Abstract
Background
Social relationships are associated with mortality and chronic conditions. However, little is known about the effects of social relationship satisfaction on multiple chronic conditions (multimorbidity).
Aims
To examine whether social relationship satisfaction is associated with the accumulation of multimorbidity.
Methods
Data from 7 694 Australian women who were free from 11 chronic conditions at 45–50 years of age in 1996 were analysed. Five types of social relationship satisfaction (partner, family members, friends, work and social activities) were measured approximately every 3 years and scored from 0 (very dissatisfied) to 3 (very satisfied). Scores from each relationship type were summed to provide an overall satisfaction score (range: ≤5–15). The outcome of interest was the accumulation of multimorbidity in 11 chronic conditions.
Results
Over a 20-year period, 4 484 (58.3%) women reported multimorbidities. Overall, the level of social relationship satisfaction had a dose–response relationship with the accumulation of multimorbidities. Compared with women reporting the highest satisfaction (score 15), women with the lowest satisfaction (score ≤5) had the highest odds of accumulating multimorbidity (odds ratio (OR)= 2.35, 95% confidence interval (CI): 1.94 to 2.83) in the adjusted model. Similar results were observed for each social relationship type. Other risk factors, such as socioeconomic, behavioural and menopausal status, together explained 22.72% of the association.
Conclusions
Social relationship satisfaction is associated with the accumulation of multimorbidity, and the relationship is only partly explained by socioeconomic, behavioural and reproductive factors. Social connections (eg, satisfaction with social relationships) should be considered a public health priority in chronic disease prevention and intervention.
Keywords: social networking, social isolation, ageism, psychosomatic medicine
WHAT IS ALREADY KNOWN ON THIS TOPIC
The associations between structural (eg, social network size and marital status) or functional (eg, received and perceived social support and loneliness) components of social relationships and morbidity and mortality have been estimated in many studies and populations, but the role of social relationship satisfaction is largely unknown.
Multiple chronic conditions (multimorbidity) are the norm in clinical practice, but little is known about the role of social relationships in this process.
WHAT THIS STUDY ADDS
We demonstrated a dose–response relationship between social relationship satisfaction and the accumulation of multimorbidity in women from midlife to early old age, which was only partly explained by sociodemographic, health behavioural and reproductive factors.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Social connections should be integrated into the prevention and intervention of chronic diseases and multimorbidity.
Introduction
Chronic diseases are the leading cause of the global disease burden.1 With the ageing of the population, the number of people, particularly women, living with multiple chronic conditions (multimorbidity) has continually increased.2 Tackling multimorbidity is a key challenge faced by healthcare systems and services traditionally designed around a single condition.3 Current approaches for the management and prevention of multimorbidity have been people-centred, involving integrated health services, which emphasise treating individuals as whole persons.2 4 Emerging evidence shows that the nature and impact of the social relationship with which people live and how it shapes the development of chronic conditions should be considered in these approaches.5–9
Social relationships have been associated with many individual mental and somatic chronic conditions (eg, depression, hypertension, cardiovascular disease and cancer), as well as all-cause and cause-specific mortality.10–12 For example, a meta-analytical review across 148 studies indicated that individuals with adequate social relationships have a 50% greater likelihood of survival than those with poor or insufficient social relationships.10 Another meta-analysis showed that loneliness and social isolation were associated with a 30% increase in the risk of cardiovascular disease.11 A longitudinal study in Korea found that loneliness, social disengagement and group-level segregation were all associated with all-cause mortality.12 Despite these findings, there is little evidence on the association between social relationships and multimorbidity.13 We are only aware of cross-sectional studies investigating the link of physical multimorbidity with social participation and loneliness.13 14 However, no study has directly shed light on the association between social relationships and multimorbidity, particularly the accumulation of multimorbidity (the transition from a healthy state or only one condition to multimorbidity).
Social relationships have been defined diversely, with three broad categorisations that assess different aspects: structural, functional and qualitative.6 The associations between the structural (eg, social network size and marital status) and functional (eg, received and perceived social support and loneliness) aspects of social relationships and cognitive performance, morbidity and mortality have been estimated in many studies and populations6 7 15; however, the role of qualitative indicators (eg, subjective rating of satisfaction or quality) is largely unknown. Furthermore, most previous studies have examined only individual types of social relationship satisfaction or quality (eg, satisfaction with the partner, family members, friends, work and social activities),16–21 not considering the relative importance and combined effects of these types in relation to the development of individual chronic conditions and accumulation of multimorbidity. To examine the relative importance of each social relationship type, it is important to compare the associations between individual relationship types and the development of multimorbidity using the same analytical model.22
Social relationships change over time. Previous studies have typically assessed these relationships at only one time point, assuming that they remain constant over time.23 Little attention has been paid to the satisfaction with social relationships measured at multiple time points and accounted for as a time-varying variable in relation to the development of individual chronic conditions and multimorbidity.24 In addition, previous evidence suggests that the magnitude of the influence of social relationships on the risk of mortality is comparable with well-established risk factors (eg, obesity and alcohol intake).6 10 However, much remains to be learnt about the extent to which social relationship satisfaction contributes to multimorbidity.
To address these important gaps in the literature, we used longitudinal data spanning two decades to investigate whether satisfaction levels of a single social relationship type and the combined effect of multiple types are associated with the accumulation of multimorbidity in a national cohort of Australian women from midlife to early old age. We also quantified the potential contribution of other risk factors (socioeconomic status, health behaviours and menopausal status) to the association.
Methods
Study design and participants
The Australian Longitudinal Study on Women’s Health (ALSWH) is an ongoing population-based prospective cohort study that aims to examine factors associated with the health and well-being of three cohorts of women aged 18–23, 45–50 and 70–75 years at baseline in 1996. Women were randomly selected from the National Medicare Health Insurance Database, which covers all Australian citizens and permanent residents. Full details of the study design, recruitment methods and responses have been published previously.25 26
For the current study, we focused on 13 714 women aged 45–50 years (also known as the 1946–1951 cohort) in 1996 and followed up with self-administered questionnaires eight times, approximately every 3 years, to 2016. Women were excluded if they (a) did not report chronic condition status at baseline, (b) had prior chronic conditions, (c) had missing data on the five types of social relationship satisfaction during follow-ups, or (d) did not provide a response on exposures and outcomes for at least two consecutive surveys (figure 1).
Figure 1.
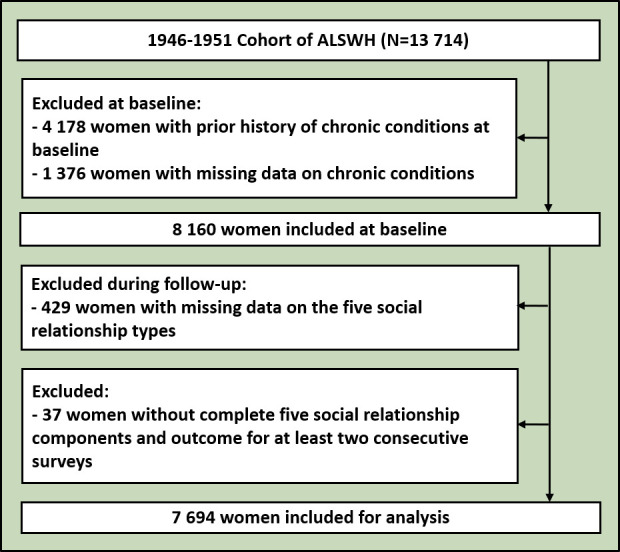
Flowchart of the participant selection. ALSWH, Australian Longitudinal Study on Women’s Health.
Assessment of social relationship satisfaction
Social relationship satisfaction was measured using a multifaceted instrument, covering five types: partners/closest person, family members, friends, work/career/study and social activities. In each survey, women were asked, ‘In general, are you satisfied with what you have achieved in your life so far in the areas of (type)?’. The response for each type was a 4-point Likert scale: ‘very dissatisfied’, ‘dissatisfied’, ‘satisfied’ and ‘very satisfied’. Each type was scored from 0 to 3 to yield a total score of 0–15 to indicate the overall level of social relationship satisfaction. Because of the small number of women with a score of 0–5 (ie, 2.4% at baseline), they were assigned into one group (score ≤5).
Assessment of individual chronic conditions and multimorbidity
The outcome of interest was the accumulation of multimorbidities from a list of 11 conditions: diabetes, hypertension, heart disease, stroke, chronic obstructive pulmonary disease (COPD), asthma, osteoporosis, arthritis, cancer, depression and anxiety. A systematic review suggested that these conditions are commonly chosen for multimorbidity studies.2 These 11 conditions have also been identified as National Health Priority Areas in Australia.27 Previous studies have validated many chronic conditions (ie, diabetes, cancer, heart disease, stroke, COPD, osteoporosis and arthritis) in ALSWH with moderate to good agreement between women’s self-reported diagnosis and hospital records or registry data.28–30
We defined the incidence of a condition as the first survey in which it was reported. We defined the accumulation of multimorbidity when two or more conditions were reported or when additional conditions were reported among women who already had multimorbidity. Accumulation occurred in three ways: zero to two or more, one to two or more, or additional condition(s) from two or more.
Assessment of covariates
Four groups of covariates were used in the analysis and collected at each survey unless indicated otherwise. The covariates included were as follows: two study design variables (age at baseline and survey period (surveys 1–8)), five sociodemographic factors (country of birth, marital status, area of residence, education and ability to manage income), four lifestyle factors (body mass index (BMI), physical activity, alcohol intake and smoking) and menopausal status. All covariates were time-varying, except for the country of birth and education. The definition of each covariate is presented in online supplemental table 1.
gpsych-2022-100925supp001.pdf (1.5MB, pdf)
Statistical analysis
Descriptive analyses were conducted according to the number of chronic conditions developed during 20 years of follow-up. Differences among groups were examined using t-tests or χ2 tests. We then described the overall social relationship satisfaction scores across surveys 1–8 in a Sankey diagram. We also compared the percentage of women reporting multimorbidity based on their previous survey’s social relationship satisfaction score.
Three sets of analyses were performed. First, we established two models to estimate the association between the overall social relationship satisfaction score and the accumulation of multimorbidity. Model 1 (age-adjusted and survey period-adjusted model) was adjusted for age at baseline and survey period. Model 2 (fully adjusted model) was adjusted for age at baseline, survey period, socioeconomic status, health behaviours and menopausal status. Second, we established a series of models to estimate the association between the level of satisfaction in each social relationship satisfaction type and the accumulation of multimorbidity. Third, we estimated the association between the social relationship satisfaction score and the incidence of each chronic condition.
To assess the extent of collinearity between the five social relationship types, we calculated the percent attenuation of the β coefficient for each type after the inclusion of each other type individually and simultaneously in the age-adjusted and survey period-adjusted model: 100×(βModel−βModel+other type (s))/(βModel).31 The same method was used to estimate the contribution of other risk factors to explain the association between the overall social relationship satisfaction score and the accumulation of multimorbidity.
All models were fitted using the accumulation of multimorbidity (or the incidence of each chronic condition) in each survey (surveys 2–8) as the outcome variable and social relationship satisfaction scores in the previous survey (surveys 1–7) as the exposure of interest, with the reference group being women who developed no or one chronic condition only. Logistic regression for repeated measures was used to calculate odds ratios (ORs) with 95% confidence intervals (CIs) using generalised estimating equations.
Sensitivity analyses were also conducted to examine the robustness of the findings under various conditions. First, we tested for a linear trend between social relationship satisfaction and the accumulation of multimorbidity by including the overall satisfaction score as a continuous variable. In addition, we reran model 2 (fully adjusted) using (1) complete case data (ie, only data from women who responded to all eight surveys), (2) satisfaction scores at baseline only, and (3) a multinomial logistic model of the incidence of one condition and the accumulation of multimorbidity with women having no conditions as the reference group.
All analyses were performed using SAS (V.9.4, SAS Institute). All statistical tests were two-sided, and p<0.05 was considered statistically significant.
Results
Characteristics of participants
The final sample comprised 7 694 women (figure 1). There were some baseline differences between the included and excluded women. The excluded women were more likely to have a lower education level, have difficulty managing their available income, be obese, be smokers and have surgical menopause (online supplemental table 2).
Over 20 years, 58.3% of the women (n=4 484) have developed multimorbidity. Women developing multimorbidity were more likely to have a lower education level, have difficulty managing their available income, be overweight or obese, have low levels of physical activity, be smokers and have surgical menopause (table 1).
Table 1.
Baseline characteristics according to the number of chronic conditions accumulated during 20 years of follow-up, ALSWH, 1996 (n=7 694)
| Characteristic | Number of chronic conditions | Statistics (t/χ2) |
P value* | |
| 0 or 1 (n=3 210) | ≥2 (n=4 484) | |||
| Overall satisfaction score, mean(SD) | 11.2 (2.4) | 10.7 (2.5) | 8.560 | <0.001 |
| Age at baseline, mean(SD) | 47.5 (1.5) | 47.6 (1.5) | 3.920 | <0.001 |
| Area of residence, n(%) | 10.540 | 0.015 | ||
| Major cities | 1 202 (37.4) | 1 600 (35.7) | ||
| Inner regions | 1 179 (36.7) | 1 799 (40.1) | ||
| Outer regions | 654 (20.4) | 881 (19.6) | ||
| Remote/very remote | 174 (5.4) | 204 (4.5) | ||
| Marital status, n(%) | 10.955 | 0.004 | ||
| Married | 2 781 (86.6) | 3 782 (84.3) | ||
| Separated/divorced/widowed | 327 (10.2) | 567 (12.6) | ||
| Single | 90 (2.8) | 121 (2.7) | ||
| Education, n(%) | 29.684 | <0.001 | ||
| University/higher degree | 489 (15.2) | 609 (13.6) | ||
| Trade/apprenticeship/diploma | 628 (19.6) | 922 (20.6) | ||
| High school certificate | 613 (19.1) | 679 (15.1) | ||
| No qualifications | 1 458 (45.4) | 2 237 (49.9) | ||
| Country of birth, n(%) | 4.348 | 0.037 | ||
| Australia | 2 386 (74.3) | 3 414 (76.1) | ||
| Outside Australia | 796 (24.8) | 1 017 (22.7) | ||
| Ability to manage income, n(%) | 66.094 | <0.001 | ||
| Easy/not bad | 2 088 (65.0) | 2 511 (56.0) | ||
| Sometimes difficult | 807 (25.1) | 1 272 (28.4) | ||
| Impossible/always difficult | 302 (9.4) | 647 (14.4) | ||
| BMI categories, n(%) | 175.549 | <0.001 | ||
| Underweight (<18.5 kg/m2) | 55 (1.7) | 64 (1.4) | ||
| Normal weight (18.5–24.9 kg/m2) | 1 889 (58.8) | 2 080 (46.4) | ||
| Overweight (25–29.9 kg/m2) | 833 (26.0) | 1 304 (29.1) | ||
| Obese (30–35 kg/m2) | 326 (10.2) | 891 (19.9) | ||
| Physical activity, n(%) | 23.235 | <0.001 | ||
| High (≥1200 MET min/week) | 591 (18.4) | 687 (15.3) | ||
| Moderate (600–1199 MET min/week) | 873 (27.2) | 1 133 (25.3) | ||
| Low (40–599 MET min/week) | 962 (30.0) | 1 384 (30.9) | ||
| Nil/sedentary (0–39 MET min/week) | 761 (23.7) | 1 249 (27.9) | ||
| Alcohol intake, n(%) | 16.745 | <0.001 | ||
| Low risk | 1 679 (52.3) | 2 215 (49.4) | ||
| None/rarely | 1 363 (42.5) | 1 994 (44.5) | ||
| Risky | 125 (3.9) | 249 (5.6) | ||
| Smoking status, n(%) | 14.645 | <0.001 | ||
| Never | 1 789 (55.7) | 2 336 (52.1) | ||
| Former smoker | 863 (26.9) | 1 253 (27.9) | ||
| Current | 461 (14.4) | 772 (17.2) | ||
| Menopausal status, n(%) | 126.538 | <0.001 | ||
| Surgical menopause | 497 (15.5) | 1 057 (23.6) | ||
| Hormone use | 439 (13.7) | 680 (15.2) | ||
| Pre-menopausal | 1 365 (42.5) | 1 477 (32.9) | ||
| Peri-menopausal | 726 (22.6) | 1 043 (23.3) | ||
| Post-menopausal | 175 (5.5) | 218 (4.9) | ||
Data are presented as n (%) or the mean (SD). The column number may not be equal to n because of missing data.
*Independent-samples t-test was used for continuous variables (age), and χ2 tests were used for categorical variables.
ALSWH, Australian Longitudinal Study on Women’s Health; BMI, body mass index; MET, metabolic equivalent of task.
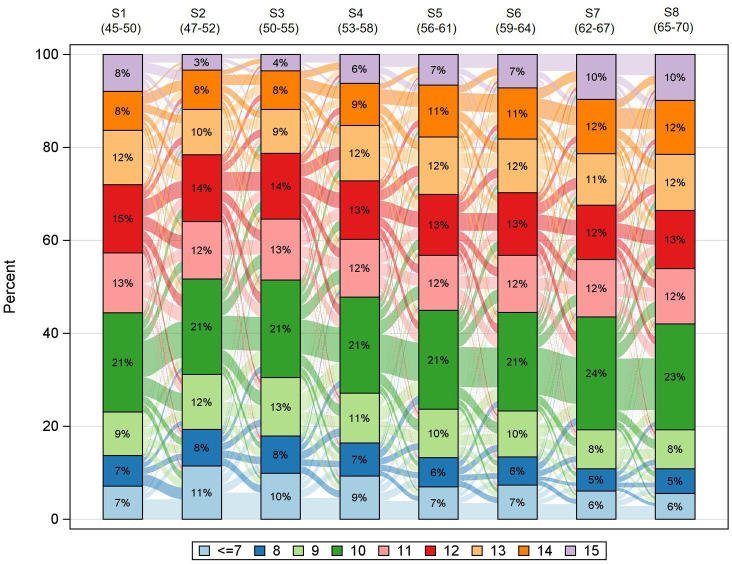
Longitudinal changes of social relationship satisfaction and multimorbidity
The percentage of women in each individual and the overall satisfaction category/score was relatively stable across the surveys (online supplemental figure 1). However, we found substantial transitions across the different satisfaction categories and scores. For example, more than half of the women changed their scores between the surveys (figure 2).
Figure 2.
Longitudinal transitions of women in different social relationship satisfaction scores. The bars with different colours show the distribution of social relationship satisfaction scores in each survey, and the links between bars show the flow from one category to another. Because the SAS procedure for this Sankey diagram cannot handle massive links between all categories, women with scores ≤7 were combined into one category.
The accumulation of multimorbidity according to social relationship satisfaction
Although multimorbidity prevalence increased markedly among all women over 20 years, there was a tendency for women with a lower score to have a higher multimorbidity prevalence (online supplemental table 3). Overall, social relationship satisfaction had a dose–response relationship with the accumulation of multimorbidity in both age-adjusted and survey period-adjusted and fully adjusted models (figure 3 and online supplemental table 4). Compared with women reporting the highest level of satisfaction (score 15, ‘very satisfied’ with all types), women with a score lower than 14 experienced higher odds of accumulating multimorbidity (p<0.05). Particularly, women with the lowest level of satisfaction (score ≤5) had the highest odds of accumulating multimorbidity in the fully adjusted models (OR=2.35, 95% CI: 1.94 to 2.83). The strength of the association was comparable with those of the well-established non-communicable disease risk factors (ie, overweight and obesity, physical inactivity, smoking and alcohol intake) in the same analytical model (online supplemental table 4).
Figure 3.
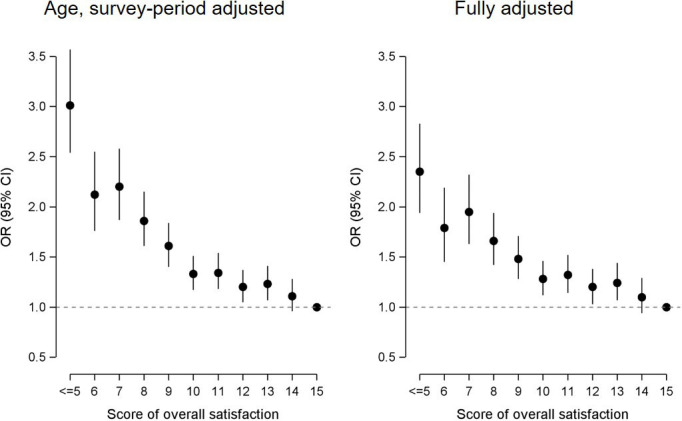
Dose–response relationship between the overall social relationship satisfaction score and the accumulation of multimorbidity in age-adjusted and survey period-adjusted and fully adjusted models (n=7694). The age-adjusted and survey period-adjusted model was adjusted for age at baseline and surveys, while the fully adjusted model was adjusted for age, surveys, socioeconomic status, health behaviours and menopausal status. The results were estimated using the accumulation of multimorbidity in each survey (surveys 2–8) regressed on social relationship satisfaction scores in previous surveys (surveys 1–7), with reference to women who developed no or one condition only. Solid circles represent ORs, and vertical lines represent 95% CIs, with a score of 15 as the reference category. The dashed grey horizontal line represents an OR of 1. A score of overall satisfaction was constructed from the five social relationship satisfaction components (partners/closest person, family members, friends, work/career/study and social activities). OR, odds ratio; CI, confidence interval.
Similar results were observed for each social relationship type in separate models (table 2, models 1a–e and models 2a–e). Compared with women who were very satisfied, those who were very dissatisfied had approximately two times higher odds of accumulating multimorbidity in each of the five types. When all five types were included in the same model, the association between each type and multimorbidity accumulation was attenuated but remained significant for all except friendships (table 2, model 3). Similar results were observed for the individual conditions. For example, women who scored ≤5 had the highest odds of developing most of the 11 conditions, except hypertension, compared with women who scored 15 (online supplemental figure 2). There were no interactions between the two social relationship types (Pinteraction: 0.226–0.970). However, the association between each type and the accumulation of multimorbidity was attenuated when the other types were added to the model individually and simultaneously (online supplemental table 5).
Table 2.
Associations (ORs and 95% CIs) between satisfaction with each social relationship type and the accumulation of multimorbidity (n=7694)
| Very satisfied | Satisfied OR (95% CI) |
Dissatisfied OR (95% CI) |
Very dissatisfied OR (95% CI) |
|
| Models 1a–e (age and survey period adjusted) | ||||
| Partner/closest person | Ref | 1.13 (1.07 to 1.20) | 1.50 (1.38 to 1.63) | 1.95 (1.73 to 2.20) |
| Family members | Ref | 1.15 (1.09 to 1.22) | 1.76 (1.60 to 1.94) | 2.36 (1.93 to 2.88) |
| Friends | Ref | 1.12 (1.06 to 1.19) | 1.63 (1.46 to 1.82) | 2.33 (1.85 to 2.94) |
| Work/career/study | Ref | 1.11 (1.03 to 1.19) | 1.44 (1.32 to 1.57) | 2.11 (1.80 to 2.48) |
| Social activities | Ref | 1.16 (1.09 to 1.24) | 1.79 (1.63 to 1.96) | 2.66 (2.24 to 3.16) |
| Models 2a–e (adjusted for age, survey period, SES, health behaviours and menopausal status) | ||||
| Partner/closest person | Ref | 1.09 (1.02 to 1.16) | 1.35 (1.22 to 1.48) | 1.63 (1.42 to 1.88) |
| Family members | Ref | 1.11 (1.05 to 1.18) | 1.52 (1.37 to 1.68) | 1.84 (1.47 to 2.31) |
| Friends | Ref | 1.10 (1.03 to 1.16) | 1.46 (1.30 to 1.65) | 1.88 (1.45 to 2.43) |
| Work/career/study | Ref | 1.10 (1.02 to 1.20) | 1.33 (1.21 to 1.46) | 1.66 (1.38 to 1.98) |
| Social activities | Ref | 1.14 (1.06 to 1.22) | 1.56 (1.41 to 1.72) | 2.13 (1.76 to 2.58) |
| Model 3 (fully adjusted) | ||||
| Partner/closest person | Ref | 1.01 (0.93 to 1.09) | 1.09 (0.98 to 1.22) | 1.19 (1.00 to 1.40) |
| Family members | Ref | 1.04 (0.97 to 1.12) | 1.26 (1.11 to 1.42) | 1.37 (1.05 to 1.79) |
| Friends | Ref | 0.97 (0.89 to 1.05) | 0.97 (0.84 to 1.13) | 0.87 (0.61 to 1.24) |
| Work/career/study | Ref | 1.07 (0.98 to 1.17) | 1.19 (1.07 to 1.32) | 1.26 (1.04 to 1.54) |
| Social activities | Ref | 1.09 (0.99 to 1.19) | 1.37 (1.20 to 1.56) | 1.73 (1.33 to 2.25) |
Models 1a–e are five separate models for each social relationship adjusted for age and survey variables. Models 2a–e are five separate models for each social relationship adjusted for age, survey period, SES, health behaviours and menopausal variables. Model 3 includes all five social relationship types in one model, adjusted for age, survey period, SES, health behaviours and menopausal variables.
CI, confidence interval; OR, odds ratio; Ref, reference; SES, socioeconomic status.
Roles of socioeconomic status, health behaviours and menopausal status
Table 3 shows the relative contributions of other risk factors. All the risk factors combined explained 22.72% of the association between overall social relationship satisfaction and the accumulation of multimorbidity, with most of the contribution being from the ability to manage income (18.32%). The four major behavioural factors accounted for 7.37% of the association.
Table 3.
Roles of SES, health behaviours and menopausal status in attenuating the association between the overall social relationship satisfaction and the accumulation of multimorbidity (n=7694)
| OR (95% CI)* | % attenuation† | |
| Model 1 (adjusted for age and survey period) | 3.01 (2.54 to 3.57) | NA |
| Model 1+marital status | 2.95 (2.48 to 3.50) | 2.07 |
| Model 1+area of residence | 3.00 (2.54 to 3.56) | 0.31 |
| Model 1+education | 2.94 (2.48 to 3.49) | 2.16 |
| Model 1+country of birth | 3.08 (2.59 to 3.65) | −1.81 |
| Model 1+ability to manage income | 2.46 (2.07 to 2.92) | 18.32 |
| Model 1+all 5 social economic status variables | 2.45 (2.05 to 2.92) | 18.93 |
| Model 1+body mass index | 2.92 (2.45 to 3.47) | 3.02 |
| Model 1+physical activity | 3.01 (2.52 to 3.59) | 0.24 |
| Model 1+drinking status | 2.99 (2.52 to 3.54) | 0.78 |
| Model 1+smoking status | 2.91 (2.46 to 3.44) | 3.26 |
| Model 1+all 4 behaviour variables | 2.78 (2.32 to 3.33) | 7.37 |
| Model 1+menopausal status | 3.02 (2.54 to 3.57) | −0.05 |
| Model 1+all variables | 2.35 (1.94 to 2.83) | 22.72 |
*ORs are for women reporting the highest score of overall social relationship satisfaction (15) compared with women reporting the lowest scores (≤5).
†Percentage of attenuation in log OR=100×(βModel 1−βModel 1+SES, health behaviours and menopausal status)/(βModel 1).
CI, confidence interval; NA, not available; OR, odds ratio; SES, socioeconomic status.
Sensitivity analysis
The sensitivity analyses, in which we used complete case data or satisfaction scores at baseline only, provided similar results to those of the primary analysis (online supplemental tables 6 and 7). Similar results were also obtained in multinomial outcome analyses (0, 1, 2 or more). Slightly higher odds of accumulating multimorbidity were noted compared with the results using binomial outcomes (0, 1, 2 or more) (online supplemental table 8). When the satisfaction score was treated as a continuous variable, a one-score decrease was associated with 7% (95% CI: 6% to 9%) higher odds of accumulating multimorbidity.
Discussion
Main findings
In this large national population-based cohort study of women in their midlife to early old age, taking several well-established risk factors into account, we observed a dose–response increasing odds of accumulating multimorbidity in relation to satisfaction with a range of relationship types as well as overall satisfaction with social relationships. In addition, well-established risk factors, such as socioeconomic status, health behaviours and menopausal status, together explained less than one-fifth of the association.
Interpretations and implications
To the best of our knowledge, this study is the first to provide compelling evidence on the association between satisfaction with individual social relationship types and their combination with the accumulation of multimorbidity. No previous study has examined these associations using longitudinal data. However, our findings on the associations between some types of social relationship satisfaction and individual chronic conditions (eg, depression, hypertension, cardiovascular disease and cancer) are similar to those observed in previous research.10–12 21 32 33 Further research is needed to explore other dimension-specific effects of social relationships on multimorbidity, such as the qualitative dimension (eg, intimacy), structure dimension (eg, quantity) and function dimension (eg, emotional and practical support), which were not addressed in this study. The current findings provide at least three unique and important inferences.
First, the present study confirms and extends previous research on social relationships and health-related outcomes (eg, chronic conditions) by quantifying the dose–response relationship. The results were robust across many analyses: when considering the exposure both as time-varying and at baseline only, examining the effects of both individual types and when combined, controlling for well-established risk factors, and considering the outcome as both the number of chronic conditions and each condition separately. In addition, the attenuated associations between social relationships and multimorbidity accumulation after adjusting for behaviours supported behaviours as a potential mediator in the underlying mechanism. Although we cannot conclude that social relationship satisfaction is a causal factor, given that all participants were disease-free at baseline and that there is a temporal sequence between the exposure and outcome, our findings advance the understanding of the association between social relationship satisfaction and the development of chronic conditions.
Second, we demonstrated the association between several different types of satisfaction and the accumulation of multimorbidity using a multivariable analysis strategy.22 We found that the association between each type and the accumulation of multimorbidity was attenuated when we added the other types to the model individually and then simultaneously but remained significant for all types except friendships. These findings suggest that engagement in diverse social relationships might be a promising approach for preventing or slowing the accumulation of multimorbidity.
Third, in the models controlling for all other risk factors, we found that the strength of the association was comparable with or even higher than well-established risk factors (eg, obesity and physical activity). Moreover, we did not find that these risk factors largely mitigated the likelihood of accumulating multimorbidity. This finding suggests that the majority of the observed relationship between social relationship satisfaction and accumulating multimorbidity may be explained by other factors (eg, psychological mechanisms) and that social relationship satisfaction itself may be a strong and dominant predictor of accumulating multimorbidity.
Our findings have significant implications for chronic disease management and intervention at both individual and population levels. First, at the individual level, these implications may help counsel women regarding the benefits of starting or maintaining high-quality and diverse social relationships throughout middle to early old age. For example, asking patients about the subjective ratings of their social relationships could be a priority in clinical practice.32 Second, at the community level, interventions focusing on social relationship satisfaction or quality may be particularly efficient in preventing the progression of chronic conditions.34 35 Third, at the country and global levels, social connections (eg, social relationship satisfaction) should be considered a public health priority in chronic disease prevention and intervention. Although some countries, for example, the UK, have appointed a Minister for Loneliness to develop national strategies around social relationships and health,36 global health strategies have not considered poor social connections as risk factors in the prevention and control of chronic conditions (eg, WHO, 25×25 risk factors).37
Plausible mechanisms
Multiple inter-related pathways have been proposed to explain the association between social relationships and health-related outcomes, with the prominent mechanisms being health behaviours (eg, physical activity and nutrition) and biological and psychosocial factors (direct effects on surrogate biological markers).6 22 38–41 Additionally, social relationships may influence healthcare-seeking behaviours and health service use. A recent study showed that individuals with poor social connectedness appear to be at a greater risk of not engaging in the full range of preventive services than individuals with good social connectedness.42 In addition, mental disturbances, including depression, might also influence social relationship satisfaction and consequently influence the accumulation of multimorbidities.43 Lastly, given that well-established risk factors only contribute to a small part of the association between social relationship satisfaction and multimorbidity, other mechanisms (eg, social relationship satisfaction itself) may be involved.
Limitations
A key limitation of this study is that chronic conditions are based on self-reported data and are thus susceptible to reporting errors. However, previous studies on ALSWH have demonstrated the validity of most chronic conditions and other covariates. For example, self-reported diabetes, heart disease and stroke were validated using hospital data in women hospitalised in New South Wales, Australia.44 The prevalence and bias-adjusted κ values for the three conditions were 0.93, 0.91 and 0.98, respectively. Cancer information has been validated against Cancer Registry data with 89% sensitivity and 97% specificity.45 Additionally, we did not capture the past social relationships of the participants in early adulthood. In addition, unmeasured confounding factors (eg, personality and mental disturbances) may have biased the research findings. Finally, all the participants were Australian women, which limits the generalisability of the results. Given that previous studies have suggested that the effects of social relationships on health-related outcomes are different for men and women,46 further large population-based studies are warranted to investigate the role of social relationships in the accumulation of multimorbidities.
Implications
We have demonstrated a dose–response relationship between social relationship satisfaction and the accumulation of multimorbidity from midlife to early old age, which was only partly explained by socioeconomic, behavioural and reproductive factors. Social connections (eg, social relationship satisfaction) should be considered a public health priority in chronic disease prevention and intervention.
Biography
Dr Xiaolin Xu is currently a Research Professor (hundred talents program) at the School of Public Health and the Second Affiliated Hospital School of Medicine, Zhejiang University in China. He is also an adjunct research fellow at the School of Public Health of The University of Queensland in Australia. This study was part of his doctoral program. He was formerly a research assistant at the Global Health Research Center of Duke Kunshan University in China. He also worked and interned at a healthcare consulting company in Shanghai and London and the headquarters of the World Health Organization in Geneva. His research interests include the epidemiology and prevention of multiple risk factors and chronic conditions (multimorbidity) using life-course approaches, the promotion of women’s health, and the implications of big data in clinical and public health practice. He received funding from national and international agencies, including the China Medical Board and Bill & Melinda Gates Foundation, to support his research.
Footnotes
Contributors: XX and GDM contributed to the design of the study. XX conducted the data analysis. XX, GDM and MJ performed the interpretation of the data. XX drafted the manuscript. XX was responsible for the overall content as the guarantor. XX, MJ, GDM and JH-L revised the article and approved the final version to be published.
Funding: This study was funded by Universities of Queensland and Newcastle, National Health and Medical Research Council Principal Research Fellowship (grant number: APP1121844), and the University of Queensland, Australian Government Department of Health.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study has current ethical approval from Human Research Ethics Committees at the Universities of Newcastle (Newcastle, New South Wales, Australia) and Queensland (Brisbane, Queensland, Australia). Participants gave informed consent to participate in the study before taking part.
References
- 1. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet 2017;390:1211–59. 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: an overview of systematic reviews. Ageing Res Rev 2017;37:53–68. 10.1016/j.arr.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 3. Academy of Medical Sciences . Multimorbidity: a priority for global health research. London: Academy of Medical Sciences, 2018. [Google Scholar]
- 4. Salisbury C, Man M-S, Bower P, et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet 2018;392:41–50. 10.1016/S0140-6736(18)31308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ong BN, Richardson JC, Porter T, et al. Exploring the relationship between multi-morbidity, resilience and social connectedness across the lifecourse. Health 2014;18:302–18. 10.1177/1363459313497609 [DOI] [PubMed] [Google Scholar]
- 6. Holt-Lunstad J, Robles TF, Sbarra DA. Advancing social connection as a public health priority in the United States. Am Psychol 2017;72:517–30. 10.1037/amp0000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Holt-Lunstad J. Why social relationships are important for physical health: a systems approach to understanding and modifying risk and protection. Annu Rev Psychol 2018;69:437–58. 10.1146/annurev-psych-122216-011902 [DOI] [PubMed] [Google Scholar]
- 8. Song L, Pettis PJ, Chen Y, et al. Social cost and health: the downside of social relationships and social networks. J Health Soc Behav 2021;62:371–87. 10.1177/00221465211029353 [DOI] [PubMed] [Google Scholar]
- 9. Uchino BN, Eisenberger NI. Emotions in social relationships and their implications for health and disease: introduction to the special issue of psychosomatic medicine. Psychosom Med 2019;81:676–80. 10.1097/PSY.0000000000000741 [DOI] [PubMed] [Google Scholar]
- 10. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med 2010;7:e1000316. 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Valtorta NK, Kanaan M, Gilbody S, et al. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 2016;102:1009–16. 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Youm Y, Baldina E, Baek J. All-cause mortality and three aspects of social relationships: an eight-year follow-up of older adults from one entire Korean village. Sci Rep 2021;11:465. 10.1038/s41598-020-80684-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stickley A, Koyanagi A. Physical multimorbidity and loneliness: a population-based study. PLoS One 2018;13:e0191651. 10.1371/journal.pone.0191651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ma R, Romano E, Vancampfort D, et al. Physical multimorbidity and social participation in adult aged 65 years and older from six low- and middle-income countries. J Gerontol B Psychol Sci Soc Sci 2021;76:1452–62. 10.1093/geronb/gbab056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hülür G. Structural and functional aspects of social relationships and episodic memory: between-person and within-person associations in middle-aged and older adults. Gerontology 2022;68:86–97. 10.1159/000514949 [DOI] [PubMed] [Google Scholar]
- 16. Whisman MA, Gilmour AL, Salinger JM. Marital satisfaction and mortality in the United States adult population. Health Psychol 2018;37:1041–4. 10.1037/hea0000677 [DOI] [PubMed] [Google Scholar]
- 17. Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: a meta-analysis. Occup Environ Med 2005;62:105–12. 10.1136/oem.2002.006734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fancourt D, Steptoe A. Community group membership and multidimensional subjective well-being in older age. J Epidemiol Community Health 2018;72:376–82. 10.1136/jech-2017-210260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cundiff JM, Matthews KA. Friends with health benefits: the long-term benefits of early peer social integration for blood pressure and obesity in midlife. Psychol Sci 2018;29:814–23. 10.1177/0956797617746510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dirlam J, Zheng H. Job satisfaction developmental trajectories and health: a life course perspective. Soc Sci Med 2017;178:95–103. 10.1016/j.socscimed.2017.01.040 [DOI] [PubMed] [Google Scholar]
- 21. Ryu E, Jenkins GD, Wang Y, et al. The importance of social activity to risk of major depression in older adults. Psychol Med 2021;2:1–9. 10.1017/S0033291721004566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Saito T, Murata C, Saito M, et al. Influence of social relationship domains and their combinations on incident dementia: a prospective cohort study. J Epidemiol Community Health 2018;72:7–12. 10.1136/jech-2017-209811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. MacNeil-Vroomen J, Schulz R, Doyle M, et al. Time-varying social support and time to death in the cardiovascular health study. Health Psychol 2018;37:1000–5. 10.1037/hea0000660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Martire LM, Franks MM. The role of social networks in adult health: introduction to the special issue. Health Psychol 2014;33:501–4. 10.1037/hea0000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee C, Dobson AJ, Brown WJ, et al. Cohort profile: the Australian longitudinal study on women's health. Int J Epidemiol 2005;34:987–91. 10.1093/ije/dyi098 [DOI] [PubMed] [Google Scholar]
- 26. Dobson AJ, Hockey R, Brown WJ, et al. Cohort profile update: Australian longitudinal study on women's health. Int J Epidemiol 2015;44:1547–1547f. 10.1093/ije/dyv110 [DOI] [PubMed] [Google Scholar]
- 27. Australian Institute of Health and Welfare . The National health priority areas, 2012. [Google Scholar]
- 28. Lazarevic N, Dobson AJ, Barnett AG, et al. Long-term ambient air pollution exposure and self-reported morbidity in the Australian longitudinal study on women's health: a cross-sectional study. BMJ Open 2015;5:e008714. 10.1136/bmjopen-2015-008714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Peeters GMEE, Tett SE, Dobson AJ, et al. Validity of self-reported osteoporosis in mid-age and older women. Osteoporos Int 2013;24:917–27. 10.1007/s00198-012-2033-7 [DOI] [PubMed] [Google Scholar]
- 30. Parkinson L, Curryer C, Gibberd A, et al. Good agreement between self-report and centralized hospitalizations data for arthritis-related surgeries. J Clin Epidemiol 2013;66:1128–34. 10.1016/j.jclinepi.2013.04.012 [DOI] [PubMed] [Google Scholar]
- 31. Stringhini S, Dugravot A, Shipley M, et al. Health behaviours, socioeconomic status, and mortality: further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Med 2011;8:e1000419. 10.1371/journal.pmed.1000419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Teo AR, Choi H, Valenstein M. Social relationships and depression: ten-year follow-up from a nationally representative study. PLoS One 2013;8:e62396. 10.1371/journal.pone.0062396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yang YC, Boen C, Mullan Harris K. Social relationships and hypertension in late life: evidence from a nationally representative longitudinal study of older adults. J Aging Health 2015;27:403–31. 10.1177/0898264314551172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Santini ZI, Fiori KL, Feeney J, et al. Social relationships, loneliness, and mental health among older men and women in Ireland: a prospective community-based study. J Affect Disord 2016;204:59–69. 10.1016/j.jad.2016.06.032 [DOI] [PubMed] [Google Scholar]
- 35. LeBlanc RG, Chiodo L, Jacelon CS. Social relationship influence on self-care and health among older people living with long term conditions: a mixed-methods study. Int J Older People Nurs 2022;17:e12450. 10.1111/opn.12450 [DOI] [PubMed] [Google Scholar]
- 36. Gulland A. Sixty seconds on… loneliness. BMJ 2018;360:k300. 10.1136/bmj.k300 [DOI] [PubMed] [Google Scholar]
- 37. World Health Organization . Global action plan for the prevention and control of noncommunicable diseases 2013-2020, 2013. [Google Scholar]
- 38. Yang YC, Boen C, Gerken K, et al. Social relationships and physiological determinants of longevity across the human life span. Proc Natl Acad Sci U S A 2016;113:578–83. 10.1073/pnas.1511085112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Holt-Lunstad J, Smith TB. Loneliness and social isolation as risk factors for CVD: implications for evidence-based patient care and scientific inquiry. Heart 2016;102:987–9. 10.1136/heartjnl-2015-309242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Suls J, Green PA, Davidson KW. A biobehavioral framework to address the emerging challenge of multimorbidity. Psychosom Med 2016;78:281–9. 10.1097/PSY.0000000000000294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Guthrie TD, Benadjaoud YY, Chavez RS. Social relationship strength modulates the similarity of brain-to-brain representations of group members. Cereb Cortex 2022;32:2469–77. 10.1093/cercor/bhab355 [DOI] [PubMed] [Google Scholar]
- 42. Stafford M, von Wagner C, Perman S, et al. Social connectedness and engagement in preventive health services: an analysis of data from a prospective cohort study. Lancet Public Health 2018;3:e438–46. 10.1016/S2468-2667(18)30141-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Campbell D, Green MJ, Davies N, et al. Effects of depression on employment and social outcomes: a Mendelian randomisation study. J Epidemiol Community Health 2022;76:563–71. 10.1136/jech-2021-218074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Navin Cristina TJ, Stewart Williams JA, Parkinson L, et al. Identification of diabetes, heart disease, hypertension and stroke in mid- and older-aged women: comparing self-report and administrative hospital data records. Geriatr Gerontol Int 2016;16:95–102. 10.1111/ggi.12442 [DOI] [PubMed] [Google Scholar]
- 45. Stavrou E, Vajdic CM, Loxton D, et al. The validity of self-reported cancer diagnoses and factors associated with accurate reporting in a cohort of older Australian women. Cancer Epidemiol 2011;35:e75–80. 10.1016/j.canep.2011.02.005 [DOI] [PubMed] [Google Scholar]
- 46. Ang S. Social participation and health over the adult life course: does the association strengthen with age? Soc Sci Med 2018;206:51–9. 10.1016/j.socscimed.2018.03.042 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gpsych-2022-100925supp001.pdf (1.5MB, pdf)
Data Availability Statement
Data are available upon reasonable request.