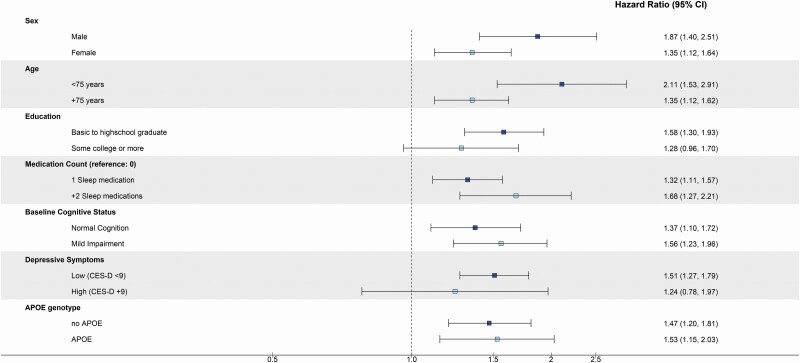
Figure 2.
Adjusted hazard ratios (95% confidence intervals) of incident dementia among late-life sleep medication users, stratified by subgroups, ARIC study (N = 4 197). Sex (n): male (1 235), female (2 962); Age (n): <75 years (2 101), +75 years (2 096); Education: basic to high school (2 390), some college (1 807); Medication count (n): 1 sleep medication (1 107), +2 sleep medications (292); Baseline cognitive status (n): normal cognitive status (3 317), mild cognitive impairment (877); Depressive symptoms (n): CES-D < 9 (3 909), CES-D ≥ 9 (288); APOE ε4 (n): no APOE ε4 (2 940), APOE ε4 (1 083); Interaction p values: sex: p = .16, age: p = .20; Education (basic): p = .09, education (some college): p = .76; Baseline cognitive status: p = .56; Depressive symptoms p = .74; APOE ε4 p = .84. Models adjusted for the following except for the variable stratified on (besides variable stratified on): age, sex, race-center, education, APOE ε4, smoking status, alcohol consumption, depressive symptoms, and BMI. ARIC = Atherosclerosis Risk in Communities; BMI = body mass index; CES-D = Center for Epidemiologic Studies Depression.