Abstract
Background
The emergence of severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) has resulted in an unprecedented global pandemic. Most infected patients are either asymptomatic or have mild upper respiratory infection symptoms. However, life‐threatening sequelae have been observed. In this report, we reviewed nine cases of patients with severe complications from sinonasal disease in the setting of acute SARS‐CoV‐2 infection.
Methods
IRB approval was obtained prior to study initiation. A retrospective chart review was performed of patients admitted to a tertiary hospital with complex sinonasal symptoms that required otolaryngologic evaluation and management in the setting of concomitant SARS‐CoV‐2 infection.
Results
Nine patients, ranging from ages 3 to 71 years, with sinonasal disease and simultaneous SARS‐CoV‐2 infection were identified. Initial presentations ranged from asymptomatic infection to mild/moderate disease (nasal obstruction, cough) or more severe sequelae including epistaxis, proptosis, or neurologic changes. SARS‐CoV‐2 tests were positive from one to 12 days after symptom onset, with three patients receiving SARS‐CoV‐2‐directed treatment. Complex disease presentations included bilateral orbital abscesses, suppurative intracranial infection, cavernous sinus thrombosis with epidural abscess, systemic hematogenous spread with abscess development in four distinct anatomic locations, and hemorrhagic benign adenoidal tissue. Eight of nine patients (88.8%) required operative intervention. Patients with abscesses also required prolonged, culture‐directed antibiotic courses.
Conclusion
Though most SARS‐CoV‐2 infections are asymptomatic and/or self‐limited, there is significant morbidity and mortality in patients with severe disease sequela as outlined in our reported cases. This suggests early identification and treatment of sinonasal disease in this patient population is critical to minimizing poor outcomes. Further research on the pathophysiology of these atypical presentations is needed.
Level of Evidence
4 (Case Series).
Keywords: COVID, functional endoscopic sinus surgery, SARS‐CoV‐2, sinusitis
The emergence of severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) has resulted in an unprecedented global pandemic. Most infected patients are either asymptomatic or have mild upper respiratory infection symptoms. However, life‐threatening sequelae have been observed. In this report, we reviewed nine cases of patients with severe complications from sinonasal disease in the setting of acute SARS‐CoV‐2 infection.
1. INTRODUCTION
The emergence of severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) has resulted in an unprecedented global pandemic. The majority of patients are either asymptomatic or have mild upper respiratory infection symptoms. 1 , 2 However, some cases are complicated by progression to acute respiratory distress syndrome and higher mortality rates. 1 , 3 , 4 It is thought that pathophysiology of severe pulmonary disease is caused by a cytokine storm and a pro‐inflammatory state. 5 , 6 Through this very mechanism, severe systemic inflammatory sequela beyond the expected pulmonary system has been described, with life‐threatening multi‐organ dysfunction. 1 , 3 , 4 In the otolaryngologic literature, there are isolated reports of atypical, severe presentations in context of SARS‐CoV‐2 infection, however, there are no larger comprehensive series. 7 , 8 , 9 , 10 , 11 , 12 , 13 We present our single center series of nine cases of patients with severe complications from sinonasal disease in the setting of acute SARS‐CoV‐2 infection. Institutional Review Board approval at the University of North Carolina was obtained prior to completing the study.
2. CLINICAL CASES
2.1. Case 1
A 48‐year‐old male with diabetes mellitus type 2, unvaccinated against SARS‐CoV‐2, presented to the emergency department (ED) with 8 days of intermittent epistaxis. He was treated conservatively with anterior nasal pressure and oxymetazoline but required eventual thrombin matrix application as well as nasal packing. Workup showed normal platelets, prothrombin time (PT)/international normalized ratio (INR), partial thromboplastin time (PTT). He continued to have ongoing bleeding around the nasal pack. Computed tomographic imaging (CT) of the sinuses was obtained, which showed a maxillary polyp (Figure 1). He was subsequently taken to the operating room for definitive management. Intraoperatively, a large 2 cm nasopharyngeal mass was noted to be friable and bleeding. This was biopsied, then the bleeding was controlled with electrocautery. Postoperatively he was discharged to home, without any subsequent issues. Surgical pathology returned as benign sinonasal lymphoid adenoidal tissue. After 6 weeks, he was taken back to the operating room for a second look and repeat biopsy, which resulted again as benign sinonasal lymphoid adenoidal tissue.
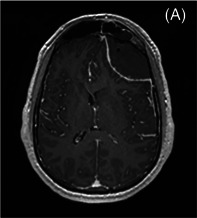
FIGURE 1.
Coronal computed tomography (CT) showing right maxillary polyp
2.2. Case 2
A 25‐year‐old male with no significant past medical history who is unvaccinated to SARS‐CoV‐2 presented to the ED with two weeks of sinus congestion and intermittent fever, with worsening symptoms and malaise over the penultimate few days. Diagnostic workup was notable for CT that showed left frontal sinus opacification and a 7 × 3 cm left frontal epidural fluid collection (Figure 2). Other notable labs were an elevated PT/INR to 15.7/1.35, with normal PTT and platelet count. He was started on vancomycin and ceftriaxone, then was taken to the operating room for a left frontal craniotomy. Intraoperatively, the fluid collection was noted to be largely hematoma, so no functional endoscopic sinus surgery (FESS) was pursued; however, intraoperative culture was sent. Postoperatively, he was treated with 3 days of Remdesivir and 2 days of systemic steroids for ongoing SARS‐CoV‐2. Intraoperative culture grew Streptococcus pneumoniae, leading to subsequent antibiotics coverage narrowed to ceftriaxone for a 6‐week total course. At time of discharge, he was at his neurologic baseline without any appreciable deficit.
FIGURE 2.
Axial (A) and coronal (B) T2 weighted magnetic resonance imaging (MRI) showing left frontal epidural hematoma. (C) Coronal computed tomography (CT) showing left frontal sinus opacification
2.3. Case 3
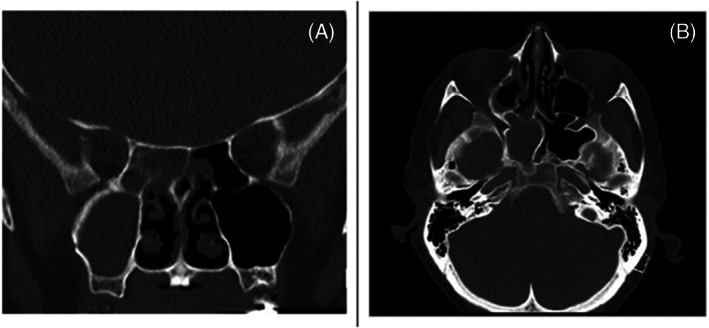
An 11‐year‐old male with history of attention deficit hyperactivity disorder and fully vaccinated to SARS‐CoV‐2 presented to the ED with 3 days of right periorbital edema, proptosis, and ophthalmoplegia. Visual acuity was intact to light perception and finger count. Sinus endoscopy with copious purulence noted in the right middle meatus and sphenoethmoidal recess. Laboratory workup notable for SARS‐CoV‐2 positive PCR test. Diagnostic workup included a CT of the sinuses and head, which showed a right orbital subperiosteal abscess measuring 1.9 × 3.3 × 2.5 cm with dehiscence of the right lateral ethmoid sinus in the setting of significant sinonasal inflammation with opacification of the right frontal, maxillary, ethmoid, and sphenoid sinus opacification (Figure 3). Broad spectrum antibiotics of vancomycin, cefepime, and metronidazole were initiated. He was taken to the operating room on hospital day 0 for a right FESS and orbital decompression. Intraoperative cultures grew methicillin‐susceptible Staphylococcus aureus (MSSA) and Streptococcus anginosus. On hospital day 4, antibiotics were narrowed to cefazolin, then subsequently to cephalexin on hospital day 6 for 3‐week total course of antibiotics. At discharge, the ophthalmoplegia was resolved, visual acuity was 20/20 bilaterally, and proptosis was resolving.
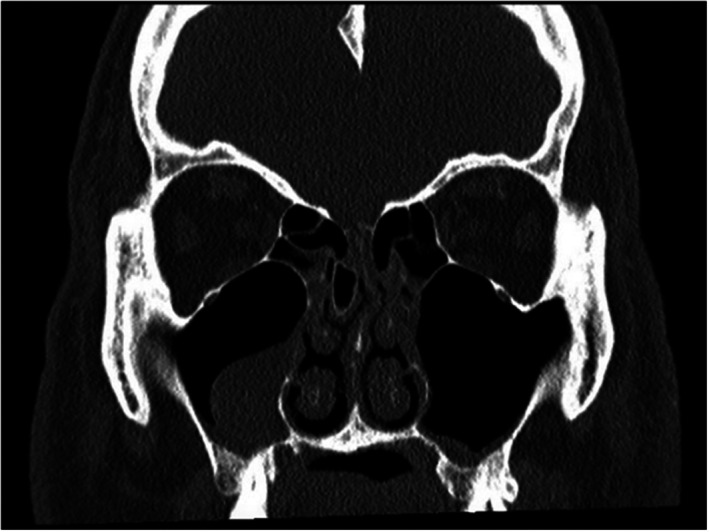
FIGURE 3.
Coronal (A) and axial (B) computed tomography (CT) showing left paranasal sinus disease and left subperiosteal abscess
2.4. Case 4
A 3‐year‐old male with no significant past medical history, unvaccinated to SARS‐CoV‐2, presented to an outside hospital with 12 days of intermittent fever and yellow nasal discharge, and a week of intermittent eye swelling. There, a CT was obtained, which showed bilateral sinus inflammation (bilateral maxillary, anterior ethmoids, right posterior ethmoid, and right sphenoid, without pneumatization of the frontal sinuses) with bilateral orbital abscesses with intracranial extension from the right frontal lobe. Ophthalmology performed an incision and drainage (I&D) of the orbital abscess, then transferred to our tertiary care center for increased level of care given the intracranial involvement. On arrival, he was started on broad‐spectrum antibiotics of vancomycin, ceftriaxone, and metronidazole. A magnetic resonance imaging (MRI) of the head was obtained, which showed a 2.5 × 1.0 × 2.1 cm right frontal abscess connecting to right orbital 4.3 × 2.7 × 1.6 cm abscess through the right superior orbital wall (Figure 4), as well as abscess of the left orbit 1.9 × 1.6 × 0.8 cm with small extension along the anterior left parafalcine and frontal subdural space. He was taken to the operating room by ophthalmology, neurosurgery, and otolaryngology services on hospital day 0 for a bilateral FESS with bilateral orbital decompression, ophthalmology performed anterior drainage of orbital abscesses, and neurosurgery performed frontal burr hole for evacuation of subdural empyema. Intraoperative cultures were obtained; the orbital culture grew Eikenella, and the subdural culture grew GPCs. On hospital day 9, he developed new onset focal right parietal seizures and hyperkinetic choreoathetotic movements of left foot. He was taken to the operating room for a craniotomy and sinus debridement. On hospital day 11, the antibiotics were narrowed to ceftriaxone and metronidazole, for a 6‐week total antibiotic course. At discharge, dilated eye exam showed a normal fundus exam, symmetric pupils, intact extraocular movements. Seizure activity was resolved; however, he had persistent left lower extremity weakness albeit with continuing improvement.
FIGURE 4.
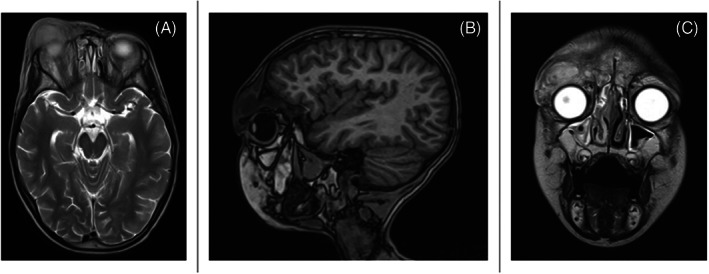
T2 weight magnetic resonance imaging (MRI) axial (A), sagittal (B), and coronal (C) views showing right frontal abscess communicating with right orbital abscess communicating through superior orbital wall
2.5. Case 5
A 15‐year‐old male with history of asthma and unvaccinated to SARS‐CoV‐2 presented to an outside hospital acute with 1 day of altered mental status, dysarthria, exophthalmos, right upper extremity, and bilateral lower extremity weakness. He presented 5 days after developing nasal congestion and intermittent headaches, with a positive test for SARS‐CoV‐2. Diagnostic evaluation of CT Head and MRI Brain were obtained, which were notable for pan‐sinus inflammation, with anterior table disruption in the left frontal sinus that extended to a 13.1 cm left frontoparietal to left occipital subdural empyema, as well as several other fluid collections in the right frontal and left frontoparietal scalp (Figure 5). He was subsequently transferred to our tertiary care center for an increased level of care. Vancomycin and meropenem were started on arrival. He was then taken to the operating room on hospital day 0 for an FESS, I&D of scalp abscess, and neurosurgery performed burr hole craniotomy. Intraoperative cultures grew MSSA, Staphylococcus lugdunensis, and Cutibacterium from the sinuses; and Fusobacterium necrophorum and coagulase negative Staphylococcus from the intracranial specimen. Blood cultures grew F. necrophorum. Interval imaging on hospital day 2 showed a residual 1.2 cm subdural empyema and multiple scalp abscesses, so he was taken back to the operating room with neurosurgery and otolaryngology for repeat sinus washout and drainage of residual abscesses. Hospital day 5 interval imaging showed increased subdural empyema to 1.4 cm and the development of a new frontal epidural empyema measuring 0.9 cm, so the patient was taken back to the operating room by neurosurgery for a left craniectomy. Hospital day 7 interval imaging showed residual subdural empyema, scalp abscesses, right periorbital fluid collection, and venous thrombosis of the superior sagittal sinus, so was taken to the operating room with neurosurgery for a repeat intracranial washout. He was started on a therapeutic heparin for the superior sagittal sinus thrombosis. Ophthalmology performed a bedside I&D of the right periorbital collection, with repeat washout on hospital days 8 and 10. The correlating orbital culture was negative. Interval imaging on hospital day 15 showed a redeveloping 4.1 cm occipital empyema, 1.4 cm parafalcine empyema, several scalp abscesses, and improvement of the superior sagittal sinus thrombosis. He was taken to the operating room with neurosurgery for a repeat left craniotomy, left occipital burr hole for occipital subdural empyema evacuation. Hospital day 18, he developed right wrist pain with corresponding multifocal osteomyelitis and fluid collections, septic arthritis of the right wrist on imaging, for which he was taken to the operating room with Orthopedic Surgery for I&D. The corresponding culture was negative. On hospital day 22, he developed right hip pain, which was showed to be a right hip abductor abscess, which was drained by Vascular‐Interventional Radiology. Subsequent interval imaging showed continued improvement of the abscesses, and no further surgical intervention was required. Antibiotics were transitioned to cefepime and metronidazole for a 6‐week total course. At discharge, he had residual right hemiparesis, albeit with improving strength and muscle activation.
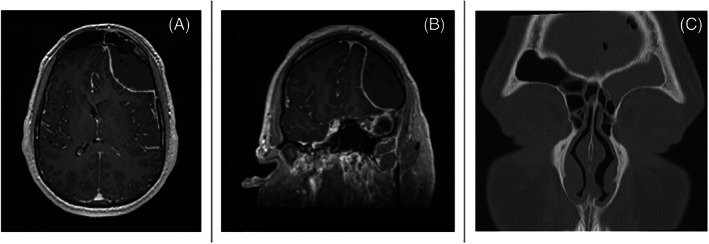
FIGURE 5.
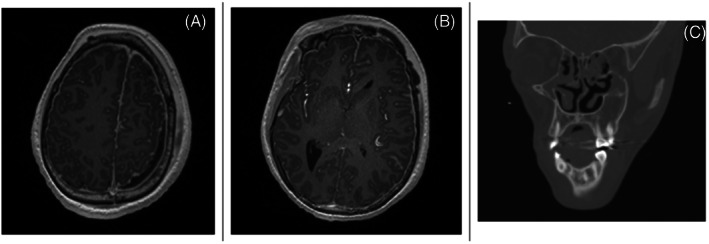
T2 weighted magnetic resonance imaging (MRI) showing left occipital subdural empyema (A) that extends from Pott's puffy tumor with disruption in the left frontal sinus that extends to a 13.1 cm left frontoparietal subdural empyema (B). (C) computed tomography (CT) showing correlating diffuse paranasal opacification
2.6. Case 6
A 4‐year‐old female without any significant past medical history, unvaccinated to SARS‐CoV‐2, presented to an outside hospital with new onset complex febrile seizure in the setting of 3 days of rhinorrhea, congestion, fatigue, and cough. A positive SARS‐CoV‐2 test was obtained. Diagnostic workup was notable CT Head that showed pan‐sinonasal mucosal edema. She was started on Remdesivir for 3 days, systemic steroids for 3 days and, and IVIG. On outside hospital day 4, she developed another seizure, with subsequent prolonged somnolence and confusion. Repeat CT Sinus and Head showed pan‐sinus opacification as well as a 1.1 cm right holohemispheric subdural empyema causing a 1 cm of leftward midline shift. She was transferred to our tertiary care center for an increased level of care (Figure 6). On arrival, she was started on vancomycin, ceftriaxone, and metronidazole. She was taken to the operating room for an FESS and neurosurgery performed right burr hole craniotomy. Intraoperative cultures grew skin flora from the sinuses and Streptococcus anginosus from the intracranial specimen. Blood culture grew Streptococcus intermedius. On hospital day 3, she developed greater somnolence in setting of increased leukocytosis, so was taken to the operating room with neurosurgery for a repeat craniotomy. She clinically improved, however, interval imaging on hospital day 10 revealed increasing 1.1 cm bilateral empyema along the anterior hemispheric fissure. She was taken to the operating room with neurosurgery and otolaryngology for repeat craniotomy and sinonasal debridement and washout. She improved clinically and interval imaging showed continued improvement of the empyema. Culture driven antibiotics were narrowed to ceftriaxone and metronidazole for a 6‐week total course. At discharge, she was neurologically intact with improving strength and mobility.
FIGURE 6.
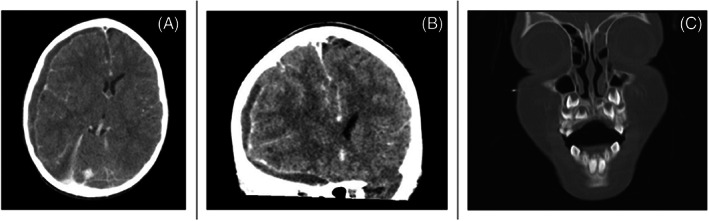
Axial (A) and coronal (B) computed tomography (CT) showing right holohemispheric subdural empyema causing leftward midline shift. (C) Coronal CT of left frontal sinus opacification that correlates the right subdural empyema
2.7. Case 7
A 28‐year‐old female with history of hepatitis C and intravenous drug use, who was 39 weeks pregnant and unvaccinated for SARS‐CoV‐2 presented to an outside hospital with altered mental, bilateral proptosis, and ophthalmoplegia in the setting of positive SARS‐CoV‐2 test 10 days prior. Diagnostic workup was notable for CT venography Head with a mild left frontal and anterior sinus opacification, 3.7 × 1.0 × 4.8 cm left frontotemporoparietal abscess (Figure 7) and filling defects of the left transverse and left cavernous venous sinuses, as well as bilateral internal jugular veins. She was transferred to our tertiary care center for increased level of care. On arrival, she was started on vancomycin, cefepime, and metronidazole. She was taken to the operating room with neurosurgery and obstetrics for left burr hole craniotomy and cesarean section. She was started on a heparin drip postoperatively for cavernous sinus and internal jugular thrombi. Intraoperative intracranial culture grew Methicillin‐resistant Staphylococcus aureus, with antibiotics narrowed to vancomycin for a 6‐week total course. Interval imaging on hospital day 3 showed worsening of sinus opacification, with increase to pan‐sinus involvement, so otolaryngology was consulted. Patient was deemed unstable for FESS given inability to hold heparin drip with high risk for postoperative bleeding, and was treated medically with ongoing antibiotics, fluticasone spray, and sinonasal irrigation. Once the patient was extubated, she was noted to have bilateral retinal artery occlusion with residual vision only to light and subjective left ear hearing loss. She required no further surgical intervention, as was discharged to home with prolonged anticoagulation and planned multidisciplinary follow‐up.
FIGURE 7.
Computed tomography (CT) coronal (A) and axial (B) showing left frontoparietal abscess
2.8. Case 8
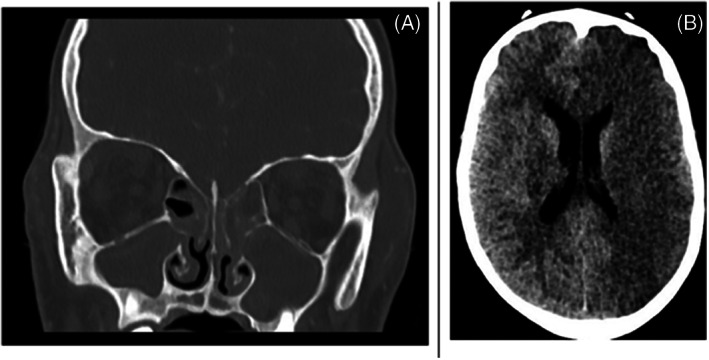
A 71‐year‐old female with history of paroxysmal atrial fibrillation, chronic sinusitis, and history of urinary tract infection presented with bilateral acute on chronic sinusitis and hypotension from an OSH. She had initially presented to the OSH with generalized weakness and a ground‐level fall. She had tested positive for SARS‐CoV‐2 prior to transfer though previously vaccinated to SARS‐CoV‐2. Notably on physical evaluation, she was noted to have left‐sided cranial nerves 3, 4, and 6 palsies. CT demonstrated significant right‐sided acute on chronic sinusitis (Figure 8). An MRA and MRV Brain were completed, which demonstrated bilateral cavernous sinus thrombosis with suspected thrombosis of the left superior ophthalmic vein, right sigmoid sinus, and right jugular bulb. Repeat MRV in 2 days' time was found to be stable and anticoagulation was continued until surgery. She underwent bilateral sphenoidotomies and a right sided FESS. Intraoperative findings included chronic pansinusitis with purulence in the maxillary, ethmoid, sphenoid, and frontal cavities on the right as well as a right‐sided sphenoidal fungal ball. Sinus cultures grew mixed anaerobes and aerobes. Prior blood cultures demonstrated klebsiella oxytoca. Heparin was restarted 24 h postoperatively. Her clinical status improved following treatment with broad‐spectrum antibiotics and anticoagulation.
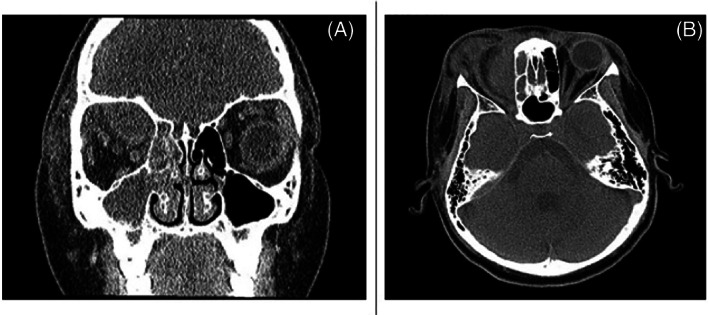
FIGURE 8.
Computed tomography (CT) coronal views (A) and axial views (B) demonstrating significant right‐sided acute on chronic sinusitis
2.9. Case 9
A 13‐year‐old male with a history of congenital aortic stenosis s/p balloon valvuloplasty at 1 month of age presented from OSH with a 2‐week history of acute onset headache, emesis, periorbital swelling, altered mental status and right upper extremity weakness in the setting of SARS‐CoV‐2, unvaccinated. The patient quickly developed acute respiratory failure, pressor‐dependent septic shock, and coagulopathy. Imaging was significant for diffuse intracranial findings, notably pontine and frontal lobe ischemia, and bilateral cavernous sinus and superior ophthalmic vein thrombosis in the setting of bilateral pansinusitis with frontal soft tissue edema (Figure 9A). TPA was administered and the patient received acute SARS‐CoV‐2 therapy with Remdesivir. He underwent a bilateral FESS with orbital decompression. Heparin drip was restarted after surgery and continued during the patient's hospital course. Intraoperative cultures grew Streptococcus anginosus. A multidisciplinary team approach was taken to care for the patient including Neurosurgery, Neurology, Pediatric Intensive Care, Infectious Disease, Ophthalmology, and Radiology. Although he was treated with broad‐spectrum antibiotics and anticoagulation, he developed progressive arterial embolic infarctions, notably new onset acute arterial infarctions of both the left ACA and left MCA territories (Figure 9B) in the setting of declining neurological function and succumbed to disease.
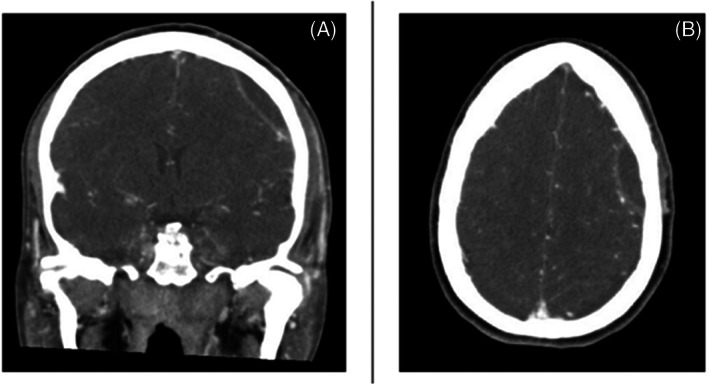
FIGURE 9.
Computed tomography (CT) coronal (A) demonstrating pansinusitis at the time of admission and CTA (B) showing significant left frontoparietal hypoattenuation in the setting of left MCA stroke
3. DISCUSSION
This series of nine cases illustrates severe and unusual sinonasal manifestations in the setting of concurrent SARS‐CoV‐2 infection. Case 1 describes a middle‐aged male with no bleeding history who presented with severe epistaxis recalcitrant to conservative management. SARS‐CoV‐2 has been described to have a wide spectrum of coagulopathy and bleeding risk. 14 , 15 , 16 , 17 , 18 , 19 An overall thrombotic complication of 9.5% and overall bleeding rate of 4.8%. 14 Critical bleeding complications are correlated to elevated D‐dimer or thrombocytopenia, often in the setting of normal PT/INR and PTT. 14 Hemorrhagic benign adenoid tissue is an uncommon presentation especially in an adult with no other known bleeding history, with only one pediatric case report noted in the literature. 20 Repeat biopsies of the tissue were obtained due to the abnormal presentation, which returned as benign adenoidal tissue, making bleeding due to pathologic change unlikely, especially as there was no recurrence once beyond the active SARS‐CoV‐2 infection. Case 2 describes the development of a frontal epidural hematoma with infiltrating sinus bacteria in the setting of an acute SARS‐CoV‐2 infection. This patient presented with an elevated PTT likely contributing to the intracranial bleed. Interestingly, an intraoperative culture was taken of the hematoma, which grew strep pneumoniae possibly stemming from the radiologically correlating frontal sinus disease.
Acute bacterial sinusitis often presents as a superinfection of an upper respiratory viral infection. 21 , 22 Most cases of acute rhinosinusitis present as cough, nasal discharge, facial pain, and pressure; and are often uncomplicated due to antibiotic efficacy. 21 However, spread of infection beyond the paranasal sinuses can lead to severe sequelae such as orbital, intracranial, and cavernous sinus thrombosis. 23 , 24 , 25 There have been isolated reports of these sinonasal complications in the setting of SARS‐CoV‐2 described in the medical literature. 8 , 10 , 11 , 13
The nasal cavity and nasopharynx are known reservoirs of SARS‐CoV‐2 viral load and replication. With this high viral activity, the virus is hypothesized to cascade a cytokine driven inflammatory response, which exacerbates endothelial damage and potentiates these severe sinonasal complications. 12 , 16 , 17 Cases 3–9 describe patients who developed these complications in the setting of active SARS‐CoV‐2 infection. These cases ranged from a singular periosteal abscess to multifocal thromboses and systemic seeding of abscesses. Cases 1–8 were eventually discharged from the hospital on broad‐spectrum antibiotic therapy and were stable at subsequent follow‐up visits (Table 1).
TABLE 1.
Summary of patient cases assessing vaccination status prior to admission, antibiotics at discharge, as well as 45‐day posthospitalization status at subsequent follow‐up visit(s)
| Case | Vaccination status preadmission | Antibiotics at discharge | 90‐Day readmission? | 45‐day morbidity/morality following discharge |
|---|---|---|---|---|
| 1 (48 yo M) | Unvaccinated | Doxycycline (2‐week course) | None | Stable with no concerns, no additional antibiotics needed |
| 2 (25 yo M) | Unvaccinated | Ceftriaxone (6‐week course) | None | Stable with no concerns, no additional antibiotics needed |
| 3 (11 yo M) | Vaccinated | Cephalexin (3‐week course) | None | Stable with no concerns, no additional antibiotics needed |
| 4 (3 yo M) | Unvaccinated | Ceftriaxone/Metronidazole (6‐week course) | None | Stable with no concerns, no additional antibiotics needed |
| 5 (15 yo M) | Unvaccinated | Cefepime/Metronidazole (6‐week course) | None | Stable with no concerns, no additional antibiotics needed |
| 6 (4 yo F) | Unvaccinated | Ceftriaxone/Metronidazole (6‐week course) | None | Stable with no concerns, no additional antibiotics needed |
| 7 (28 yo F) | Unvaccinated | None | None | Stable with no concerns, no additional antibiotics needed |
| 8 (71 yo F) | Vaccinated | Ceftriaxone (6‐week course) | None | Stable with no concerns, no additional antibiotics needed |
| 9 (13 yo M) | Unvaccinated | ‐ | ‐ | Deceased during hospitalization |
Though it is unclear if SARS‐CoV‐2 is truly contributory or just incidental to the presentations outlined in the cases, the concurrent nature of infection with these atypical and severe presentation is interesting. With concurrent sinus disease in many of these patients, active SARS‐CoV‐2 could potentially inhibit normal mucociliary clearance, leading to these complex manifestations. SARS‐CoV‐2 may be the underlying viral infection for bacterial superinfection or as a severe systemic inflammatory response facilitating easier hematologic spread and seeding of sinonasal bacteria. 26
4. CONCLUSION
To our knowledge, this case series is the most extensive single‐center review of SARS‐CoV‐2 sinonasal sequelae. Although the SARS‐CoV‐2 pandemic has been going on for several years, there is still much to be researched and investigated about the disease process. The inflammatory milieu of the virus has illustrated a wide presentation spectrum that continues to be ever expanded. Though most SARS‐CoV‐2 infections are asymptomatic or self‐limited, there is significantly high morbidity and mortality to the severe disease sequelae, so early identification and treatment is critical.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Lee SE, Ghodke AN, Stepp WH, et al. Sinonasal complications of severe acute respiratory syndrome coronavirus‐2: A single center case series. Laryngoscope Investigative Otolaryngology. 2023;8(1):16‐24. doi: 10.1002/lio2.1006
REFERENCES
- 1. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the new York City area. JAMA‐J Am Med Assoc. 2020;323(20):2052‐2059. doi: 10.1001/jama.2020.6775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID‐2019. Nature. 2020;581(7809):465‐469. doi: 10.1038/s41586-020-2196-x [DOI] [PubMed] [Google Scholar]
- 3. Shen C, Wang Z, Zhao F, et al. Treatment of 5 critically ill patients with COVID‐19 with convalescent plasma. JAMA‐J Am Med Assoc. 2020;323(16):1582‐1589. doi: 10.1001/jama.2020.4783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid‐19. N Engl J Med. 2020;383(2):120‐128. doi: 10.1056/nejmoa2015432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the “Cytokine Storm” in COVID‐19. J Infect. 2020;80(6):607‐613. doi: 10.1016/j.jinf.2020.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID‐19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033‐1034. doi: 10.1016/S0140-6736(20)30628-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leboulanger N, Sagardoy T, Akkari M, et al. COVID‐19 and ENT pediatric otolaryngology during the COVID‐19 pandemic. Guidelines of the French Association of Pediatric Otorhinolaryngology (AFOP) and French Society of Otorhinolaryngology (SFORL). Eur Ann Otorhinolaryngol Head Neck Dis. 2020;137(3):3‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Balasa D, Tunas A, Stan AV. Odontogen frontoparial epidural and subdural empyema complicated with frontal intracerebral abscess and Covid. ROM Neurosurg. 2021;35:20‐24. doi: 10.33962/roneuro-2021-003 [DOI] [Google Scholar]
- 9. Blanco CH, Stein JB, Barinsky GL, et al. Management of complicated pediatric rhinosinusitis in the COVID‐19 era. Am J Otolaryngol‐Head Neck Med Surg. 2020;41(6):102746. doi: 10.1016/j.amjoto.2020.102746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shahab A, Arora A, Chhina SS, Dhillon S, Nazir U. A unique triad of invasive sinusitis, brain abscess with focal cerebritis, and COVID‐19. Am J Case Rep. 2021;22(1):e933177. doi: 10.12659/AJCR.933177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Turbin RE, Wawrzusin PJ, Sakla NM, et al. Orbital cellulitis, sinusitis and intracranial abnormalities in two adolescents with COVID‐19. Orbit (London). 2020;39(4):305‐310. doi: 10.1080/01676830.2020.1768560 [DOI] [PubMed] [Google Scholar]
- 12. Arteaga AA, Tran J, Frey H, Lewis AF. Rapidly progressive complicated acute bacterial sinusitis in the setting of severe pediatric SARS‐CoV‐2 infection. Ann Otol Rhinol Laryngol. 2021;131:1158‐1163. doi: 10.1177/00034894211055337 [DOI] [PubMed] [Google Scholar]
- 13. Shires CB, Klug T, Dryden S, Ford J. Unusual cause of acute sinusitis and orbital abscess in COVID‐19 positive patient: case report. Int J Surg Case Rep. 2021;79:79‐168. doi: 10.1016/j.ijscr.2021.01.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Al‐Samkari H, Karp Leaf RS, Dzik WH, et al. COVID‐19 and coagulation: bleeding and thrombotic manifestations of SARS‐CoV‐2 infection. Blood. 2020;136(4):489‐500. doi: 10.1182/BLOOD.2020006520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nadkarni GN, Lala A, Bagiella E, et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID‐19. J Am Coll Cardiol. 2020;76(16):1815‐1826. doi: 10.1016/j.jacc.2020.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Merrill JT, Erkan D, Winakur J, James JA. Emerging evidence of a COVID‐19 thrombotic syndrome has treatment implications. Nat Rev Rheumatol. 2020;16(10):581‐589. doi: 10.1038/s41584-020-0474-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Iba T, Levy JH, Levi M, Thachil J. Coagulopathy in COVID‐19. J Thromb Haemost. 2020;18(9):2103‐2109. doi: 10.1111/jth.14975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Connors JM, Levy JH. COVID‐19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033‐2040. doi: 10.1182/BLOOD.2020006000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jiménez D, García‐Sanchez A, Rali P, et al. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: a systematic review and meta‐analysis. Chest. 2021;159(3):1182‐1196. doi: 10.1016/j.chest.2020.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Almomen AH, Alzaid JA. Spontaneous adenoid bleeding presenting as epistaxis and hematemesis. MOJ Clin Med Case Rep. 2018;8(1):1‐2. doi: 10.15406/mojcr.2018.08.00234 [DOI] [Google Scholar]
- 21. Orlandi RR, Kingdom TT, Smith TL, et al. International consensus statement on allergy and rhinology: rhinosinusitis 2021. Int Forum Allergy Rhinol. 2021;11(3):213‐739. doi: 10.1002/alr.22741 [DOI] [PubMed] [Google Scholar]
- 22. Fokkens WJ, Lund VJ, Hopkins C, et al. Epos 2020. Off J Eur Int Rhinol Soc Confed Eur ORL‐HNS. 2020;(Suppl 29):62. [Google Scholar]
- 23. Chandler JR, Langenerunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80(9):1414‐1428. doi: 10.1288/00005537-197009000-00007 [DOI] [PubMed] [Google Scholar]
- 24. Gallagher RM, Gross CW, Phillips CD. Suppurative intracranial complications of sinusitis. Laryngoscope. 1998;108:11‐1642. doi: 10.1097/00005537-199811000-00009 [DOI] [PubMed] [Google Scholar]
- 25. Dayman GL, Adams GL, Paugh DR, Koopmann CF. Intracranial complications of paranasal sinusitis a combined institutional review. Laryngoscope. 1991;101(3):234‐239. doi: 10.1288/00005537-199103000-00003 [DOI] [PubMed] [Google Scholar]
- 26. Robinot R, Hubert M, de Melo GD, et al. SARS‐CoV‐2 infection induces the dedifferentiation of multiciliated cells and impairs mucociliary clearance. Nat Commun. 2021;12(1):4354. doi: 10.1038/s41467021-24521-x [DOI] [PMC free article] [PubMed] [Google Scholar]


