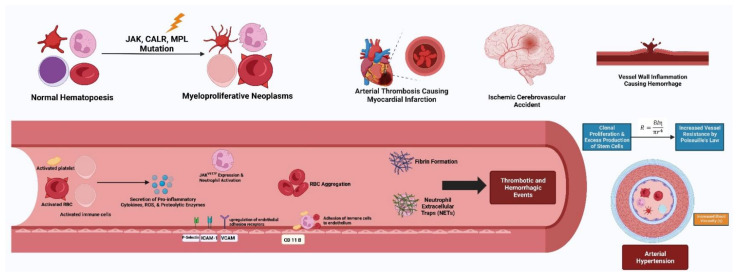
Figure 2.
The pathogenesis of myeloproliferative neoplasms is multifaceted and often includes genetic mutations involving the JAK2, CALR and MPL genes among others. Abnormal clone-derived blood cells (i.e., erythrocytes, platelets and leukocytes) drive prothrombotic features. The secretion of pro-inflammatory cytokines and reactive oxygen species disrupts normal endothelial function and leads to increased expression of endothelial adhesion receptors. The release of tissue factor from activated platelets aids in the formation of fibrin clots and DNA released from activated neutrophils forms neutrophil-extracellular traps (NETs). Additionally, red blood cell (RBC) aggregation occurs through biochemical changes in the RBC membrane. The culmination of these maladaptive events causes increased blood viscosity, vascular resistance and arterial hypertension through Poiseuille’s law.