shown in Table 3 . As shown in Table 3, in the regression results with life expectancy as a proxy variable for public health (columns (1)–(3)), the F-test for the fixed effects model versus the least square method indicates that the fixed effects model should be chosen. The results of the Hausman-test for the fixed effects model versus the random effect model also denote that the fixed effects model should be selected.
Table 3.
The result of benchmark regression.
|
|
|
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| 0.0197*** (10.1300) | 0.0187*** (18.3193) | 0.0195*** (20.6744) | −0.0338*** (−3.6841) | −0.0648*** (−17.0538) | −0.0588*** (−16.3367) | |
| 0.0939*** (19.9681) | 0.0296*** (4.3675) | 0.0456*** (7.1513) | −0.1769*** (−7.9949) | −0.2073*** (−8.2038) | −0.2110*** (−8.6587) | |
| 0.0184* (1.6721) | 0.0335* (1.7348) | 0.0455** (2.5478) | −0.0510 (−0.9819) | −0.0213 (−0.2968) | −0.0549 (−0.7991) | |
| 0.0279*** (9.4523) | 0.0013 (0.6701) | 0.0019 (0.9819) | −0.0798*** (−5.7482) | −0.0087 (−1.1930) | −0.0083 (−1.1216) | |
| 0.0068 (1.6213) | 0.0105*** (3.0096) | 0.0097*** (2.7974) | −0.0720*** (−3.6594) | −0.0139 (−1.0704) | −0.0224* (−1.7295) | |
| 0.0032 (0.6457) | −0.0133*** (−3.2879) | −0.0132*** (−3.2775) | 0.1961*** (8.3156) | 0.1333*** (8.8771) | 0.1377*** (9.1771) | |
| −0.0092 (−1.3665) | 0.1717*** (10.4516) | 0.1151*** (8.4242) | −0.0810** (−2.5621) | −0.2720*** (−4.4443) | −0.3002*** (−5.5112) | |
| 0.0093*** (3.0131) | 0.0076 (1.4818) | 0.0069 (1.5264) | −0.0871*** (−5.9861) | 0.1796*** (9.4098) | 0.1319*** (7.4627) | |
| 3.5461*** (63.6154) | 3.1453*** (30.9507) | 3.2579*** (36.0155) | 4.1424*** (15.7896) | 2.4724*** (6.5305) | 3.1307*** (8.8632) | |
| 0.7089 | 0.7070 | 0.7038 | 0.5050 | 0.5620 | 0.5593 | |
| 0.0000 | 0.0000 | |||||
| 0.0000 | 0.0000 | |||||
Note: "***", "**", and "*" mean significance at the level of 0.01, 0.05, and 0.1, respectively; t value in parehtheses.
In column (2), regarding the core explanatory variables, the coefficient of digitalization is significantly positive, indicating that Hypothesis 1 holds and digitalization significantly enhances public health. This may be due to the following reasons: first, digitalization empowers medical service links and innovates new medical service models, such as online consultation and telemedicine, which effectively solve the lack of medical resources and greatly improve medical services efficiency, making basic medical services accessible to everyone. Second, digitalization can provide the impetus for health knowledge dissemination links. Through official media, personal video blog or log (VLOG), and other ways, digitalization can embed in disseminating health knowledge so that health knowledge is deeply involved in public life and transforms unhealthy habits.
Regarding control variables, the prevalence rate of basic sanitation services is significantly positive, suggesting that the prevalence rate of basic sanitation services can efficiently improve public health care conditions, which in turn positively impacts public health. The estimated coefficient of the employment rate is positive, reflecting that increasing the employment rate is an effective path to improve public health, which is consistent with the conclusion of Heggebo and Dahl (2015). The estimated coefficient of financial development is positive but insignificant, probably because the level of financial development in developing countries cannot yet positively affect public health at this stage. The coefficient of trade freedom is estimated to be significantly positive, which aligns with the research results of Archana (2020). Trade freedom enables the import of diverse foods to enrich the residents' diet and thus protect public health. The coefficient for the health expenditure variable is negative, and the association is significant. Health expenditure is regarded as one of the most important indicators for examining the government's performance in public health, and the negative coefficient of health expenditure indicates a lot of wasted resources in the public health system, which seriously reduces the efficiency of public health expenditure in developing countries [64]. The coefficient of urbanization is statistically significant at the 1% level. The medical and health services levels are compatible with urbanization development [65]. As urbanization levels rise, sanitation facilities continue to improve, which benefits public health outcomes. Per capita income positively impacts public health, but insignificant.
Life expectancy and mortality are like the tails of a coin. Therefore, the variables theoretically act in the opposite direction for mortality as they do for life expectancy. In the regression results with mortality as a proxy variable for public health (columns (4)–(6)), the estimated coefficient of the digitalization is significantly negative, consistent with the expectation that digitalization has a significant suppressive effect on under-5 mortality. The sign of the coefficients of the other control variables is essentially opposite to the regression results in columns (1)–(3), demonstrating the robustness of the benchmark regression results.
5.2. Robustness test
To further evaluate whether the assumptions are valid, this study performs robustness tests by replacing both estimation methods and core explanatory variables. First, we adopt the system generalized method of moments (GMM) to replace the fixed effects model for re-estimating equation (1). Due to the applicability condition of the system GMM, the lagged period of the explanatory variables is included in equation (1) [66]. The estimation results are reported in Table 4 (columns (1)–(2)). Second, we use mobile phone penetration as an indicator to measure the development of digitalization and re-estimate equation (1). The estimation results are shown in Table 4 (columns (3)–(4)). In Table 4, the regression results express that the coefficient of digitalization on life expectancy is significantly positive and on mortality is significantly negative for either method, proving that the benchmark regression results are robust.
Table 4.
The result of the robustness test.
| VARIABLES | Replacing estimation method |
Replacing the core explanatory variable |
||
|---|---|---|---|---|
| (1) |
(2) |
(3) |
(4) |
|
| 0.9173*** (237.1867) | ||||
| 0.9699*** (299.5643) | ||||
| 0.0008*** (4.2669) | −0.0037*** (−6.0750) | 0.0128*** (13.0240) | −0.0470*** (−13.0041) | |
| 0.0073*** (6.1089) | 0.0890*** (10.6527) | 0.0393*** (5.5231) | −0.2361*** (−9.0240) | |
| 0.0329*** (7.2728) | 0.0190 (1.3576) | 0.0569*** (2.8079) | −0.1023 (−1.3735) | |
| −0.0009*** (−2.6732) | −0.0171*** (−6.2657) | 0.0054*** (2.6367) | −0.0215*** (−2.8589) | |
| 0.0050*** (10.8712) | −0.0244*** (−18.9626) | −0.0072* (−1.7035) | 0.1125*** (7.2346) | |
| 0.0004 (1.1556) | 0.0743*** (14.6276) | 0.2327*** (14.0844) | −0.4737*** (−7.7960) | |
| −0.0075*** (−3.9519) | −0.0158** (−2.3233) | 0.0039 (1.0473) | 0.0102 (0.7523) | |
| 0.0042*** (8.8933) | −0.0258*** (−9.1141) | 0.0100* (1.8241) | 0.1759*** (8.7230) | |
| Constant | 0.1653*** (9.8448) | −0.0818 (−1.0485) | 2.7470*** (27.1281) | 3.7574*** (10.0921) |
| 0.0670 | 0.0910 | |||
| 0.1270 | 0.3480 | |||
| 0.6690 | 0.6060 | |||
| R-squared | 0.6751 | 0.5272 | ||
Note: "***", "**", and "*" mean significance at the level of 0.01, 0.05, and 0.1, respectively; t value in parehtheses.
5.3. Heterogeneity analysis
5.3.1. Regression analysis of different geographic locations
Regarding the benchmark regression, it analyzes the impact of digitalization on public health in an average sense. It concludes that digitalization remarkably contributes to public health in developing countries. In order to explore whether a difference exists in the impact of digitalization on public health in different geographic locations, the overall sample is divided into three subsamples: Asia, Africa, and the Americas. As shown in Table 5 , in the regression results in columns (1)–(3), the lengthening effect of digitalization on life expectancy is much greater in Africa than in Asia and the Americas. In the regression results in columns (4)–(6), the suppression effect of digitalization on mortality is also much higher in Africa than in Asia and the Americas. Overall, the health benefits of digitalization are most pronounced in Africa, followed by Asia and the Americas. In general, it is plausible to expect income elasticity to change as the income level grows; when a country is poor, a lot of goods and services are regarded by its citizens as luxuries. However, when people are wealthy, luxuries may become necessities [67]. Therefore, the possible reason is that the economies of developing African countries grow relatively slower than those in Asia and the Americas. African residents face more stringent household economic constraints than those in Asia and the Americas. They often disregard healthcare spending in favor of higher savings when weighing household savings and healthcare. Their physical and mental health is often not effectively protected. In other words, health is a luxury good for African residents [68]. A small change in the price of health brought about by digitalization can induce a large variation in health consumption by African residents. Health is a necessity good for Asian and American residents. Digitalization brings a significant change in prices but only causes a slight change in health consumption for Asian and American residents. As a result, African public health is the most sensitive to digitalization.
Table 5.
The result of the heterogeneity test based on geographic locations.
| VARIABLES |
|
|
||||
|---|---|---|---|---|---|---|
| (1) Asia |
(2) Africa |
(3) The Americas |
(4) Asia |
(5) Africa |
(6) The Americas |
|
| 0.0089*** (8.1298) | 0.0264*** (13.6201) | 0.0042*** (3.0165) | −0.0441*** (−8.4188) | −0.0700*** (−7.3233) | −0.0381*** (−5.4272) | |
| 0.0088 (1.3244) | 0.0105 (0.8712) | 0.0945*** (9.4306) | −0.0793** (−2.5125) | −0.1869*** (−4.8488) | −0.5530*** (−10.8404) | |
| 0.0898*** (4.4802) | 0.1894*** (4.9717) | −0.0061 (−0.3413) | −0.3796*** (−3.9689) | −0.5028*** (−4.0508) | 0.0743 (0.8159) | |
| −0.0015 (−0.5911) | 0.0082*** (2.8142) | −0.0137*** (−5.2351) | −0.0036 (−0.2900) | −0.0244** (−2.5402) | 0.0563*** (4.2150) | |
| −0.0086** (−2.1874) | 0.0170*** (2.8849) | 0.0003 (0.0779) | 0.0508*** (2.6994) | −0.0423** (−2.1157) | 0.0741*** (3.9367) | |
| −0.0003 | −0.0092 (−1.3760) | 0.0062 (1.1565) | 0.1152*** (5.4602) | 0.1036*** (4.7436) | −0.0397 (−1.4591) | |
| (-0.0704) | ||||||
| 0.1600*** | 0.1359*** (4.1965) | 0.0227 (1.4719) | −0.1860** (−2.3079) | −0.1138 (−1.0585) | −0.0309 (−0.3937) | |
| (9.4709) | ||||||
| 0.0263*** (4.6388) | 0.0730*** (6.2133) | 0.0091* (1.6659) | 0.1001*** (3.7009) | −0.0404 (−1.0290) | 0.0793*** (2.8529) | |
| 3.0134*** (29.0245) | 2.1061*** (10.4910) | 3.7520*** (39.9566) | 3.2369*** (6.5349) | 5.8905*** (8.4828) | 2.9609*** (6.1943) | |
| 0.7355 | 0.8055 | 0.8674 | 0.3859 | 0.7933 | 0.4936 | |
Note: "***", "**", and "*" mean significance at the level of 0.01, 0.05, and 0.1, respectively; t value in parehtheses.
5.3.2. Regression analysis of different income levels
The sample countries were classified as high-income, middle-income and low-income countries based on the World Bank standard, the regression statistics were categorized, to verify whether heterogeneity exists in the impact of digitalization on public health in countries with different income levels. The regression results are displayed in Table 6 . In columns (1)–(3), digitalization passed the significance test in high-, middle- and low-income countries, with impact coefficients of 0.0038, 0.0164, and 0.0139, respectively. Notably, these results coincide with the results of the heterogeneity of the geographic locations above, as most countries in Africa are middle- and low-income countries, and most countries in Asia and the Americas are middle- and high-income countries [69], which further confirms the robustness of the heterogeneity results. As discussed above, public health is necessary for middle- and high-income countries and a luxury for low-income countries. Smaller changes in digitalization can cause larger changes in public health in low-income countries. Therefore, the elasticity coefficient of digitalization is higher in low-income countries than in middle- and high-income countries.
Table 6.
The result of the heterogeneity test based on the income level.
| VARIABLES |
|
|
||||
|---|---|---|---|---|---|---|
| (1) High-income |
(2) Middle-income |
(3) Low-income |
(4) High-income |
(5) Middle-income |
(6) Low-income |
|
| 0.0038** (2.4354) | 0.0164*** (13.6012) | 0.0139*** (6.7428) | −0.0365*** (−2.9764) | −0.0538*** (−11.9006) | −0.0442*** (−6.9509) | |
| 0.0730*** (3.2886) | 0.0188*** (2.6477) | 0.0072 (0.3896) | 0.5718*** (3.2951) | −0.1714*** (−6.4614) | −0.1317** (−2.3081) | |
| 0.1369*** (6.3683) | 0.1762*** (8.3488) | −0.3506*** (−3.9627) | −0.1893 (−1.1259) | −0.3852*** (−4.8792) | 0.7821*** (2.8634) | |
| 0.0111*** (3.5320) | 0.0006 (0.2997) | 0.0178*** (2.6668) | −0.1244*** (−5.0512) | −0.0060 (−0.8202) | −0.0469** (−2.2704) | |
| −0.0035 (−1.1029) | −0.0027 (−0.6865) | 0.0271*** (3.6332) | −0.0112 (−0.4507) | 0.0371** (2.5152) | −0.0468** (−2.0319) | |
| 0.0066** (2.3170) | −0.0294*** (−6.0296) | −0.0161* (−1.8066) | 0.2548*** (11.4607) | 0.1967*** (10.7970) | 0.0882*** (3.2118) | |
| −0.0469* (−1.7095) | 0.2509*** (14.4535) | 0.2044*** (4.2609) | −1.4280*** (−6.6604) | −0.5030*** (−7.7480) | −0.4322*** (−2.9185) | |
| 0.0157*** (4.0841) | −0.0140** (−2.4656) | 0.1124*** (6.1643) | 0.1786*** (5.9320) | 0.2375*** (11.1935) | −0.4055*** (−7.2017) | |
| 3.4176*** (25.7094) | 2.5440*** (22.8544) | 3.9542*** (9.4543) | 4.1317*** (3.9749) | 4.0189*** (9.6534) | 3.6966*** (2.8628) | |
| 0.8558 | 0.7350 | 0.8492 | 0.7364 | 0.5571 | 0.8583 | |
Note: "***", "**", and "*" mean significance at the level of 0.01, 0.05, and 0.1, respectively; t value in parehtheses.
5.4. Mechanism analysis
In this study, the income inequality is taken as a mediating variable to test the validity of Hypothesis 2 by using the previous mediating effects model (Eq. (1)–Eq. (3)). The results of the test are shown in Table 7 .
Table 7.
The result of the mechanism analysis.
| VARIABLES | (1) |
(2) |
(3) |
(4) |
(5) |
(6) |
|---|---|---|---|---|---|---|
| 0.0187*** (18.3193) | −0.0125*** (−6.2012) | 0.0182*** (17.6587) | −0.0648*** (−17.0538) | −0.0125*** (−6.2012) | −0.0630*** (−16.4076) | |
| −0.0372*** (−2.7292) | 0.1388*** (2.7298) | |||||
| 0.0296*** (4.3675) | 0.0395*** (2.9487) | 0.0311*** (4.5808) | −0.2073*** (−8.2038) | 0.0395*** (2.9487) | −0.2128*** (−8.4140) | |
| 0.0335* (1.7348) | −0.1218*** (−3.1969) | 0.0289 (1.4975) | −0.0213 (−0.2968) | −0.1218*** (−3.1969) | −0.0044 (−0.0614) | |
| 0.0013 (0.6701) | −0.0054 (−1.3929) | 0.0011 (0.5685) | −0.0087 (−1.1930) | −0.0054 (−1.3929) | −0.0080 (−1.0923) | |
| 0.0105*** (3.0096) | 0.0162** (2.3522) | 0.0111*** (3.1837) | −0.0139 (−1.0704) | 0.0162** (2.3522) | −0.0162 (−1.2439) | |
| −0.0133*** (−3.2879) | 0.0086 (1.0856) | −0.0129*** (−3.2142) | 0.1333*** (8.8771) | 0.0086 (1.0856) | 0.1321*** (8.8141) | |
| 0.1717*** (10.4516) | −0.1235*** (−3.8042) | 0.1671*** (10.1421) | −0.2720*** (−4.4443) | −0.1235*** (−3.8042) | −0.2549*** (−4.1522) | |
| 0.0076 (1.4818) | 0.0260** (2.5736) | 0.0086* (1.6711) | 0.1796*** (9.4098) | 0.0260** (2.5736) | 0.1760*** (9.2198) | |
| 3.1453*** (30.9507) | 4.5191*** (22.5066) | 3.3136*** (27.9234) | 2.4724*** (6.5305) | 4.5191*** (22.5066) | 1.8452*** (4.1738) | |
| 0.7070 | 0.1130 | 0.7080 | 0.5620 | 0.1130 | 0.5640 |
Note: "***", "**", and "*" mean significance at the level of 0.01, 0.05, and 0.1, respectively; t value in parehtheses.
In Table 7, columns (1)–(3) report the estimated results of the mediating effects model with life expectancy as a proxy variable for public health. From the regression results in column (1), the total effect of digitalization on life expectancy is significantly positive at the 1% level. For every 1% increase in digitalization, life expectancy increases by 0.0187%. The regression results in column (2) show that the improvement in digitalization significantly suppresses income inequality. In column (3), the coefficient of income inequality is significantly negative, demonstrating that income inequality adversely influences life expectancy. The coefficient of digitalization remains significantly positive after controlling for income inequality, implying that digitalization directly contributes to life expectancy. Meanwhile, since the coefficients correspond to , and in columns (1)–(3) of Table 7 are significant, a mediating effect exists, which accounts for 2.4866% of the total effect.
Columns (4)–(6) report the estimated results of the mediating effects model with mortality as a proxy variable for public health. The total effect of digitalization on mortality is significant at the 1% level, as shown by the regression results in column (4). For every 1% increase in digitalization, the mortality rate decreases by −0.0648%. The regression results in column (5) are the same as in column (2). In column (6), the coefficient of income inequality is significantly positive, which implies that income inequality significantly contributes to mortality. However, the digitalization coefficient is significantly negative, indicating that digitalization negatively correlates with mortality. The coefficients corresponding to , and in columns (4)–(6) of Table 7 remain significant, so the mediating effect is still present, accounting for 2.6775% of the total effect. Thus, there are effective mechanisms for digitalization to improve public health by suppressing income inequality, whether life expectancy is used as a proxy variable for public health or mortality is used as a proxy variable.
6. Conclusion and policy implications
With the development of the Mobile Internet, the Internet of Things, and other digital information technology, digitalization forcefully penetrates people's daily lives and profoundly transform people's lifestyles and health concepts. In this research, applying the panel data of 81 developing countries from 2002 to 2019, the impact and mechanism of digitalization on public health in developing countries are investigated. The following conclusions have been reached. First, digitalization can effectively improve public health in developing countries. After accounting for endogeneity issues arising from measurement error, omitted variables, and bidirectional causality, this core conclusion remains robust. Second, further heterogeneity analysis reveals that the enhancing effect of digitalization on public health in Africa and middle-income countries is the most pronounced. Third, from the perspective of the mechanism, the enhancing impact of digitalization on public health can be achieved by alleviating income inequality.
This research provides an impetus to recognize the effect of digitalization on public health and put forward some workable policy implications for developing countries. First, developing countries could carry out priority strategies for digital infrastructure development so that residents have the opportunity and ability to enjoy the digital dividend. On the one hand, if possible developing countries can increase investment in digital infrastructure and perfect the construction of the Internet of Things, cloud computing, and big data platforms. On the other hand, in association with social welfare organizations, the government can provide rich guidance on using digital technology for residents. For example, through public service training seminars on how to use the Internet, residents can improve their Internet skills. Second, countries should strengthen the inhibiting effect of digitalization on income inequality and strive to realize the in-depth integration of the digital revolution and fair income distribution. Regarding employment security, the government could take the initiative to explore new paths to integrate digitalization and employment security systems and strengthen the employment-absorbing function of digitalization. In terms of the income distribution, developing countries should establish rules and standards for income distribution that are uniform, concise, and easy to implement; give full play to the regulatory effectiveness of digitalization; and promote intelligent, precise, and standardized income regulation. Finally, if possible the government should encourage hospitals to innovate digital application scenarios, enrich the ways and channels of medical treatment, address the problem of limited and uneven distribution of medical resources, and provide solid medical protection for public health.
Credit author statement
Jing Wang: Conceptualization, Methodology, Supervision, Funding acquisition, Data curation, formal analysis, Writing- Reviewing and Editing. Yubing Xu: Software, Data curation, Writing- Original draft preparation, formal analysis.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work was supported by Heilongjiang Social Science Foundation (Grant No. 20JLB101).
Footnotes
Data availability
Data will be made available on request.
References
- 1.Lin Y.H., Liu C.H., Chiu Y.C. Google searches for the keywords of "wash hands" predict the speed of national spread of COVID-19 outbreak among 21 countries. Brain Behav. Immun. 2020;87:30–32. doi: 10.1016/j.bbi.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guzel A.E., Arslan U., Acaravci A. The impact of economic, social, and political globalization and democracy on life expectancy in low-income countries: are sustainable development goals contradictory? Environ. Dev. Sustain. 2021;23(9):13508–13525. doi: 10.1007/s10668-021-01225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee B.X., Kjaerulf F., Turner S., Cohen L., Donnelly P.D., Muggah R., Davis R., Realini A., Kieselbach B., MacGregor L.S. Transforming our world: implementing the 2030 agenda through sustainable development goal indicators. J. Publ. Health Pol. 2016;37(1):13–31. doi: 10.1057/s41271-016-0002-7. [DOI] [PubMed] [Google Scholar]
- 4.Dzambazovic R., Gerbery D. Socio-economic inequalities in health: socio-economic status as a determinant of health. Sociologia. 2014;46(2):194–219. [Google Scholar]
- 5.Herzer D. The macro-level effect of religiosity on health. Health Econ. 2022;31(6):993–1011. doi: 10.1002/hec.4494. [DOI] [PubMed] [Google Scholar]
- 6.Karanika-Murray M., Bartholomew K.J., Williams G.A., Cox T. Leader-Member Exchange across two hierarchical levels of leadership: concurrent influences on work characteristics and employee psychological health. Work. Stress. 2015;29(1):57–74. doi: 10.1080/02678373.2014.1003994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee H.Y., Zhou A.Q., Lee R.M., Dillon A.L. Parents' functional health literacy is associated with children's health outcomes: implications for health practice, policy, and research. Child. Youth Serv. Rev. 2020;110 [Google Scholar]
- 8.Alvarez E.C., Kawachi I., Romani J.R. Family social capital and health - a systematic review and redirection. Sociol. Health Illness. 2017;39(1):5–29. doi: 10.1111/1467-9566.12506. [DOI] [PubMed] [Google Scholar]
- 9.Hawkes C. The role of foreign direct investment in the nutrition transition. Publ. Health Nutr. 2005;8(4):357–365. doi: 10.1079/phn2004706. [DOI] [PubMed] [Google Scholar]
- 10.Yang T.R., Liu W.L. Does air pollution affect public health and health inequality? Empirical evidence from China. J. Clean. Prod. 2018;203:43–52. [Google Scholar]
- 11.Subramanian S.V., Kawachi I. Income inequality and health: what have we learned so far? Epidemiol. Rev. 2004;26(1):78–91. doi: 10.1093/epirev/mxh003. [DOI] [PubMed] [Google Scholar]
- 12.He Y., Li K., Wang Y. Crossing the digital divide: the impact of the digital economy on elderly individuals' consumption upgrade in China. Technol. Soc. 2022;71 [Google Scholar]
- 13.Sandri S., Alshyab N., Sha'Ban M. The effect of digitalization on unemployment reduction. NEW MEDIT. 2022;21(4):29–39. [Google Scholar]
- 14.Iyamu I., Xu A.X.T., Gómez-Ramírez O., Ablona A., Chang H.-J., McKee G., Gilbert M. Defining digital public health and the role of digitization, digitalization, and digital transformation: scoping review. JMIR Public Health Surveill. 2021;7(11) doi: 10.2196/30399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hildebrand V., Van Kerm P. Income inequality and self-rated health status: evidence from the european community household panel. Demography. 2009;46(4):805–825. doi: 10.1353/dem.0.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curran M., Mahutga M.C. Income inequality and population health: a global gradient? J. Health Soc. Behav. 2018;59(4):536–553. doi: 10.1177/0022146518808028. [DOI] [PubMed] [Google Scholar]
- 17.Spencer N. The effect of income inequality and macro-level social policy on infant mortality and low birthweight in developed countries – a preliminary systematic review. Child Care Health Dev. 2004;30(6):699–709. doi: 10.1111/j.1365-2214.2004.00485.x. [DOI] [PubMed] [Google Scholar]
- 18.Kawachi I., Kennedy B.P. Income inequality and health: pathways and mechanisms. Health Serv. Res. 1999;34(1 Pt 2):215–227. [PMC free article] [PubMed] [Google Scholar]
- 19.Marmot M., Wilkinson R.G. Psychosocial and material pathways in the relation between income and health: a response to Lynch et al. BMJ. 2001;322(7296):1233. doi: 10.1136/bmj.322.7296.1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Odgers C.L., Jensen M.R. Annual Research Review: adolescent mental health in the digital age: facts, fears, and future directions. JCPP (J. Child Psychol. Psychiatry) 2020;61(3):336–348. doi: 10.1111/jcpp.13190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McMullan M. Patients using the Internet to obtain health information: how this affects the patient–health professional relationship. Patient Educ. Counsel. 2006;63(1):24–28. doi: 10.1016/j.pec.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Sims T., Reed A.E., Carr D.C. Information and communication technology use is related to higher well-being among the oldest-old. J. Gerontol.: Ser. Bibliogr. 2017;72(5):761–770. doi: 10.1093/geronb/gbw130. [DOI] [PubMed] [Google Scholar]
- 23.Cotten S.R., Ford G., Ford S., Hale T.M. Internet use and depression among retired older adults in the United States: a longitudinal analysis. J. Gerontol.: Ser. Bibliogr. 2014;69(5):763–771. doi: 10.1093/geronb/gbu018. [DOI] [PubMed] [Google Scholar]
- 24.Ma X., Zhang X., Guo X., Lai K.-h., Vogel D. Examining the role of ICT usage in loneliness perception and mental health of the elderly in China. Technol. Soc. 2021;67 [Google Scholar]
- 25.Odone A., Buttigieg S., Ricciardi W., Azzopardi-Muscat N., Staines A. Public health digitalization in Europe: EUPHA vision, action and role in digital public health European. J. Publ. Health. 2019;29(Supplement_3):28–35. doi: 10.1093/eurpub/ckz161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang J.P., Gong X.M., Zhang H. ICT diffusion and health outcome: effects and transmission channels. Telematics Inf. 2022;67 [Google Scholar]
- 27.Bessière K., Pressman S., Kiesler S., Kraut R. Effects of internet use on health and depression: a longitudinal study. J. Med. Internet Res. 2010;12(1):e6. doi: 10.2196/jmir.1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sami H., Danielle L., Lihi D., Elena S. The effect of sleep disturbances and internet addiction on suicidal ideation among adolescents in the presence of depressive symptoms. Psychiatr. Res. 2018;267:327–332. doi: 10.1016/j.psychres.2018.03.067. [DOI] [PubMed] [Google Scholar]
- 29.Bozkurt H., Özer S., Şahin S., Sönmezgöz E. Internet use patterns and Internet addiction in children and adolescents with obesity. Pediatric Obesity. 2018;13(5):301–306. doi: 10.1111/ijpo.12216. [DOI] [PubMed] [Google Scholar]
- 30.Dutta-Bergman M.J. Health attitudes, health cognitions, and health behaviors among internet health information seekers: population-based survey. J. Med. Internet Res. 2004;6(2):e15. doi: 10.2196/jmir.6.2.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dalton J.A., Rodger D.L., Wilmore M., Skuse A.J., Humphreys S., Flabouris M., Clifton V.L. Who's afraid?”: attitudes of midwives to the use of information and communication technologies (ICTs) for delivery of pregnancy-related health information. Women Birth. 2014;27(3):168–173. doi: 10.1016/j.wombi.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 32.Wilkinson R.G. Socioeconomic determinants of health: health inequalities: relative or absolute material standards? BMJ. 1997;314(7080):591. doi: 10.1136/bmj.314.7080.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang S., Gao B. A fresh evidence of income inequality and health outcomes asymmetric linkages in emerging asian economies. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.791960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu Q., Zhong M.R. The impact of income inequity on energy consumption: the moderating role of digitalization. J. Environ. Manag. 2023;325 doi: 10.1016/j.jenvman.2022.116464. [DOI] [PubMed] [Google Scholar]
- 35.Ahmed A., Al-Roubaie A. Poverty reduction in the Arab world: the use of ICTs. World J. Sci. Tech. Sustain. Develop. 2013;10(3):195–211. [Google Scholar]
- 36.Faizah C., Yamada K., Pratomo D.S. Information and communication technology, inequality change and regional development in Indonesia. J. Socioeco. Develop. 2021;4(No 2) doi: 10.31328/jsed.v4i2.2669. OctoberDO -2021. [DOI] [Google Scholar]
- 37.Mora-Rivera J., García-Mora F. Internet access and poverty reduction: evidence from rural and urban Mexico. Telecommun. Pol. 2021;45(2) [Google Scholar]
- 38.Yin Z.H., Choi C.H. Does digitalization contribute to lesser income inequality? Evidence from G20 Countries. Inform. Tech. Develop. 2022 [Google Scholar]
- 39.Guellec D., Paunov C. National Bureau of Economic Research; 2017. Digital Innovation and the Distribution of Income. [Google Scholar]
- 40.Mohd Daud S.N., Ahmad A.H., Ngah W.A.S.W. Financialization, digital technology and income inequality. Appl. Econ. Lett. 2021;28(16):1339–1343. [Google Scholar]
- 41.Ali M.A., Alam K., Taylor B., Rafiq S. Do income distribution and socio-economic inequality affect ICT affordability? Evidence from Australian household panel data. Econ. Anal. Pol. 2019;64:317–328. [Google Scholar]
- 42.Njangang H., Beleck A., Tadadjeu S., Kamguia B. Do ICTs drive wealth inequality? Evidence from a dynamic panel analysis. Telecommun. Pol. 2022;46(2) [Google Scholar]
- 43.Fang P., Xie Q., Hu T. The relationship between internet industry and health care service. Chinese Journal of Health Policy. 2016;9(1):65–68. [Google Scholar]
- 44.Ma B.J., Jin X. Does internet use connect us to a healthy diet? Evidence from rural China. Nutrients. 2022;14(13) doi: 10.3390/nu14132630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kuhn P., Skuterud M. Internet job search and unemployment durations. Am. Econ. Rev. 2004;94(1):218–232. [Google Scholar]
- 46.Psacharopoulos G., Montenegro C., Patrinos H.A. Education financing priorities in developing countries. J. Educ. Plann. Adm. 2017;31(1):5–16. [Google Scholar]
- 47.Baron R.M., Kenny D.A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 48.MacKinnon D.P., Fairchild A.J., Fritz M.S. Mediation analysis. Annu. Rev. Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mooney G. The spirit level: why more equal societies almost always do better. Local Econ. 2010;24:705–706. [Google Scholar]
- 50.Lu Z.-N., Chen H., Hao Y., Wang J., Song X., Mok T.M. The dynamic relationship between environmental pollution, economic development and public health: evidence from China. J. Clean. Prod. 2017;166:134–147. [Google Scholar]
- 51.Bergh A., Nilsson T. Good for living? On the relationship between globalization and life expectancy. World Dev. 2010;38(9):1191–1203. [Google Scholar]
- 52.Currie J. Healthy, wealthy, and wise: socioeconomic status, poor health in childhood, and human capital development. J. Econ. Lit. 2009;47(1):87–122. [Google Scholar]
- 53.Wang J., Xu Y.B. How does digitalization affect haze pollution? The mediating role of energy consumption. Int. J. Environ. Res. Publ. Health. 2022;19(18) doi: 10.3390/ijerph191811204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wilkinson R.G., Pickett K.E. Income inequality and population health: a review and explanation of the evidence. Soc. Sci. Med. 2006;62(7):1768–1784. doi: 10.1016/j.socscimed.2005.08.036. [DOI] [PubMed] [Google Scholar]
- 55.Doorslaer E.v., Koolman X. Explaining the differences in income-related health inequalities across European countries. Health Econ. 2004;13(7):609–628. doi: 10.1002/hec.918. [DOI] [PubMed] [Google Scholar]
- 56.Chandy L., Seidel B. vol. 17. Brookings Institute; 2017. (How Much Do We Really Know about Inequality within Countries Around the World? Adjusting Gini Coefficients for Missing Top Incomes). [Google Scholar]
- 57.Haddon E., Wu C. How does actual inequality shape people's perceptions of inequality? A class perspective. Socio. Perspect. 2021;65(5):825–847. [Google Scholar]
- 58.Zhao Y., Cui S., Yang J., Wang W., Guo A., Liu Y., Liang W. Basic public health services delivered in an urban community: a qualitative study. Publ. Health. 2011;125(1):37–45. doi: 10.1016/j.puhe.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Julia M., Vanroelen C., Bosmans K., Van Aerden K., Benach J. Precarious employment and quality of employment in relation to health and well-being in Europe. Int. J. Health Serv. 2017;47(3):389–409. doi: 10.1177/0020731417707491. [DOI] [PubMed] [Google Scholar]
- 60.Claessens S., Feijen E. World Bank Publications; 2007. Financial Sector Development and the Millennium Development Goals. [Google Scholar]
- 61.Himmelstein D.U., Woolhandler S. Public health's falling share of US health spending. Am. J. Publ. Health. 2015;106(1):56–57. doi: 10.2105/AJPH.2015.302908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nguyen T.T., Pham T.A.T., Tram H.T.X. Role of information and communication technologies and innovation in driving carbon emissions and economic growth in selected G-20 countries. J. Environ. Manag. 2020;261 doi: 10.1016/j.jenvman.2020.110162. [DOI] [PubMed] [Google Scholar]
- 63.Xiaoman W., Majeed A., Vasbieva D.G., Yameogo C.E.W., Hussain N. Natural resources abundance, economic globalization, and carbon emissions: advancing sustainable development agenda. Sustain. Dev. 2021;29(5):1037–1048. [Google Scholar]
- 64.Jin H., Qian X. International Journal of Environmental Research and Public Health; 2020. How the Chinese Government Has Done with Public Health from the Perspective of the Evaluation and Comparison about Public-Health Expenditure. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shen L., Ren Y., Xiong N., Li H., Chen Y. Why small towns can not share the benefits of urbanization in China? J. Clean. Prod. 2018;174:728–738. [Google Scholar]
- 66.Roodman D. How to do Xtabond2: an introduction to difference and system GMM in stata. STATA J. 2009;9(1):86–136. [Google Scholar]
- 67.Baltagi B.H., Lagravinese R., Moscone F., Tosetti E. Health care expenditure and income: a global perspective. Health Econ. 2017;26(7):863–874. doi: 10.1002/hec.3424. [DOI] [PubMed] [Google Scholar]
- 68.Jaunky V.C., Khadaroo A.J. 2006. Health Care Expenditure and GDP: an African Perspective, iHEA 2007 6th World Congress: Explorations in Health Economics Paper. [Google Scholar]
- 69.Xu Q., Zhong M. The impact of income inequity on energy consumption: the moderating role of digitalization. J. Environ. Manag. 2023;325 doi: 10.1016/j.jenvman.2022.116464. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.