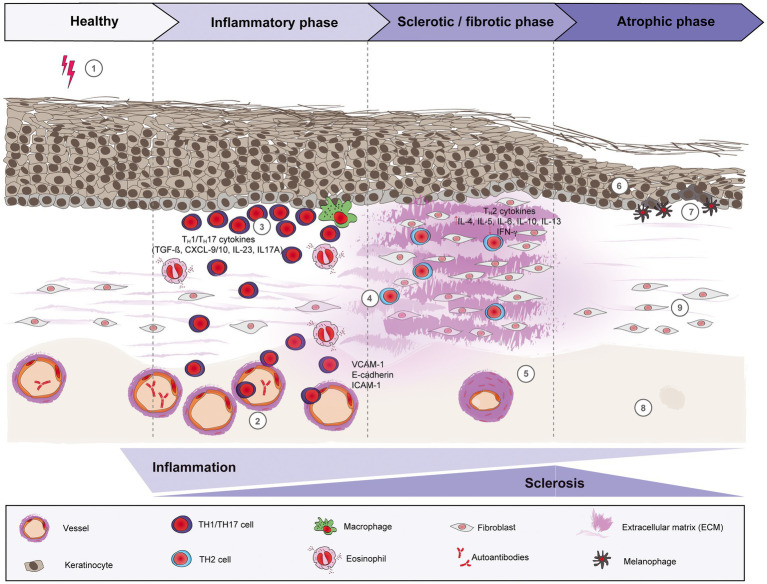
Figure 1.
Schematic overview of morphea pathogenesis. Based on current evidence, the pathogenesis of morphea can be divided into three distinct phases: early inflammatory, sclerotic/fibrotic and late atrophic. Environmental factors like radiation, skin trauma and infections may trigger in genetically predisposed patients (1) a T cell-driven skin inflammation, but also plasma cells and eosinophils around the vessels, adnexal structures and in the dermis. The resulted intense endothelial damage will lead to the upregulation of adhesion molecules, such as E-cadherin and VCAM-1 during the inflammatory stage (2), which in turn will recruit pro-inflammatory TH1 and TH17 cells and associated cytokines (CXCL-9/10, TGF-ß, IL-23 and IL-17A, respectively) that will activate fibroblasts. (3) Next, a switch towards a predominant TH2-driven response will facilitate the recruitment of T lymphocytes that are capable of producing profibrotic cytokines like IL-4, IL-6 and TGF-ß. (4) Therefore, sclerosis increases with hyalinized, compact collagen bundles in the dermis, with few sweat glands and blood vessels, the latter with thickened walls and narrow lumens. (5) In the last phase, atrophy slowly increases as sclerosis subsides. The epidermis will decrease in thickness (6), while basal keratinocytes display pigment, with the presence of underlying melanophages. (7) There is loss of skin appendages, blood vessels (8) and inflammatory cells (9).